-
PDF
- Split View
-
Views
-
Cite
Cite
Tudor Sergiu Niculae, Otilia Ciurea, Nicoleta Petre, Gabriel Mircescu, Cristina-Stela Capusa, #4918 IS THE KIDNEY FAILURE RISK EQUATION VALID IN PREDICTING END STAGE KIDNEY DISEASE IN ADULTS WITH GLOMERULOPATHIES?, Nephrology Dialysis Transplantation, Volume 38, Issue Supplement_1, June 2023, gfad063c_4918, https://doi.org/10.1093/ndt/gfad063c_4918
Close - Share Icon Share
Abstract
The Kidney Failure Risk Equation (KFRE) is a clinical tool that predicts the 2- and 5- year risk of progression to end stage kidney disease (ESKD) in patients with chronic kidney disease (CKD) stages 3a-5. The equation's accuracy and its predictive performance in subjects with glomerulopathies were not properly evaluated and validated. The current study examined the 4 variable KFRE in subjects with advanced CKD from glomerulopathy etiologies by evaluating discrimination and calibration at 2 and 5 years.
This retrospective, single-center, cohort study included 558 subjects who were diagnosed by kidney biopsy with primary or secondary glomerulopathies between 1st January 2008 and 31st December 2016 and followed until 31st December 2021 for a mean follow-up time of 85.3 (95%CI 78.9 to 91.8) months. Patients with inadequate biopsy samples, histological findings other than glomerulopathy, those with missing data, and those with eGFR > 60 ml/min/1.73 m2 were excluded. The 4-variable KFRE using eGFR, urinary albumin to creatinine ratio (uACR), age, and sex was calculated using the data from the first visit. The primary outcome of the study was the need for renal replacement therapy (RRT) initiation (dialysis or kidney transplant). The area under the receiver operator characteristic curve (AUC) and calibration plots were used to measure discrimination and calibration of the KFRE in specific glomerulopathy etiologies: IgA nephropathy, diabetic nephropathy, amyloidosis, endocapillary and crescentic glomerulonephritis, lupus nephritis, minimal change disease, membranous nephropathy, focal segmental glomerulosclerosis and membranoproliferative glomerulonephritis.
In this cohort, most of the patients were males (57.7%) and the median age was 53 (95%CI 53 to 57) years. The median eGFR was 30,5 (95%CI 28 to 32,6) ml/min/ 1.73 m2 and the median uACR 1932 (95% CI 1633 to 2200) mg/g. The most common glomerulopathies were IgA nephropathy (21.3%), diabetic nephropathy (13.4%), and membrano-proliferative glomerulonephritis (9.5%). The median 2-year and 5-year KFRE score was 2.2 (95%CI 1.8 to 2.7) % and 18.9 (95%CI 17.8 to 19.7) % respectively. During the first 2 years of follow-up 154 (27.5%) subjects needed RRT and 93 (16.6%) subjects died, while 218 (39%) started RRT and 108 (19.3%) died within 5 years from the kidney biopsy. The 4-variable KFRE provided good discrimination in the whole cohort with an AUC of 0.728 (95% CI 0.686-0.770) for predicting ESRD at 2-years and 0.725 (95% CI 0.686-0.767) at 5 years (Figure 1A). There was also a good to excellent discrimination of 2-years and 5-years KFRE across all glomerulopathy etiologies, with statistically significant p-values (p<0.05), with the exception of diabetic nephropathy and endocapillary GN which had a non-significant AUC (Figure 2). Calibration plots were adequate both overall and across glomerulopathy etiologies; however, the predicted risks for kidney failure were overestimated across CKD etiologies, especially in those with low to moderate risk in the 2-years model. Notably the calibration plot for the 5-years KFRE showed that the predicted risk was near the observed risk across all glomerulopathies (Figure 1B).
The 4 variable-KFRE seems to be a good predictive tool in patients with glomerulopathies both for 2 and 5-years, except for diabetic nephropathy and endocapillary glomerulonephritis.

A. ROC curves for the 4-variable KFRE at 2 and 5 years for the whole cohort. 1B. A calibration plot for the 4-variable KFRE at 5 years.
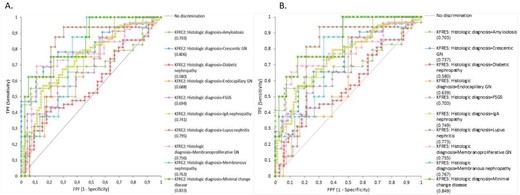
ROC curves for the 4-variable KFRE at 2- and 5-years according to glomerulopathy etiologies. A. ROC curve for KFRE at 2-years; B. ROC curve for KFRE at 5-years.
- amyloidosis
- hemodialysis
- diabetic nephropathy
- renal transplantation
- glomerulonephritis
- albumins
- kidney failure, chronic
- biopsy
- creatinine
- kidney failure
- adult
- calibration
- follow-up
- iga glomerulonephritis
- membranoproliferative glomerulonephritis
- membranous glomerulonephritis
- focal glomerulosclerosis
- lupus nephritis
- lipoid nephrosis
- renal replacement therapy
- roc curve
- urinary tract
- renal glomerular disease
- dialysis procedure
- pauci-immune crescentic glomerulonephritis
- renal biopsy
- clinical diagnostic instrument
- urine albumin/creatinine ratio
- idiopathic crescentic glomerulonephritis
- missing data
- primary outcome measure





Comments