-
PDF
- Split View
-
Views
-
Cite
Cite
Gregory L Hundemer, Pietro Ravani, Manish M Sood, Deborah Zimmerman, Amber O Molnar, Danielle Moorman, Matthew J Oliver, Christine White, Swapnil Hiremath, Ayub Akbari, Social determinants of health and the transition from advanced chronic kidney disease to kidney failure, Nephrology Dialysis Transplantation, Volume 38, Issue 7, July 2023, Pages 1682–1690, https://doi.org/10.1093/ndt/gfac302
Close - Share Icon Share
ABSTRACT
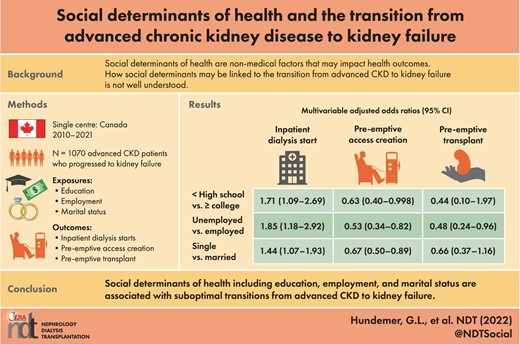
The transition from chronic kidney disease (CKD) to kidney failure is a vulnerable time for patients, with suboptimal transitions associated with increased morbidity and mortality. Whether social determinants of health are associated with suboptimal transitions is not well understood.
This retrospective cohort study included 1070 patients with advanced CKD who were referred to the Ottawa Hospital Multi-Care Kidney Clinic and developed kidney failure (dialysis or kidney transplantation) between 2010 and 2021. Social determinant information, including education level, employment status and marital status, was collected under routine clinic protocol. Outcomes surrounding suboptimal transition included inpatient (versus outpatient) dialysis starts, pre-emptive (versus delayed) access creation and pre-emptive kidney transplantation. We examined the association between social determinants of health and suboptimal transition outcomes using multivariable logistic regression.
The mean age and estimated glomerular filtration rate were 63 years and 18 ml/min/1.73 m2, respectively. Not having a high school degree was associated with higher odds for an inpatient dialysis start compared with having a college degree {odds ratio [OR] 1.71 [95% confidence interval (CI) 1.09–2.69]}. Unemployment was associated with higher odds for an inpatient dialysis start [OR 1.85 (95% CI 1.18–2.92)], lower odds for pre-emptive access creation [OR 0.53 (95% CI 0.34–0.82)] and lower odds for pre-emptive kidney transplantation [OR 0.48 (95% CI 0.24–0.96)] compared with active employment. Being single was associated with higher odds for an inpatient dialysis start [OR 1.44 (95% CI 1.07–1.93)] and lower odds for pre-emptive access creation [OR 0.67 (95% CI 0.50–0.89)] compared with being married.
Social determinants of health, including education, employment and marital status, are associated with suboptimal transitions from CKD to kidney failure.
What is already known about this subject?
The transition from advanced chronic kidney disease (CKD) to kidney failure is a vulnerable time for patients, with suboptimal transitions associated with increased morbidity and mortality.
Social determinants of health (e.g. education, employment, income) are strongly linked to the incidence of both CKD and kidney failure.
Whether social determinants of health are associated with suboptimal transitions from CKD to kidney failure is not well understood.
What this study adds?
Lower education levels, unemployment and being single (versus married) were associated with suboptimal transitions from advanced CKD to kidney failure.
Indicators of suboptimal transitions associated with these social determinants of health included a higher likelihood of inpatient (versus outpatient) dialysis starts, a lower likelihood of pre-emptive (versus delayed) access creation and a lower likelihood of pre-emptive kidney transplantation.
What impact this may have on practice or policy?
This study highlights the important role that social determinants of health play during the vulnerable transition period between advanced CKD and kidney failure.
These social determinants of health are ‘upstream’ factors that require improvement in the infrastructure of nephrology care as a whole if we hope to see an improvement in patient outcomes.
INTRODUCTION
The transition from advanced chronic kidney disease (CKD) to kidney failure is a challenge for both patients and nephrologists. Patients with advanced CKD are particularly vulnerable during this time period and experience high rates of adverse events that impact their outcomes even after they ultimately transition to kidney replacement therapies [1–4]. Because of this, there has been a move in nephrology towards developing specialized multidisciplinary clinics specifically dedicated to this pre–kidney failure population [5]. These clinics are designed to mitigate CKD-related complications, provide education about kidney replacement therapies, including dialysis and kidney transplantation, and smooth the transition from advanced CKD to kidney failure. Yet despite these efforts, the transition from advanced CKD to kidney failure remains suboptimal, with approximately half of patients starting dialysis in the inpatient setting, the majority of patients starting haemodialysis (HD) with a catheter and only a small minority undergoing pre-emptive kidney transplantation [3, 6–15].
A better understanding of the factors that impact this transition phase from advanced CKD to kidney failure may allow for improved identification of patients at high risk for a suboptimal transition. In turn, additional healthcare resources (e.g. education, outreach, etc.) could be prioritized toward this highly susceptible subset of the advanced CKD population to help smooth the transition phase. Prior studies assessing factors associated with a suboptimal transition from advanced CKD to kidney failure have focused on traditional medical risk factors such as age, cardiovascular disease, obesity and late referral to nephrology [6–9, 11, 12, 14]. However, the association between social determinants of health and the transition from advanced CKD to kidney failure has not been well studied. Social determinants of health refer to non-medical factors that have a major influence on health outcomes, such as education, employment, income, literacy and home environment [16]. In modern-day nephrology practice, information about these social determinants of health is not typically collected as part of standard advanced CKD care at most centres.
Social determinants of health are strongly linked to CKD prevalence and outcomes. For instance, lower education levels are associated with a higher mortality risk among individuals with CKD [17, 18]. Further, unemployment and lower income levels are strongly associated with a heightened prevalence of CKD and kidney failure [17–20]. Yet, to date, it remains not well understood how social determinants of health influence the transition from CKD to kidney failure. In fact, acknowledging and addressing these ‘upstream’ social factors that may impact kidney disease has been identified as an area in need of improvement within the nephrology community [21]. Herein we conducted a retrospective study to assess the association between social determinants of health (education level, employment status and marital status) and outcomes surrounding the transition from CKD to kidney failure, including inpatient (versus outpatient) dialysis starts, pre-emptive (versus delayed) access creation and pre-emptive kidney transplantation.
MATERIALS AND METHODS
Study design
We performed a retrospective cohort study of consecutive adult (≥18 years of age) patients with advanced CKD who were referred to the Ottawa Hospital Multi-Care Kidney Clinic and developed kidney failure (defined as dialysis or kidney transplantation) between 2010 and 2021.
Data source and study cohort
This study was conducted at the Ottawa Hospital Multi-Care Kidney Clinic (Ottawa, Ontario, Canada). The Ottawa Hospital is a 1150-bed academic tertiary care centre with a catchment area of ≈1.3 million people. The Ottawa Hospital Multi-Care Kidney Clinic is a specialty nephrology clinic designed to provide comprehensive, multidisciplinary care for patients with advanced CKD and is the sole such program within the catchment area. Timing of referral is at the discretion of the primary nephrologist, although referrals are suggested when the estimated glomerular filtration rate (eGFR) is <25 ml/min/1.73 m2 or the 2-year four-variable Kidney Failure Risk Equation [22] score is >20%. Patients are seen in the clinic typically every 3 months, although this interval can vary from as often as every 2 weeks to as long as every 6 months, at the discretion of the nephrologist. At each visit, patients are seen by a nurse, dietician and nephrologist, with pharmacist and social work support available as needed. Patients are educated about kidney failure treatment options, including HD, peritoneal dialysis (PD), kidney transplantation and conservative management.
The study cohort was derived from a database of all patients referred to the Multi-Care Kidney Clinic since 1 January 2010 with follow-up data available through 31 December 2021. The database undergoes random data audits every 6–12 months where the data are compared with the electronic medical record to ensure accuracy. As part of routine clinic protocol, a social worker meets with each patient at the time of the initial clinic referral visit and collects social determinant information including education level, employment status and marital status. Patients were included in the study if they developed kidney failure (which we defined as dialysis or kidney transplantation) within the study time window (1 January 2010–31 December 2021). The only exclusion criterion was if a patient had incomplete baseline social determinant and/or laboratory data. All protocols were approved by the Ottawa Health Science Network Research Ethics Board (protocol ID 20210228-01H). Informed consent requirements were waived due to the retrospective nature of the data.
Exposures
We assessed three social determinant exposures: education level, employment status and marital status. Education level was categorized as college degree or higher, high school degree or less than a high school degree based on the patient's terminal degree. Employment status was categorized as employed, unemployed or retired. Marital status was categorized as married or single.
Outcomes
We assessed three outcomes surrounding the transition from advanced CKD to kidney failure: inpatient (versus outpatient) dialysis starts, pre-emptive (versus delayed) access creation and pre-emptive kidney transplantation. Inpatient dialysis starts included both HD and PD. Pre-emptive access creation included arteriovenous fistula, arteriovenous graft and PD catheter insertion. Of note, standard practice at the Ottawa Hospital Multi-Care Kidney Clinic for patients who elect to pursue PD is to place a buried PD catheter when the eGFR is 10–15 ml/min/1.73 m2; the catheter remains buried until the patient needs to start dialysis, at which point the catheter is exteriorized. For the outcome of pre-emptive access creation, we excluded patients who underwent pre-emptive kidney transplantation.
Statistical analysis
For baseline data, continuous variables were expressed as mean [standard deviation (SD)] if normally distributed and as median [25th–75th percentile interquartile range (IQR)] if non-normally distributed, while categorical variables were expressed as number (%). We then determined the number (%) of patients who developed each outcome by the aforementioned social determinants and used chi-squared testing to assess for statistically significant differences. We then used univariable and multivariable logistic regression models to measure both crude and adjusted odds ratios (ORs) along with 95% confidence intervals (CIs) in the association between each social determinants of health (education level, employment status, marital status) and the outcomes (inpatient dialysis start, pre-emptive access creation, pre-emptive kidney transplantation). The multivariable models were adjusted for the following covariates selected a priori and collected at the time of the initial visit to the Multi-Care Kidney Clinic: age, sex, self-reported race, eGFR, urine albumin:creatinine ratio (UACR), obesity (defined as a body mass index >30 kg/m2), diabetes mellitus, hypertension, cardiovascular disease, education level, employment status and marital status. eGFR was calculated using the 2021 Chronic Kidney Disease Epidemiology Collaboration creatinine equation [23]. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). The 95% CIs that did not overlap with 1.0 and two-sided P-values <.05 were considered statistically significant.
RESULTS
Baseline characteristics
A total of 1519 patients with advanced CKD were referred to the Ottawa Hospital Multi-Care Kidney Clinic and developed kidney failure between 1 January 2010 and 31 December 2021. The final study cohort included 1070 patients after excluding those with incomplete baseline social determinant and/or laboratory data (n = 449). The baseline characteristics of the study cohort are displayed in Table 1. The mean age was 63 years (SD 15) and 37% of patients were female. The majority (73%) of the population was white. The mean serum creatinine and eGFR at the time of clinic referral were 322 μmol/L (SD 100) and 18 ml/min/1.73 m2 (SD 6), respectively. The median UACR was 204 mg/mmol (IQR 78–387). Hypertension (94%) and diabetes mellitus (61%) were common in the cohort.
| Variable . | Values . |
|---|---|
| Age (years), mean (SD) | 63 (15) |
| Sex, n (%) | |
| Female | 400 (37) |
| Male | 670 (63) |
| Race, n (%) | |
| White | 778 (73) |
| Asian | 165 (15) |
| Black | 49 (5) |
| Aboriginal | 22 (2) |
| Other/unknown | 56 (5) |
| Laboratory data | |
| Creatinine (μmol/L), mean (SD) | 322 (100) |
| eGFR (ml/min/1.73 m2), mean (SD) | 18 (6) |
| Potassium (mmol/L), mean (SD) | 4.51 (0.56) |
| Bicarbonate (mmol/L), mean (SD) | 24 (3) |
| Calcium (mmol/L), mean (SD) | 2.22 (0.15) |
| Phosphate (mmol/L), mean (SD) | 1.38 (0.30) |
| Parathyroid hormone (pmol/L), median (IQR) | 20.1 (12.2–30.6) |
| Albumin (g/L), mean (SD) | 34 (5) |
| Haemoglobin (g/L), mean (SD) | 110 (16) |
| UACR (mg/mmol), median (IQR) | 204 (78–387) |
| Comorbidities, n (%) | |
| Coronary artery disease | 323 (30) |
| Congestive heart failure | 251 (23) |
| Stroke | 136 (13) |
| Hypertension | 1007 (94) |
| Diabetes mellitus | 652 (61) |
| Medication use, n (%) | |
| ACEI/ARB | 543 (51) |
| Diuretic | 619 (58) |
| Social determinants | |
| Education level, n (%) | |
| ≥College degree | 571 (53) |
| High school degree | 383 (36) |
| <High school degree | 116 (11) |
| Employment status, n (%) | |
| Employed | 259 (24) |
| Unemployed | 262 (24) |
| Retired | 549 (51) |
| Marital status, n (%) | |
| Married | 669 (63) |
| Single | 401 (37) |
| Variable . | Values . |
|---|---|
| Age (years), mean (SD) | 63 (15) |
| Sex, n (%) | |
| Female | 400 (37) |
| Male | 670 (63) |
| Race, n (%) | |
| White | 778 (73) |
| Asian | 165 (15) |
| Black | 49 (5) |
| Aboriginal | 22 (2) |
| Other/unknown | 56 (5) |
| Laboratory data | |
| Creatinine (μmol/L), mean (SD) | 322 (100) |
| eGFR (ml/min/1.73 m2), mean (SD) | 18 (6) |
| Potassium (mmol/L), mean (SD) | 4.51 (0.56) |
| Bicarbonate (mmol/L), mean (SD) | 24 (3) |
| Calcium (mmol/L), mean (SD) | 2.22 (0.15) |
| Phosphate (mmol/L), mean (SD) | 1.38 (0.30) |
| Parathyroid hormone (pmol/L), median (IQR) | 20.1 (12.2–30.6) |
| Albumin (g/L), mean (SD) | 34 (5) |
| Haemoglobin (g/L), mean (SD) | 110 (16) |
| UACR (mg/mmol), median (IQR) | 204 (78–387) |
| Comorbidities, n (%) | |
| Coronary artery disease | 323 (30) |
| Congestive heart failure | 251 (23) |
| Stroke | 136 (13) |
| Hypertension | 1007 (94) |
| Diabetes mellitus | 652 (61) |
| Medication use, n (%) | |
| ACEI/ARB | 543 (51) |
| Diuretic | 619 (58) |
| Social determinants | |
| Education level, n (%) | |
| ≥College degree | 571 (53) |
| High school degree | 383 (36) |
| <High school degree | 116 (11) |
| Employment status, n (%) | |
| Employed | 259 (24) |
| Unemployed | 262 (24) |
| Retired | 549 (51) |
| Marital status, n (%) | |
| Married | 669 (63) |
| Single | 401 (37) |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
| Variable . | Values . |
|---|---|
| Age (years), mean (SD) | 63 (15) |
| Sex, n (%) | |
| Female | 400 (37) |
| Male | 670 (63) |
| Race, n (%) | |
| White | 778 (73) |
| Asian | 165 (15) |
| Black | 49 (5) |
| Aboriginal | 22 (2) |
| Other/unknown | 56 (5) |
| Laboratory data | |
| Creatinine (μmol/L), mean (SD) | 322 (100) |
| eGFR (ml/min/1.73 m2), mean (SD) | 18 (6) |
| Potassium (mmol/L), mean (SD) | 4.51 (0.56) |
| Bicarbonate (mmol/L), mean (SD) | 24 (3) |
| Calcium (mmol/L), mean (SD) | 2.22 (0.15) |
| Phosphate (mmol/L), mean (SD) | 1.38 (0.30) |
| Parathyroid hormone (pmol/L), median (IQR) | 20.1 (12.2–30.6) |
| Albumin (g/L), mean (SD) | 34 (5) |
| Haemoglobin (g/L), mean (SD) | 110 (16) |
| UACR (mg/mmol), median (IQR) | 204 (78–387) |
| Comorbidities, n (%) | |
| Coronary artery disease | 323 (30) |
| Congestive heart failure | 251 (23) |
| Stroke | 136 (13) |
| Hypertension | 1007 (94) |
| Diabetes mellitus | 652 (61) |
| Medication use, n (%) | |
| ACEI/ARB | 543 (51) |
| Diuretic | 619 (58) |
| Social determinants | |
| Education level, n (%) | |
| ≥College degree | 571 (53) |
| High school degree | 383 (36) |
| <High school degree | 116 (11) |
| Employment status, n (%) | |
| Employed | 259 (24) |
| Unemployed | 262 (24) |
| Retired | 549 (51) |
| Marital status, n (%) | |
| Married | 669 (63) |
| Single | 401 (37) |
| Variable . | Values . |
|---|---|
| Age (years), mean (SD) | 63 (15) |
| Sex, n (%) | |
| Female | 400 (37) |
| Male | 670 (63) |
| Race, n (%) | |
| White | 778 (73) |
| Asian | 165 (15) |
| Black | 49 (5) |
| Aboriginal | 22 (2) |
| Other/unknown | 56 (5) |
| Laboratory data | |
| Creatinine (μmol/L), mean (SD) | 322 (100) |
| eGFR (ml/min/1.73 m2), mean (SD) | 18 (6) |
| Potassium (mmol/L), mean (SD) | 4.51 (0.56) |
| Bicarbonate (mmol/L), mean (SD) | 24 (3) |
| Calcium (mmol/L), mean (SD) | 2.22 (0.15) |
| Phosphate (mmol/L), mean (SD) | 1.38 (0.30) |
| Parathyroid hormone (pmol/L), median (IQR) | 20.1 (12.2–30.6) |
| Albumin (g/L), mean (SD) | 34 (5) |
| Haemoglobin (g/L), mean (SD) | 110 (16) |
| UACR (mg/mmol), median (IQR) | 204 (78–387) |
| Comorbidities, n (%) | |
| Coronary artery disease | 323 (30) |
| Congestive heart failure | 251 (23) |
| Stroke | 136 (13) |
| Hypertension | 1007 (94) |
| Diabetes mellitus | 652 (61) |
| Medication use, n (%) | |
| ACEI/ARB | 543 (51) |
| Diuretic | 619 (58) |
| Social determinants | |
| Education level, n (%) | |
| ≥College degree | 571 (53) |
| High school degree | 383 (36) |
| <High school degree | 116 (11) |
| Employment status, n (%) | |
| Employed | 259 (24) |
| Unemployed | 262 (24) |
| Retired | 549 (51) |
| Marital status, n (%) | |
| Married | 669 (63) |
| Single | 401 (37) |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
For the social determinants of health, we captured education level, employment status and marital status at the time of the initial clinic visit (Table 1). Regarding education level, 53% of patients had attained a college degree or higher, 36% attained a high school degree and 11% did not attain a high school degree. Regarding employment status, 24% of patients were employed, 24% were unemployed and 51% were retired. The majority of patients (63%) were married, while 37% were single.
Education level and suboptimal transition outcomes
Fig. 1A displays the incidence of suboptimal transition outcomes by education level. Patients with a lower education level were more likely to have an inpatient dialysis start (P < .001), less likely to have pre-emptive access creation (P = .001) and less likely to undergo pre-emptive kidney transplantation (P = .006) compared with patients with a higher education level. Fig. 1B displays the crude and adjusted ORs for the association between education level and suboptimal transition outcomes. Not having a high school degree was associated with higher odds for an inpatient dialysis start [adjusted OR 1.71 (95% CI 1.09–2.69)] and lower odds for pre-emptive access creation [adjusted OR 0.63 (95% CI 0.40–0.998)] compared with a college degree. On multivariable regression analysis, there was no significant difference in the odds for the suboptimal transition outcomes between patients who attained a high school degree compared with those who attained a college degree or higher.
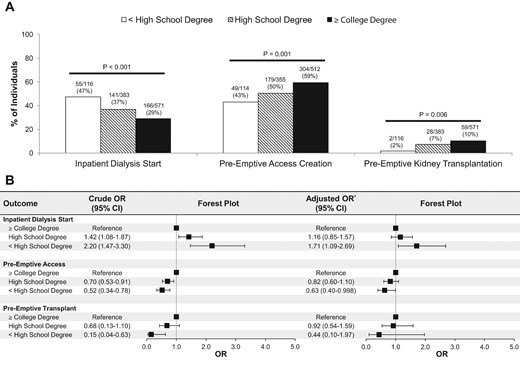
Association between education level and outcomes surrounding the transition from advanced CKD to kidney failure. *Adjusted for age, sex, self-reported race, eGFR, UACR, obesity, diabetes mellitus, hypertension, cardiovascular disease, employment status and marital status.
Employment status and suboptimal transition outcomes
Fig. 2A displays the incidence of suboptimal transition outcomes by employment status. Patients with active employment were less likely to have an inpatient dialysis start (P < .001), more likely to have pre-emptive access creation (P < .001) and more likely to undergo pre-emptive kidney transplantation (P < .001) compared with patients who were unemployed or retired. Fig. 2B displays the crude and adjusted ORs for the association between employment status and suboptimal transition outcomes. Unemployment was associated with higher odds for an inpatient dialysis start [adjusted OR 1.85 (95% CI 1.18–2.92)], lower odds for pre-emptive access creation [adjusted OR 0.53 (95% CI 0.34–0.82)] and lower odds for pre-emptive kidney transplantation [adjusted OR 0.48 (95% CI 0.24–0.96)] compared with active employment. Retirement was also associated with higher odds for an inpatient dialysis start [adjusted OR 1.70 (95% CI 1.05–2.77)] and lower odds for pre-emptive access creation [adjusted OR 0.53 (95% CI 0.33–0.85)], but no difference in odds for pre-emptive kidney transplantation [adjusted OR 1.43 (95% CI 0.67–3.05)] compared with active employment.
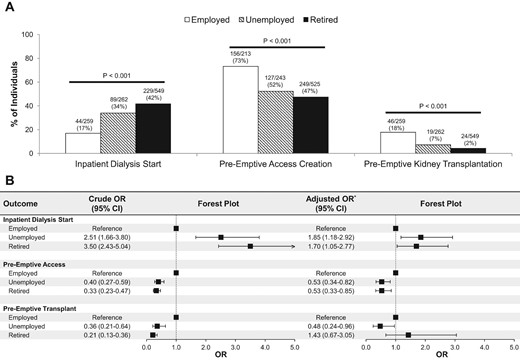
Association between employment status and outcomes surrounding the transition from advanced CKD to kidney failure. *Adjusted for age, sex, self-reported race, eGFR, UACR, obesity, diabetes mellitus, hypertension, cardiovascular disease, education level and marital status.
Marital status and suboptimal transition outcomes
Fig. 3A displays the incidence of suboptimal transition outcomes by marital status. Married patients were less likely to have an inpatient dialysis start (P = .03) and more likely to have pre-emptive access creation (P = .003) compared with single patients, whereas there was no significant difference in regard to pre-emptive kidney transplantation (P = .44). Fig. 3B displays the crude and adjusted ORs for the association between marital status and suboptimal transition outcomes. Being single was associated with higher odds for an inpatient dialysis start [adjusted OR 1.44 (95% CI 1.07–1.93)] and lower odds for pre-emptive access creation [adjusted OR 0.67 (95% CI 0.50–0.89)] but no difference in odds for pre-emptive kidney transplantation [adjusted OR 0.66 (95% CI 0.37–1.16)] compared with being married.
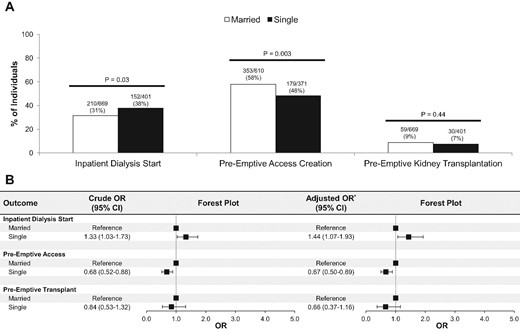
Association between marital status and outcomes surrounding the transition from advanced CKD to kidney failure. *Adjusted for age, sex, self-reported race, eGFR, UACR, obesity, diabetes mellitus, hypertension, cardiovascular disease, education level and employment status.
DISCUSSION
In this retrospective cohort study of adult patients with advanced CKD who transitioned to kidney failure, we found that social determinants of health were associated with suboptimal transitions. Lower education levels were associated with a higher likelihood of starting dialysis in the inpatient setting and initiating dialysis without a pre-created access. Lack of employment was associated with a higher likelihood of starting dialysis in the inpatient setting and initiating dialysis without a pre-created access along with a lower likelihood of receiving a pre-emptive kidney transplant. Compared with married patients, single patients had a higher likelihood of starting dialysis in the inpatient setting and initiating dialysis without a pre-created access. These results speak to the important role that these ‘upstream’ social determinants of health play during the vulnerable time period when patients with advanced CKD are transitioning to kidney failure.
Our results expand upon prior studies examining the influence of social determinants of health upon patients with kidney disease. These factors, such as income level, employment status and race, have been shown to be strongly linked to both CKD prevalence and adverse associated outcomes. An abundance of studies has demonstrated that low income is associated with the incidence of CKD and albuminuria [17–19, 24–30]. Perhaps more importantly, income level is even more strongly linked to kidney failure [20, 31–33]. For instance, Volkova et al. [20] reported a 4-fold higher incidence of kidney failure in areas of high versus low levels of residential poverty. Jurkovitz et al. [34] found that a lack of health insurance in the USA (where insurance is closely tied to employment) among CKD patients was associated with a 72% higher risk of kidney failure and an 82% higher risk of death. Even after low-income patients develop kidney failure and transition to dialysis, they experience longer wait times for kidney transplantation and a higher risk of death compared with higher-income patients [35, 36].
Several studies have also highlighted the strong link between education level and CKD, along with its associated outcomes [21, 37, 38]. Choi et al. [37] found that a higher educational level (non–high school graduate, high school graduate, some college or college graduate) was directly associated with kidney function but inversely associated with albuminuria. Moreover, those patients who attained a college degree had a 24% lower mortality risk compared with those patients who did not graduate from high school. An epidemiologic subanalysis of the Study of Heart and Renal Protection randomized controlled trial found that among participants with moderate–severe CKD, having no formal education was associated with a 46% higher risk for vascular events (cardiac, cerebral or peripheral vascular) and a 2-fold higher risk of death compared with having completed tertiary education [38].
The current study now links social determinants of health to outcomes surrounding the transition from advanced CKD to kidney failure. Just as education level and employment status are linked to the incidence and associated outcomes of both CKD and kidney failure, we now demonstrate that they are also associated with the transition between these two disease states. Advanced CKD patients with higher formal education levels and active employment are more likely to transition to kidney failure in an optimal fashion, i.e. starting dialysis in the outpatient setting with a pre-created access or, better yet, with pre-emptive kidney transplantation. A novelty in our study is assessing marital status as a social determinant of health, one which has not been well studied in kidney disease previously. We now show that being married is linked to a more optimal transition to kidney failure, with a higher likelihood of dialysis initiation in the outpatient setting with a pre-created access.
What can be done to mitigate these disparities in outcomes related to the transition from advanced CKD to kidney failure? We need to carefully re-examine the educational programs provided by CKD centres to inform patients about issues surrounding the transition to kidney failure (e.g. modality options, access creation, kidney transplantation). To adequately account for the diverse social backgrounds of our patients, these educational programs cannot take a ‘one-size-fits-all’ approach. Instead, they must be tailored in such a way to meet the unique needs of each patient on a case-by-case basis. Further, social determinants of health are ‘upstream’ factors that require improvement in the infrastructure of nephrology care as a whole if we hope to see an improvement. Broader health insurance coverage may improve access to nephrology care in certain regions of the world. However, it should be noted that this alone is likely insufficient, as our study was conducted in Canada where all residents are provided government-sponsored health coverage. Therefore we should additionally support policy reforms that limit the inequities experienced by our patients in regard to such factors as education, income and housing. Also, we should increase screening of our CKD patients for social needs that may be linked to their disease progression, outcomes and transition to kidney failure. In most centres, this screening for social needs occurs only late in the disease course once a patient has started on dialysis. If identified at an earlier disease stage, we could potentially allocate resources toward vulnerable patient populations that would assist them with navigating the healthcare system, thereby improving the quality and effectiveness of the care they receive. Only with such changes in our ‘upstream’ approach to caring for our CKD population are we likely to realize the ‘downstream’ benefits of more equitable outcomes.
We acknowledge several limitations within our study. First, this was a single-centre study, which may limit the generalizability of the findings. Our centre is unique in uniformly capturing the reported social determinant data for our advanced CKD population, which is not commonly done in other centres. Also, our study took place in Canada, where universal health coverage is available, which is not true for other regions of the world. The findings may also not generalize to low-income countries, where the barriers to access to care may be greater. Therefore the associations between social determinants of health and outcomes relating to the transition from advanced CKD to kidney failure may differ in other settings. Second, we focused exclusively on the social determinant factors of education level, employment status and marital status, as these were routinely captured as part of our clinic protocol. Other social determinants such as income level, literacy, housing status and neighbourhood environment were not studied, as we did not have specific details on these variables. Also, we did not explore race as a social determinant, as our patient population was predominantly white. Third, the number of patients receiving a pre-emptive kidney transplantation was relatively low, which limited our statistical power to detect significant differences based on social determinants of health.
In conclusion, social determinants of health including education, employment and marital status are associated with indicators of a suboptimal transition from advanced CKD to kidney failure. These outcomes include inpatient (versus outpatient) dialysis starts, pre-emptive (versus delayed) access creation and pre-emptive kidney transplantation. As a nephrology community, we must identify ‘upstream’ targets to improve care for our CKD population if we hope to achieve more equitable outcomes for our patients.
ACKNOWLEDGEMENTS
The authors acknowledge the individuals who assisted with data management at the Ottawa Hospital: Suzanne Jackson and Melanie Bujold.
FUNDING
G.L.H. is supported by the Canadian Institutes of Health Research Institute of Nutrition, Metabolism and Diabetes (reference PJT-183840) and the Lorna Jocelyn Wood Chair for Kidney Research. M.M.S. is supported by the Jindal Research Chair for the Prevention of Kidney Disease.
AUTHORS’ CONTRIBUTIONS
G.L.H., P.R., M.M.S. and A.A. were responsible for the research idea and study design. G.L.H. and A.A. were responsible for data acquisition and statistical analysis. G.L.H., P.R., M.M.S., D.Z., A.O.M., D.M., M.J.O., C.W., S.H. and A.A. were responsible for data analysis/interpretation. P.R., M.M.S., D.Z. and A.A. were responsible for supervision and mentorship. Each author contributed important intellectual content during manuscript drafting or revision, accepts personal accountability for the author's own contributions and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
DATA AVAILABILITY STATEMENT
The data underlying this article will be shared upon reasonable request to the corresponding author.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.





Comments