-
PDF
- Split View
-
Views
-
Cite
Cite
Tali Shafat, Daniel De-la-Rosa-Martinez, Fareed Khawaja, Ying Jiang, Amy Spallone, Marjorie Batista, Ella Ariza Heredia, Diana Vilar-Compte, Roy F Chemaly, P-730. Risk Factors for Severe Influenza and Respiratory Syncytial Virus Infections in Patients with Lymphoma or Multiple Myeloma - A Seven-Year Retrospective Cohort Study, Open Forum Infectious Diseases, Volume 12, Issue Supplement_1, February 2025, ofae631.926, https://doi.org/10.1093/ofid/ofae631.926
Close - Share Icon Share
Abstract
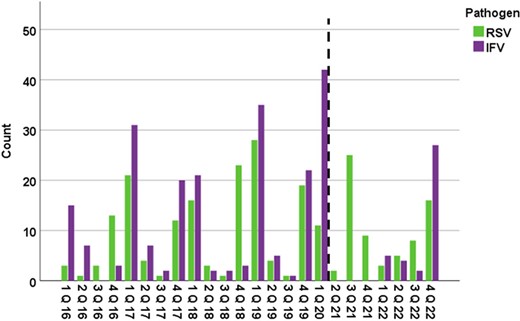
Respiratory viral infections per quarter stratified by viral pathogen.
The dashed line represents the beginning of the COVID-19 era in the USA (March 2020).
Abbreviations: IFV=influenza; Q=quarter; RSV= respiratory syncytial virus.
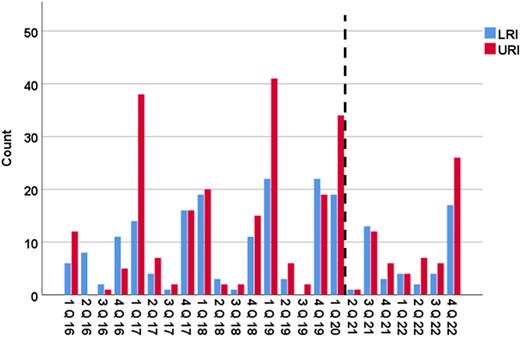
Respiratory viral infections per quarter stratified by site of infection.
The dashed line represents the beginning of the COVID-19 era in the USA (March 2020).
The LRI group includes patients who presented with LRI or progressed from URI to LRI.
Abbreviations: LRI=lower respiratory tract infection; Q=quarter; URI= upper respiratory tract infection
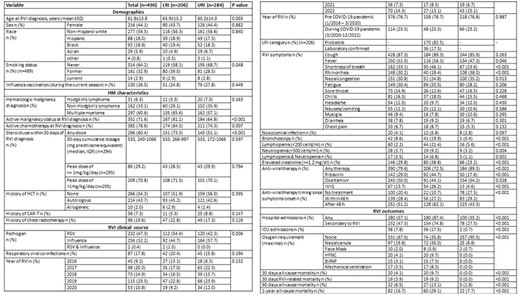
Baseline characteristics and clinical outcomes following respiratory viral infections by site of infection.
Abbreviations: BiPAP= bilevel positive airway pressure; CAR-T= chimeric antigen receptor T-cell therapy; COVID-19=Coronavirus Disease 2019; HCT= hematopoietic stem cell transplantation; HFNC= high-flow nasal cannula; HM= hematologic malignancy; ICU=intensive care unit; IQR= interquartile range; IVIG= Intravenous immunoglobulin; LRI= lower respiratory tract infection; RSV= respiratory syncytial virus; RVI= respiratory virus infection; SD=standard deviation; URI= upper respiratory tract infection.
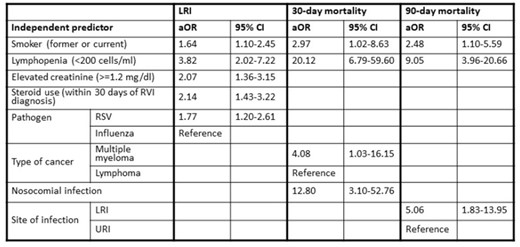
Independent predictors of LRI, 30-day and 90-day mortality by multivariable logistic regression.
Abbreviations: aOR=Adjusted-Odds Ratio; LRI= lower respiratory tract infection; RSV= respiratory syncytial virus; RVI=respiratory tract infection; URI= upper respiratory tract infection; 95% CI= 95% Confidence Interval.
Fareed Khawaja, MBBS, Eurofins Viracor: Grant/Research Support|Symbio: Grant/Research Support Roy F. Chemaly, MD/MPH, AiCuris: Advisor/Consultant|AiCuris: Grant/Research Support|Ansun Pharmaceuticals: Advisor/Consultant|Ansun Pharmaceuticals: Grant/Research Support|Astellas: Advisor/Consultant|Eurofins-Viracor: Grant/Research Support|InflaRX: Advisor/Consultant|Janssen: Advisor/Consultant|Karius: Advisor/Consultant|Karius: Grant/Research Support|Merck/MSD: Advisor/Consultant|Merck/MSD: Grant/Research Support|Moderna: Advisor/Consultant|Oxford Immunotec: Advisor/Consultant|Oxford Immunotec: Grant/Research Support|Roche/Genentech: Advisor/Consultant|Roche/Genentech: Grant/Research Support|Shinogi: Advisor/Consultant|Takeda: Advisor/Consultant|Takeda: Grant/Research Support|Tether: Advisor/Consultant
Author notes
Study Group:
Session: 65. Respiratory Infections - Viral
Thursday, October 17, 2024: 12:15 PM
- smoking
- influenza
- immunoglobulins, intravenous
- bi-level positive airway pressure
- hematopoietic stem cell transplantation
- adult
- consultants
- disclosure
- follow-up
- hematologic neoplasms
- intensive care unit
- lymphoma
- lymphopenia
- orthomyxoviridae
- respiratory syncytial virus infections
- respiratory syncytial viruses
- respiratory tract infections
- steroids
- virus diseases
- multiple myeloma
- infections
- morbidity
- mortality
- treatment outcome
- lower respiratory tract infections
- nosocomial infection
- pathogenic organism
- upper respiratory infections
- viral respiratory infections
- renal trauma
- allogeneic hematopoietic stem cell transplant
- pathogenicity
- high-flow nasal cannulas
- chimeric antigen receptor t-cell therapy
- primary outcome measure
- covid-19
- coronavirus pandemic





Comments