-
PDF
- Split View
-
Views
-
Cite
Cite
James Ayieko, Maya L Petersen, Annelies van Rie, Erick Wafula, Wilson Opudo, Tamara D Clark, Moses R Kamya, Laura B Balzer, Craig R Cohen, Elizabeth A Bukusi, Edwin D Charlebois, Diane V Havlir, Effect of a Patient-Centered Phone Call by a Clinical Officer at Time of HIV Testing on Linkage to Care in Rural Kenya, Open Forum Infectious Diseases, Volume 5, Issue 6, June 2018, ofy126, https://doi.org/10.1093/ofid/ofy126
Close - Share Icon Share
Abstract
In a randomized controlled trial, we tested whether a structured, patient-centered phone call from a clinical officer after HIV testing improved linkage to/re-engagement in HIV care. Among 130 HIV-positive persons, those randomized to the phone call were significantly more likely to link to care by 7 and 30 days (P = .04).
Timely linkage to HIV care is key to successful antiretroviral treatment (ART) and to effective treatment as prevention [1]. Poor linkage rates are well documented, with large proportions of HIV-positive persons not getting into care in a timely fashion [2]. There is need for simple, effective interventions to boost linkage to care for both the newly HIV-diagnosed and prior diagnosed persons who have fallen out of care or never linked to care.
In an ongoing test-and-treat trial where the UNAIDS “90-90-90” targets were achieved in the intervention arm by 2 years [3], we had the opportunity to test a simple phone call–based linkage strategy that was based on (i) social cognitive theory [4], (ii) observations that patients who had fallen out of care often re-engaged after a personal phone call from a clinical officer, and (iii) data on phone technology that have shown promise in improving treatment outcomes [5, 6].
METHODS
Study Design and Participants
We conducted a 2-arm randomized controlled trial (RCT) nested within the SEARCH trial (NCT01864683) in East Africa between August and December 2016. The RCT involved a subset of 5 Kenyan communities comprising approximately 5000 adults each from a region with an HIV prevalence of 20.1% [3]. HIV testing was done through a hybrid mobile HIV testing approach combining mobile, multidisease community health campaigns (CHCs) lasting 2 weeks per community with home-based HIV testing for those residents who did not attend CHCs [7]. All participants ≥15 years of age, HIV-positive, and who self-reported that they had either never linked to HIV care or had dropped out of care for >6 months were eligible for the nested RCT. Self-report of prior diagnosis and details of last clinic visit (or lack thereof) were confirmed by medical record review.
Study Procedures
All participants received standard HIV counseling and a transport voucher redeemable at linkage, irrespective of study arm. In addition, participants in the intervention arm received 1 structured call from a clinical officer, a holder of a diploma in medicine, within an hour of post-test counseling (Supplementary 1). The clinical officers had received training on principles of patient-centered care, problem-solving by role play of different scenarios reflecting the cultural context of the region.
A study staff made the call to the clinical officer using a study phone that was then handed to the participant. The content of the call included introductions, relationship initiation, and a brief assessment of the participant’s state of mind. The participant was provided with information about HIV disease and the benefits of early linkage and immediate treatment. The clinical officer assessed readiness to link, explored barriers to linkage, and sought solutions to overcome participant-specific barriers to ensure immediate linkage and treatment. The phone call conversation also included a description of a streamlined, patient-centered care model that would allow for spaced-out clinic visits, reduced waiting times, flexibility in visiting hours, and appointment reminders. Clinic options were provided for the participant to choose from; clinic staff details, including names, were also shared to ensure personalized service. A phone call checklist was used to ensure consistency and fidelity to the intervention (Supplementary Table 2).
Outcome
The primary end point was linkage to care at any ART clinic within 30 days of testing; linkage within 7 days was a secondary outcome. Time to linkage was defined as time between date of study enrollment and the first ART clinic visit. If a participant opted to link to a clinic outside the study community, linkage was verified by assessment of medical records. Absence of a linkage record was treated as failure to link.
Statistical Analysis
We conducted an intention-to-treat analysis. The proportions linking by 7 and 30 days between the intervention and control arms were compared using Pearson chi-square tests without continuity correction.
Cumulative linkage over time was estimated using Kaplan-Meier estimation. Cox proportional hazards models, adjusted for age and sex strata, were used to compare time to linkage between arms. We also used logistic regression models to explore factors associated with not linking to care.
Sample Size
Based on prior data within the SEARCH study, we assumed 56% linkage within 30 days in the control arm. A calculated sample size of 116 subjects (58 per arm) was based on simple unadjusted comparison of proportions, a 2-sided alpha of .05, and 80% power to detect an absolute effect size of 24% (80% linkage in the intervention arm).
Ethical Approval
The Kenya Medical Research Institute Ethical Review Committee (Kenya) and the University of California San Francisco Committee on Human Research (United States) approved the study, and participants provided consent.
RESULTS
Between August and December 2016, 223 participants were identified as eligible to participate in the study, 15 (6.7%) declined participation, and 208 were enrolled and randomized (Figure 1). The most common reason reported for decline was lack of time to participate in the study. Of the 208 enrolled, 78 were excluded from the analysis after establishing that they were ineligible due to medical records showing that they had linked to care before the study and had not been out of care for >6 months.
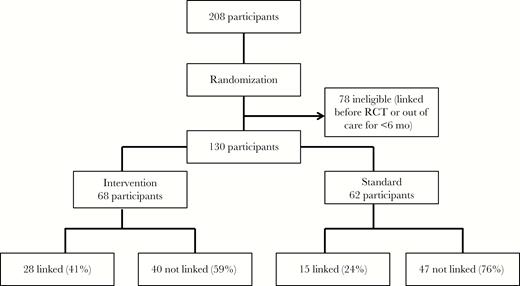
Study profile of 208 participants recruited into the study, with the final linkage outcomes by 30 days after intervention. Abbreviation: RCT, randomized controlled trial.
A total of 130 participants were included in the analysis (68 intervention, 62 control). Of these, 88 (68%) were newly diagnosed with HIV and 42 (32%) had a prior diagnosis but had never engaged in care or had dropped out of care >6 months before study enrollment; 109 (84%) of the participants were tested at the CHC. The median age (interquartile range) was 31 (27–40) years, 88 (64%) were <34 years old, 27% were male, 72% were married, 75% had a primary level of education or higher, and 20% were unemployed. The median length of the calls (range) was 17 (7–33) minutes. Baseline characteristics are available in Supplementary Table 2. Overall, 53/130 (41%) participants linked to care, with 43/130 (33%) linking within 30 days. The majority of individuals who linked (36/53, 68%) did so within 7 days. No deaths were reported during the follow-up period.
Participants in the intervention group were more likely to link to care within 7 days compared with those in the control group (24/68 [35%] vs 12/62 [19%]; P = .043). The effect of the intervention was maintained at 30 days (28/68 [41%] vs 15/62 [24%]; P = .040).
In Cox proportional hazards modeling, the relative hazard of linking to care at 30 days was higher in the intervention arm, before and after adjusting for age (< vs >35 years) and sex (hazard ratio [HR], 1.82; 95% confidence interval [CI], 0.97–3.41; P = .061; adjusted HR [aHR], 1.86; 95% CI, 0.99–3.48; P = .054), but estimates were imprecise.
In logistic regression models adjusted for community, younger people (<35 years vs >35 years; aOR, 0.32; 95% CI, 0.12–0.88; P .027) and individuals from households that did not have anyone else in HIV care (aOR, 0.33; 95% CI, 0.11–0.97; P = .045) were less likely to link within 30 days of testing.
The most common barriers to linkage reported were fear of disclosure to spouses, anticipated stigma, work-related mobility and travel, feeling healthy, and not seeing the need for treatment. Approaches used during the intervention call to overcome these barriers were matched to context and included facilitated disclosure, linkage to other community clinics, provision of information, and personal reassurances.
DISCUSSION
A personalized structured phone call by a health provider at the time of HIV testing significantly improved linkage to and re-engagement in care. Prior studies have demonstrated that messages focused on patients’ concerns, when delivered effectively, can be used to improve care engagement [8, 9]. Having a clinical officer rather than a lower-skilled worker perform the call, establishing rapport, health information empowerment, and addressing barriers to linkage while ensuring personalized care within a patient-centered context likely contributed to the success of the intervention.
In our setting, younger individuals and those from households without any members in HIV care were less likely to link. This is consistent with previous findings reporting lower linkage rates among the young and those lacking social support [2, 10, 11]. These findings suggest that interventions aimed at improving disclosure, stigma reduction, family/couple testing, and counseling could improve linkage to care for these groups.
The low overall linkage rates in this study compared with prior studies [12] may be explained in part by the study’s population, which included a significant proportion of “hard-to-engage” individuals, in particular persons with a previous diagnosis and history of failing to link to care and individuals who had engaged in care previously but had subsequently dropped out of care.
Our study had limitations. Our sample size was insufficient to assess the effectiveness of the intervention in subgroups of interest, such as those out of care vs the newly diagnosed. Second, reliance on self-report of newly diagnosed vs previously diagnosed disease may have resulted in some misclassification. Finally, linkage verification at clinics far removed from our study communities was not possible and may have led to underestimation of linkage.
In conclusion, a structured patient-centered phone call from a clinical officer at the time of HIV testing or re-engagement significantly improved the proportion of individuals linked to care. The proportion of individuals linked remained low, suggesting that more innovative interventions are needed to facilitate linkage to care, especially among hard-to-engage individuals such as youth and those living with HIV who have never linked to or dropped out of care.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
We are grateful to the participants from the 5 communities in Kenya who participated in this study. We would also like to thank the staff who performed testing and counseling for the participants and who made this study a success.
Prior presentation. Results contained in the manuscript were accepted for presentation at the 25th Conference on Retroviruses and Opportunistic Infections (CROI 2018) in Boston, Massachusetts.
Financial support. This work was supported by the National Institutes of Health (National Institute of Allergy and Infectious Diseases).
Potential conflicts of interest. D.V.H. reports grants from the National Institutes of Health (NIH) and nonfinancial support from Gilead Sciences during the conduct of the study; and grants from the NIH and the Gates Foundation outside the submitted work. E.C. reports grants from the NIH during the conduct of the study. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References





Comments