-
PDF
- Split View
-
Views
-
Cite
Cite
Sacha F de Stoppelaar, Liza Pereverzeva, Bram Hafkamp, Nikki Lips, Floor Tielbeke, Linde Rustenburg, Caroline Hoogerheide-Wiegerinck, Koen de Heer, Diagnostic Value of Chest X-Ray in Patients With Suspected Infection and No Respiratory Signs or Symptoms, Open Forum Infectious Diseases, Volume 7, Issue 6, June 2020, ofaa221, https://doi.org/10.1093/ofid/ofaa221
Close - Share Icon Share
Abstract
Suspicion of an infection without localizing signs or symptoms is a common problem. A chest x-ray (CXR) is often performed to rule out pneumonia. Our prospective cross-sectional study suggests that a CXR has no diagnostic value in patients without respiratory signs or symptoms, if a reliable medical history can be obtained.
Patients suspected of an infection at the emergency department (ED) often have no localizing signs or symptoms. The sepsis guideline of the National Institute for Health and Care Excellence [1] advises to consider a chest x-ray (CXR) to identify the source of infection. In a recent survey among Dutch internists, 88% reported that they performed a CXR in patients with a suspected infection and no respiratory signs or symptoms [2]. The diagnostic value of a CXR in this situation is unknown, although it increases healthcare cost, waiting times at the ED, and the risk of crowding [3]. We hypothesized that a CXR has no diagnostic value in patients with a suspected infection when no evident extrapulmonary source of infection and no respiratory signs or symptoms are present. We performed a prospective cross-sectional study to test this hypothesis.
METHODS
This cross-sectional study was conducted from April 2017 to May 2018 at the Flevoziekenhuis, Almere, the Netherlands. We prospectively included all adult patients that were referred to the internal medicine emergency department (ED) with a suspected infection, defined as a temperature ≤36.0°C or ≥38.0°C, or a C-reactive protein (CRP) ≥100 µg/L as CRP is a routine test in case of a suspected infection in the Netherlands. Subjects underwent a full medical history and physical examination by the attending physician as well as laboratory tests including a complete blood count and indices, leukocyte differentiation, and CRP. Patients were assessed for an evident extrapulmonary source of infection (excluding bacteriuria or leukocyturia in women without urinary tract symptoms) and for respiratory signs or symptoms of pneumonia: ie, dyspnoea, chest pain, cough, an elevated respiratory rate (>20 per minute), decreased oxygen saturation (<95%), and abnormalities at auscultation. Bacteriuria or leukocyturia in women without a positive urine culture or urinary tract symptoms was not considered an evident extrapulmonary source of infection. Clinical parameters were measured at presentation. The medical history was scored unreliable in case of a confused patient or a patient with a language barrier, cognitive impairment, or verbal response of <5 on the Glasgow Coma Scale (GCS). Experienced radiologists analyzed the CXRs. Pneumonia was radiologically defined as increased attenuation of lung parenchyma without loss of volume in affected segments. A second radiologist confirmed the interpretation of the CXR in the patients without an evident extrapulmonary source of infection and without respiratory signs or symptoms. Attending physicians discussed all cases with their supervisor. Patient follow-up consisted of screening all additional pulmonary imaging for delayed manifestations of pneumonia in admitted patients and urinary cultures in female patients with bacteriuria or leukocyturia. The primary outcome of our study was the number of pneumonia diagnoses that were uncovered by the CXR in patients with a suspected infection, no evident extrapulmonary source of infection, and no respiratory signs or symptoms, and in whom a reliable medical history could be obtained. All data were evaluated using R, version 3.6.1. Between-group differences in continuous non-parametric variables were analyzed using a Mann-Whitney U test; categorical data were examined using a χ 2 test. We calculated the 95% confidence interval (CI) of the primary outcome using the equal-tailed Jeffreys’ prior interval [4, 5]. A secondary analysis was performed in patients without a reliable medical history. Need for informed consent for this study was waived by the Medical Ethics Committee of the Academic Medical Center, Amsterdam (W16_365 no. 16.430).
RESULTS
Of the 2920 patients that presented at the ED during the study period, 741 met the inclusion criteria (Figure 1). Of those 741 patients, 274 had an evident extrapulmonary source of infection and 365 patients had 1 or more of the defined respiratory signs or symptoms. A reliable medical history could be obtained in 70 of the remaining 102 patients, 7 of which were neutropenic. Patient characteristics of patients without respiratory signs or symptoms are shown in Table 1. There was a significant difference in age and GCS between patients with and without reliable medical history. In the 70 patients in whom reliable medical history could be obtained, no pneumonia was diagnosed by CXR (95% CI, 0%–3.51%) (Figure 1 and Table 1). In the 32 patients in whom a reliable medical history was not possible, 5 diagnoses of pneumonia were made by CXR (95% CI, 6%–31%) (Figure 1 and Table 1). There were 2 female patients without evident source of infection that had leukocyturia. They did not use antibiotics at presentation and urinary cultures were negative. Additional pulmonary radiography (4 CXRs and 5 computed tomography scans) was performed in 9 patients because of development of respiratory complaints (3 patients) during hospital admission or persisting unexplained complaints (6 patients). The additional radiography did not lead to a new diagnosis of pneumonia.
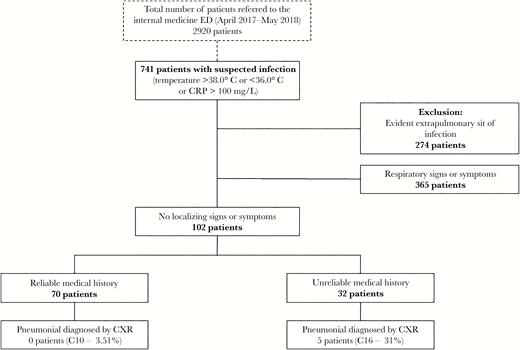
Flow chart. CI, confidence interval; CRP, C-reactive protein; ED, emergency department.
Characteristics of Patients With Suspected Infection Without Localizing Signs or Symptoms
| Characteristics . | Reliable Medical History . | Unreliable Medical History . | P Value . |
|---|---|---|---|
| Patients, n | 70 | 32 | |
| Demographics | |||
| Age, year, median [IQR] | 62 [52–69] | 76 [66–83] | <.01 |
| Sex, male, n (%) | 31 (44) | 19 (59) | .23 |
| Chronic Comorbidity, n (%) | |||
| Asthma | 2 (3) | 1 (3) | 1.00 |
| COPD | 3 (4) | 1 (3) | 1.00 |
| Recent use of antineoplastic drugs | 16 (23) | 1 (3) | .03 |
| Hematologic malignancy | 10 (14) | 0 (0) | .06 |
| Solid tumor | 14 (20) | 4 (13) | .52 |
| Auto immune disease | 1 (1) | 0 (0) | 1.00 |
| Immunosuppressive medication | 4 (6) | 0 (0) | .41 |
| Sickle cell disease | 2 (3) | 0 (0) | .84 |
| Clinical Parameters | |||
| Temperature, n (%) | .15 | ||
| ≤36.0°C | 2 (3) | 4 (13) | |
| 36.0–38.0°C | 22 (31) | 8 (25) | |
| ≥38.0°C | 46 (66) | 20 (63) | |
| CRP ≥100 mg/L, n (%) | 39 (56) | 16 (50) | .75 |
| Heart rate, bpm, median [IQR] | 96 [85–105] | 93 [81–105] | .42 |
| Systolic blood pressure ≤100 mmHg, n (%) | 5 (7) | 5 (16) | .33 |
| GCS <15, n (%) | 2 (3) | 14 (44) | <.01 |
| Respiratory Rate, n (%) | .89 | ||
| <9 breaths/min | 1 (1.6) | 0 (0.0) | |
| 9–14 breaths/min | 24 (38.1) | 11 (36.7) | |
| 15–20 breaths/min | 35 (55.6) | 17 (56.7) | |
| 21–30 breaths/min | 3 (4.8) | 2 (6.7) | |
| Neutrophil count, ×109/L, median [IQR] | 7.3 [5–12] | 9.3 [8–12] | .15 |
| Neutropenia, n (%) | 7 (11) | 0 (0) | .17 |
| Admission to hospital, n (%) | 44 (64) | 23 (72) | .51 |
| Pneumonia on CXR, n (%) | 0 (0) | 5 (16) | <.01 |
| Characteristics . | Reliable Medical History . | Unreliable Medical History . | P Value . |
|---|---|---|---|
| Patients, n | 70 | 32 | |
| Demographics | |||
| Age, year, median [IQR] | 62 [52–69] | 76 [66–83] | <.01 |
| Sex, male, n (%) | 31 (44) | 19 (59) | .23 |
| Chronic Comorbidity, n (%) | |||
| Asthma | 2 (3) | 1 (3) | 1.00 |
| COPD | 3 (4) | 1 (3) | 1.00 |
| Recent use of antineoplastic drugs | 16 (23) | 1 (3) | .03 |
| Hematologic malignancy | 10 (14) | 0 (0) | .06 |
| Solid tumor | 14 (20) | 4 (13) | .52 |
| Auto immune disease | 1 (1) | 0 (0) | 1.00 |
| Immunosuppressive medication | 4 (6) | 0 (0) | .41 |
| Sickle cell disease | 2 (3) | 0 (0) | .84 |
| Clinical Parameters | |||
| Temperature, n (%) | .15 | ||
| ≤36.0°C | 2 (3) | 4 (13) | |
| 36.0–38.0°C | 22 (31) | 8 (25) | |
| ≥38.0°C | 46 (66) | 20 (63) | |
| CRP ≥100 mg/L, n (%) | 39 (56) | 16 (50) | .75 |
| Heart rate, bpm, median [IQR] | 96 [85–105] | 93 [81–105] | .42 |
| Systolic blood pressure ≤100 mmHg, n (%) | 5 (7) | 5 (16) | .33 |
| GCS <15, n (%) | 2 (3) | 14 (44) | <.01 |
| Respiratory Rate, n (%) | .89 | ||
| <9 breaths/min | 1 (1.6) | 0 (0.0) | |
| 9–14 breaths/min | 24 (38.1) | 11 (36.7) | |
| 15–20 breaths/min | 35 (55.6) | 17 (56.7) | |
| 21–30 breaths/min | 3 (4.8) | 2 (6.7) | |
| Neutrophil count, ×109/L, median [IQR] | 7.3 [5–12] | 9.3 [8–12] | .15 |
| Neutropenia, n (%) | 7 (11) | 0 (0) | .17 |
| Admission to hospital, n (%) | 44 (64) | 23 (72) | .51 |
| Pneumonia on CXR, n (%) | 0 (0) | 5 (16) | <.01 |
Abbreviations: bpm, beats per minute; COPD, chronic obstructive pulmonary disease; CRP, C-reactive protein; CXR, chest x-ray; GCS Glasgow Coma Scale; IQR, interquartile range.
Characteristics of Patients With Suspected Infection Without Localizing Signs or Symptoms
| Characteristics . | Reliable Medical History . | Unreliable Medical History . | P Value . |
|---|---|---|---|
| Patients, n | 70 | 32 | |
| Demographics | |||
| Age, year, median [IQR] | 62 [52–69] | 76 [66–83] | <.01 |
| Sex, male, n (%) | 31 (44) | 19 (59) | .23 |
| Chronic Comorbidity, n (%) | |||
| Asthma | 2 (3) | 1 (3) | 1.00 |
| COPD | 3 (4) | 1 (3) | 1.00 |
| Recent use of antineoplastic drugs | 16 (23) | 1 (3) | .03 |
| Hematologic malignancy | 10 (14) | 0 (0) | .06 |
| Solid tumor | 14 (20) | 4 (13) | .52 |
| Auto immune disease | 1 (1) | 0 (0) | 1.00 |
| Immunosuppressive medication | 4 (6) | 0 (0) | .41 |
| Sickle cell disease | 2 (3) | 0 (0) | .84 |
| Clinical Parameters | |||
| Temperature, n (%) | .15 | ||
| ≤36.0°C | 2 (3) | 4 (13) | |
| 36.0–38.0°C | 22 (31) | 8 (25) | |
| ≥38.0°C | 46 (66) | 20 (63) | |
| CRP ≥100 mg/L, n (%) | 39 (56) | 16 (50) | .75 |
| Heart rate, bpm, median [IQR] | 96 [85–105] | 93 [81–105] | .42 |
| Systolic blood pressure ≤100 mmHg, n (%) | 5 (7) | 5 (16) | .33 |
| GCS <15, n (%) | 2 (3) | 14 (44) | <.01 |
| Respiratory Rate, n (%) | .89 | ||
| <9 breaths/min | 1 (1.6) | 0 (0.0) | |
| 9–14 breaths/min | 24 (38.1) | 11 (36.7) | |
| 15–20 breaths/min | 35 (55.6) | 17 (56.7) | |
| 21–30 breaths/min | 3 (4.8) | 2 (6.7) | |
| Neutrophil count, ×109/L, median [IQR] | 7.3 [5–12] | 9.3 [8–12] | .15 |
| Neutropenia, n (%) | 7 (11) | 0 (0) | .17 |
| Admission to hospital, n (%) | 44 (64) | 23 (72) | .51 |
| Pneumonia on CXR, n (%) | 0 (0) | 5 (16) | <.01 |
| Characteristics . | Reliable Medical History . | Unreliable Medical History . | P Value . |
|---|---|---|---|
| Patients, n | 70 | 32 | |
| Demographics | |||
| Age, year, median [IQR] | 62 [52–69] | 76 [66–83] | <.01 |
| Sex, male, n (%) | 31 (44) | 19 (59) | .23 |
| Chronic Comorbidity, n (%) | |||
| Asthma | 2 (3) | 1 (3) | 1.00 |
| COPD | 3 (4) | 1 (3) | 1.00 |
| Recent use of antineoplastic drugs | 16 (23) | 1 (3) | .03 |
| Hematologic malignancy | 10 (14) | 0 (0) | .06 |
| Solid tumor | 14 (20) | 4 (13) | .52 |
| Auto immune disease | 1 (1) | 0 (0) | 1.00 |
| Immunosuppressive medication | 4 (6) | 0 (0) | .41 |
| Sickle cell disease | 2 (3) | 0 (0) | .84 |
| Clinical Parameters | |||
| Temperature, n (%) | .15 | ||
| ≤36.0°C | 2 (3) | 4 (13) | |
| 36.0–38.0°C | 22 (31) | 8 (25) | |
| ≥38.0°C | 46 (66) | 20 (63) | |
| CRP ≥100 mg/L, n (%) | 39 (56) | 16 (50) | .75 |
| Heart rate, bpm, median [IQR] | 96 [85–105] | 93 [81–105] | .42 |
| Systolic blood pressure ≤100 mmHg, n (%) | 5 (7) | 5 (16) | .33 |
| GCS <15, n (%) | 2 (3) | 14 (44) | <.01 |
| Respiratory Rate, n (%) | .89 | ||
| <9 breaths/min | 1 (1.6) | 0 (0.0) | |
| 9–14 breaths/min | 24 (38.1) | 11 (36.7) | |
| 15–20 breaths/min | 35 (55.6) | 17 (56.7) | |
| 21–30 breaths/min | 3 (4.8) | 2 (6.7) | |
| Neutrophil count, ×109/L, median [IQR] | 7.3 [5–12] | 9.3 [8–12] | .15 |
| Neutropenia, n (%) | 7 (11) | 0 (0) | .17 |
| Admission to hospital, n (%) | 44 (64) | 23 (72) | .51 |
| Pneumonia on CXR, n (%) | 0 (0) | 5 (16) | <.01 |
Abbreviations: bpm, beats per minute; COPD, chronic obstructive pulmonary disease; CRP, C-reactive protein; CXR, chest x-ray; GCS Glasgow Coma Scale; IQR, interquartile range.
DISCUSSION
Our results suggest that a CXR has no diagnostic value in patients with suspected infection without respiratory signs or symptoms, if a reliable medical history can be obtained. The CXR demonstrated pneumonia in 5 of the 32 patients with an unreliable medical history. This implies that pulmonary imaging should be performed in those patients.
There were 5 patients that could be classified as having no respiratory signs or symptoms despite the respiratory rate being initially registered as >20, if the respiratory rate decreased during the stay at the emergency department. There were 2 women without evident extrapulmonary source of infection that had leukocyturia. However, their urinary cultures were negative, ruling out a urinary tract infection as the source of infection.
Concerning applicability, our study was the first to study a general internal medicine ED population. During the study period, we consecutively included all 2920 patients referred to the internal medicine ED of the Flevoziekenhuis (a teaching hospital with 386 beds). Therefore, the results are well applicable to an internal medicine ED of similar size [6].
CONCLUSIONS
Studies had already been performed in asymptomatic patients with neutropenic fever, showing pneumonia in 0% to 2.3% of the CXRs. All authors concluded that CXR should not be performed in asymptomatic febrile neutropenic patients [7–9]. The results of our study raise the hypothesis that this conclusion might be applicable to a more general population. External validation is also warranted in different settings than that of our study population [10]; for example, patients suspected of an infection during a hospital admission.
Acknowledgments
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Presented in part: 29th European Congress of Clinical Microbiology & Infectious Diseases, April 2019, Amsterdam, the Netherlands; Amsterdam European Congress of Emergency Medicine, October 12–16, 2019, Prague, Czech Republic.
References
Author notes
S. F. d. S. and L. P. contributed equally to this manuscript.





Comments