-
PDF
- Split View
-
Views
-
Cite
Cite
Ekaterina Parshina, Pavel Kislyy, Aleksei Zulkarnaev, Alexey Tolkach, MO816: Bone Turnover Markers as Risk Factors of Severe Hypocalcemia After Parathyroidectomy for Secondary Hyperparathyroidism, Nephrology Dialysis Transplantation, Volume 37, Issue Supplement_3, May 2022, gfac082.014, https://doi.org/10.1093/ndt/gfac082.014
Close - Share Icon Share
Abstract
Hungry bone syndrome is a common postoperative complication after parathyroidectomy (PTx) for severe secondary hyperparathyroidism (SHPT). We aimed to evaluate whether preoperative levels of serum alkaline phosphatase (AP) and β-crosslaps (CTX) are associated with the development of severe hypocalcemia after PTx for SHPT in dialysis-dependent patients.
The retrospective study included 127 severe SHPT dialysis-dependent patients who underwent subtotal (SPTx) or total parathyroidectomy with autotransplantation of parathyroid tissue (PTx + AT) in a single high-volume centre of endocrine surgery between 2011 and 2014. Severe postoperative hypocalcemia was defined as an ionized serum calcium level <0.9 mmol/L on a day 3 after surgery.
Severe hypocalcemia was observed in 83 (65.4%) patients after PTx. Comparing to those with mild hypocalcemia, hypoCa patients were significantly younger (mean age 44.2 ± 11.3 years versus 49.7 ± 10.4 years in a non-hypoCa group; P = .0089). Patients in two groups did not differ in terms of gender (P = .198), dialysis vintage (P = .24) and type of surgery (TPTx + AT or SPTx; P = .127). Preoperative PTH level was significantly higher in hypoCa group comparing to non-hypo Ca group [134 (Q1–Q3: 103–190) pmol/L versus 93.9 (Q1–Q3: 74.6–124.3) pmol/L, respectively; P < .0001]. In univariate analysis preoperative AP level was associated with the risk of postoperative severe hypocalcemia [363.2 (Q1–Q3: 180.9–726.3) IU in hypoCa group versus 142.1 (Q1–Q3: 97.2–223.7) IU in non-hypoCa group; P < 0.0001) (Figure 1). AP level above the cut-off value of 238.5 IU/L caused a 5-fold increase risk of severe hypocalcemia. We observed a moderate negative correlation between preoperative AP level and serum ionized calcium level on the third postoperative day after PTx {ρ = –0.637 [95% confidence interval (95% CI) –0.51 to –0.74]; P < .0001}. In contrast, preoperative CTX level was not associated with postoperative severe hypocalcemia [5.34 (Q1–Q3: 4.06–6.03) µg/L in hypoCa group versus 4.6 (Q1–Q3: 3.42–5.69) µg/L in non-hypoCa group; P = .191] (Figure 2). Moreover, the correlation between preoperative AP and CTX levels was weak, even though it was statistically significant [ρ = 0.27 (95% CI 0.08–0.44); P = .006]; and we observed no statistically significant correlation between preoperative CTX and PTH levels (P = .07).
The multivariate logistic regression revealed AP level as the only independent risk factor of severe hypocalcemia development after PTx [ОR 1.006 (95% CI 1.002–1.009) per each IU; P = .005].
We identified serum AP level, but not CTX, as an independent risk factor of severe hypocalcemia development after surgical treatment of SHPT. The correlation between CTX and other bone turnover markers (PTH, AP) is weak in dialysis-dependent patients with severe SHPT.
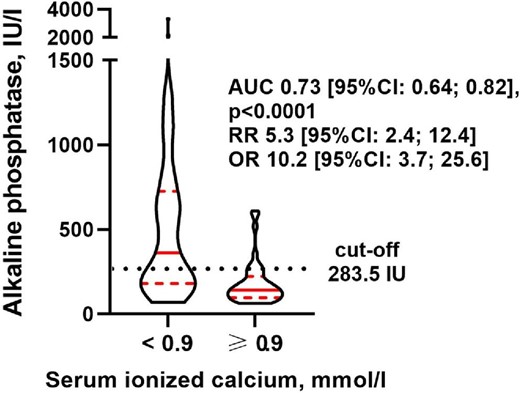
Preoperative total alkaline phosphatase levels in dialysis-dependent patients with and without severe hypocalcemia after parathyroidectomy. Medians, and first and third quartiles are depicted in red; the shape of the figures reflects the distribution. AUC-ROC, RR and OR for the cut-off value of 283.5 IU/L are given.
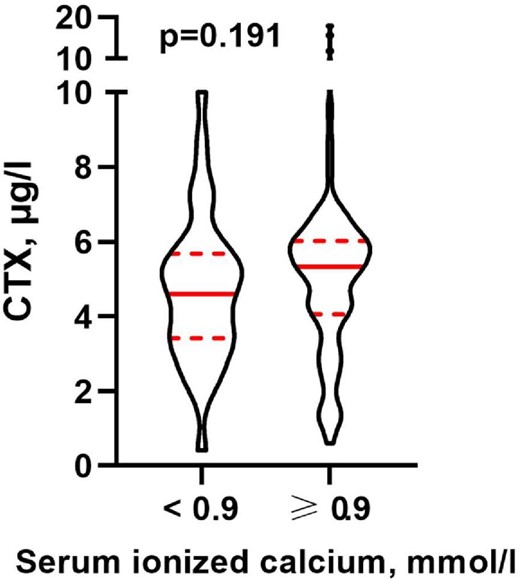
Preoperative β-crosslaps (CTX) levels in dialysis-dependent patients with and without severe hypocalcemia after parathyroidectomy. Medians, and first and third quartiles are depicted in red; the shape of the figures reflects the distribution.
- hemodialysis
- hyperparathyroidism, secondary
- hypocalcemia
- alkaline phosphatase
- postoperative complications
- endocrine surgical procedures
- parathyroidectomy
- pentoxifylline
- preoperative care
- surgical procedures, operative
- dialysis procedure
- gender
- hungry bones syndrome
- parathyroidectomy, complete
- parathyroid autograft
- bone turnover rate
- serum alkaline phosphatase measurement
- calcium test, serum
- ionized calcium measurement, serum
- univariate analysis





Comments