-
PDF
- Split View
-
Views
-
Cite
Cite
Matthias Cassia, Judit Cacho, Hugo Vergara Pérez, María Verónica Torres Jaramillo, Federico Alberici, Fritz Diekmann, David Cucchiari, #1327 mTOR inhibitors in kidney transplant recipients: long-term efficacy and discontinuation causes, Nephrology Dialysis Transplantation, Volume 39, Issue Supplement_1, May 2024, gfae069–0994–1327, https://doi.org/10.1093/ndt/gfae069.994
Close - Share Icon Share
Abstract
mTOR inhibitors use in kidney transplantation showed conflicting results, but their use as add-on treatment to calcineurin inhibitors (CNI) is still considered a valuable option. High frequency of drug discontinuation hinders their use in clinical practice. We present a real-life study on long term efficacy of mTOR inhibitors use vs mycophenolic acid (MPA) and the causes of drug discontinuation.
This is an observational retrospective monocentric study. We analyzed data from 773 patients that underwent kidney transplantation at Hospital Clinic between 2013 and 2019. Induction treatment was based either on basiliximab or a lymphocyte-depleting agent together with methylprednisolone. Maintenance treatment was based either on MPA or mTORi with a CNI. Baseline differences were accounted for with the Inverse Propensity of Treatment Weighting (IPTW). Outcomes explored were death with a functioning graft, graft loss or biopsy-proven rejection. Predictors of outcome were explored through logistic regression or Cox-regression as appropriate.
335/773 (43.3%) of the patients received MPA as maintenance treatment, whereas 438/773 (56.6%) received an mTOR inhibitor. Average follow-up was 3.36 years (SD ± 2.04 years). No outcome resulted statistically significant at the logistic regression weighted with IPTW in the subgroup mTORi vs MPA: odds ratio was 1.16 (0.75-1.63, p = 0.57) for death, 0.87 (0.54-1.41, p = 0.59) for graft loss and 1.15 (0.79-1.67, p = 0.45) for biopsy-proven acute rejection. The per-protocol analysis confirmed these results as not statistically significant. Strongest predictors of death resulted having a deceased donor of cardiac death (HR 2.17 (1.06-4.40, p = 0.03), having a delayed graft function (HR 1.9 (1.26-2.87, p = 0.002) and being readmitted within three months from the surgery (HR 1.76 (1.21-2.55, p = 0.003). Diabetic nephropathy as cause of kidney disease was significant as well (HR 2.01 (1.24-3.26, p = 0.004). Proportion of patients with a CMV infection were significantly lower in the mTORi than MPA subgroups (33.5% vs 41.5%, p = 0.02). Proportion of patients developing neoplasias were not significantly different (10% vs 11.3%, p = 0.55). A total of 307/773 (39.7%) of patients changed their immunosuppressive treatment at a median time of 110 days (26.5-375.5). In the MPA subgroup 77/335 (22.9%) changed treatment, whereas in the mTORi subgroup 230/438 (52.5%). The causes of change due to drug-related events were the most represented and related to mTOR treatment: lymphocele in 36/773 (4.6%), complications of the surgical wound in 31/773 (4.1%) and edemas in 23/773 (2.9%) were the most common. Of note, unspecific physician preference was cause of discontinuation in a total of 66/773 (8.5%) patients.
Our data from a tertiary-center, real-life experience show that mTOR inhibitors are a solid alternative to MPA based protocols, with effectiveness proven at the multivariate and weighted analysis. mTOR treatment has a high rate of discontinuation, with most of the causes represented by post-intervention complications; interestingly, physician preference represent a frequent cause. Further experience and research is needed to optimize mTORi treatment, in order to maintain a therapeutic option for transplanted patients.
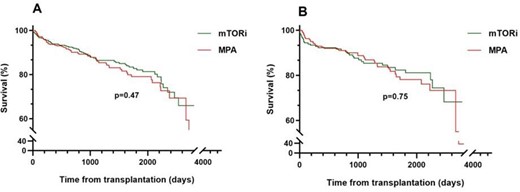
The figure shows the Kaplan-Meier survival analysis for death in the subgroup treated with mTOR inhibitors (green line) and mycophenolc acid (MPA, red line)). In the «A» panel the intention to treat subgroup, whereas in the «B» panel the per-protocol sub-group is shown.
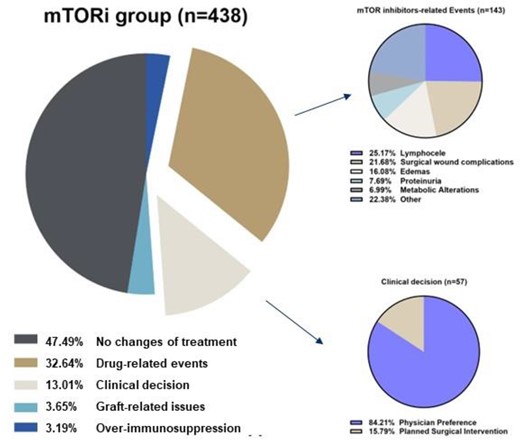
The figure shows the proportion of the causes of discontinuation in the mTOR inhibitors group. In the right graphs a detail of the «drug-related events» and «clinical decision» is showed.
- kidney diseases
- diabetic nephropathy
- renal transplantation
- edema
- immunosuppressive agents
- basiliximab
- biopsy
- follow-up
- lymphocele
- lymphocytes
- methylprednisolone
- mycophenolic acid
- rejection (psychology)
- surgical procedures, operative
- tissue transplants
- cytomegalovirus infections
- heart
- surgery specialty
- surgical incisions
- graphical displays
- calcineurin inhibitors
- kaplan-meier survival curve
- cox proportional hazards models
- mtor serine-threonine kinases
- per protocol analysis
- intention to treat
- mtor inhibitors
- graft loss
- donors
- delayed graft function





Comments