-
PDF
- Split View
-
Views
-
Cite
Cite
Jiashen Cai, Dorothy Huang, Hanis Abdul Kadir, Zhihua Huang, Li Choo Ng, Andrew Ang, Ngiap Chuan Tan, Yong Mong Bee, Wei Yi Tay, Chieh Suai Tan, Cynthia Lim, #100 Hospital readmissions for fluid overload among individuals with diabetes mellitus, Nephrology Dialysis Transplantation, Volume 39, Issue Supplement_1, May 2024, gfae069–1069–100, https://doi.org/10.1093/ndt/gfae069.1069
Close - Share Icon Share
Abstract
Hospital readmissions due to recurrent fluid overload in diabetes can be avoided with evidence-based interventions. To identify at-risk individuals, we evaluated the incidence and risk factors associated with fluid overload-related hospital readmissions and developed risk prediction models for readmissions for fluid overload in people with diabetes.
Single-centre retrospective cohort study of 1531 adults with diabetes and hospitalized in Singapore General Hospital for fluid overload, congestive heart failure, pulmonary edema and generalized edema between 2015 and 2017. Patients were included if they had diabetes mellitus identified by the SingHealth Diabetes Registry according to diagnosis codes, laboratory results and/or the use of glucose-lowering medication and had follow up visits, but excluded if their estimated glomerular filtration rate (eGFR) <15 ml/min/1.73 m2. Baseline data on demographics, comorbidities, biochemistry and medication use during admission were retrieved from electronic medical records up till 30 December 2018. The outcomes were fluid overload- related readmissions within 30 days and 90 days of discharge of the index hospitalization. Multivariable Cox proportional-hazards regression analysis was performed with inclusion of covariates with p≤0.10 on univariate analysis. Multivariable regression models developed were compared with the LACE index with net reclassification index (NRI).
Among 1531 patients, median age was 73 (IQR 64, 81) and readmissions for fluid overload within 30 days and 90 days occurred in 131 (8.6%) and 264 (17.2%) patients, respectively.
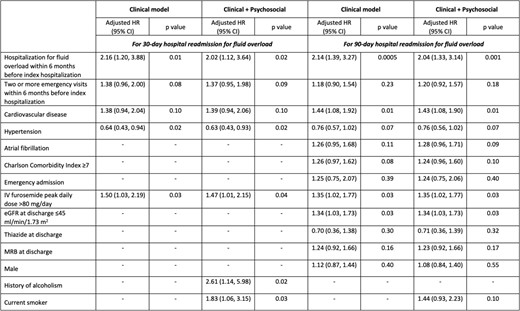
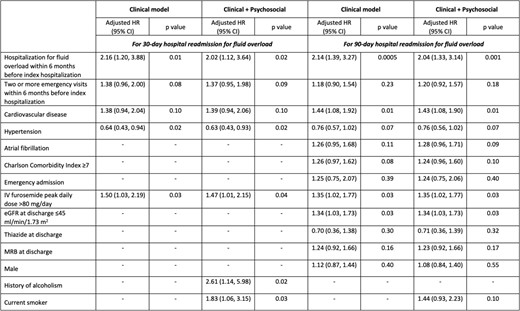
Individuals with 30- or 90-day readmissions were more likely to have prior hospitalization for fluid overload and more frequent ED visits within 6 months before the index hospitalization, cardiovascular disease, hypertension, and required high-dose intravenous furosemide during the index hospitalization, or current smoker.
Clinical and clinico-psychosocial models for 30- and 90-day readmissions for fluid overload were developed (Table 1). The clinical and clinico-psychosocial models showed better discrimination and calibration than LACE index for predicting 30- and 90-day readmissions for fluid overload. The NRIs for clinical models were i. 30-day readmissions: +22.1%, ii. 90-day readmissions: +27.9% respectively, while the NRIs for clinico-psychosocial models were i. 30-day readmissions: +22.4%, ii. 90-day readmissions: +28.9% respectively (Fig. 1).
Patients with diabetes who are at-risk of readmission for fluid overload can be identified for targeted interventions to reduce preventable hospitalizations.
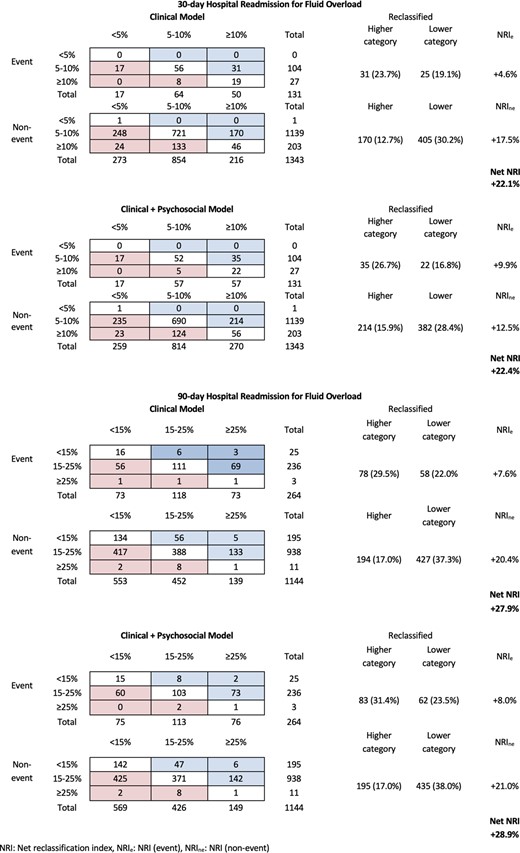
Net reclassification index of the developed risk models compared to LACE index for predicting 30- and 90-day hospital readmission for fluid overload in individuals with diabetes.
Developed risk models for 30- and 90-day hospital readmissions for fluid overload in individuals with diabetes.
Developed risk models for 30- and 90-day hospital readmissions for fluid overload in individuals with diabetes.
- anasarca
- furosemide
- hypertension
- cardiovascular diseases
- diabetes mellitus
- edema
- pulmonary edema
- congestive heart failure
- diabetes mellitus, type 2
- glucose
- adult
- biochemistry
- calibration
- comorbidity
- demography
- follow-up
- multivariate analysis
- patient readmission
- singapore
- diagnosis
- excess fluid volume
- drug usage
- electronic medical records
- evidence-based practice
- glomerular filtration rate, estimated
- univariate analysis
- net reclassification improvement
- risk prediction rule
- smokers





Comments