-
PDF
- Split View
-
Views
-
Cite
Cite
Aleksei Zulkarnaev, Vadim Stepanov, Andrey Vatazin, Aleksandr Fomin, Aleksandra Artamonova, Daria Penzeva, MO793: AVF Blood Flow Reduction in the Older Adults, Nephrology Dialysis Transplantation, Volume 37, Issue Supplement_3, May 2022, gfac080.030, https://doi.org/10.1093/ndt/gfac080.030
Close - Share Icon Share
Abstract
Older adults are approximately 40% of all prevalent HD patients (ERA-EDTA Annual report, 2019). Cardiovascular disease is the leading cause of death in this cohort. It is well-known that the cardiotoxic effect of arterio-venous fistula (AVF) is fully realized when cardio-fistula recirculation (CFR) is above 20–30%. We believe that the reduction of AVF blood flow (Qa) in the elderly is often less effective than in younger patients.
To evaluate the outcomes of Qa reduction in the elder and the younger HD patients.
The prospective cohort study included 21 patients ˃ 60 years and 36 patients ˂60 years: the median age was 74 years [interquartile range (IQR) 69; 78, min-max 64–81] and 41 years (IQR 35; 45, min-max 31; 55), respectively. In all patients, glomerular filtration rate (GFR) before reduction was more than 25%: 32.8% (IQR 29.2; 35.1, min-max 27.3; 38.9) and 33% (IQR 31; 35.125, min-max 27.1; 39.3), respectively. Qa reduction was performed by banding of the para-anastomotic AVF segment with intraoperative control (Doppler ultrasonography) until reaching Qa of 1.5 L/min or less.
In all patients, we noted a significant (P < 0.0001 in all cases) decrease in Qa as a result of the banding: in older adults from 2.1 L/min (IQR 1.9; 2.4, min-max 1.8; 2.8) to 1.2 L/min (IQR 1; 1.4, min-max 0.8; 1.5), delta Qa was −1 L/min (IQR −1.2; −0.9, min-max −1.5; −0.7), in younger patients from 2.8 L/min (IQR 2.5; 3.1, min-max 1.9; 3.5) to 1.3 L/min (IQR 1.1; 1.4, min-max 0.9; 1.5), −1.5 L/min (IQR −1.7; −1.3, min-max −2.3; −0.9], respectively.
In both elder and younger patients, we noted a significant decrease in CFR—Figure 1. However, after Qa reduction, only 5/21 elderly patients had CFR value less than 20%. Thus, 17/21 patients had CFR in the ‘gray zone’ —20–30%: 22.8% (IQR 21.85; 27.3, min-max 21; 29.2).
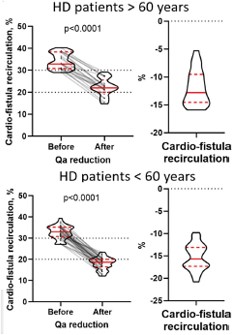
Changes in cardio-fistula recirculation as a result of Qa reduction in HD patients >60 and <60 years old.
In younger patients, 25/36 had CFR ˂ 20% after Qa reduction, while 11 stayed in the ‘gray zone’: 21.15% (IQR 20.575; 22.3, min-max 20.3; 23.4).
The probability of reducing CFR to a safe level (˂ 20%) after surgery was significantly less in the elder patients: RR = 0.3429 [95% confidence interval (95%CI) 0.1495; 0.6852], P = 0.0011.
We consider the lower baseline cardiac output in the elderly to be the main reason for the lower efficacy of Qa reduction: the difference between medians (older adults-younger patients before Qa reduction, Hodges–Lehmann method) was 1.9 L/min (95% CI 1.5; 2.4), P < 0.0001. At the same time, Qa before reduction did not differ much between the older and the younger: 0.6 L/min (95% CI 0.4; 0.8), P < 0.0001.
Moreover, the reduction of Qa in elderly patients led to a decrease in the ejection fraction (EF), which was not noticed in young patients—Figure 2. Notably, in all patients of both groups, the initial value of the EF was more than 55%.
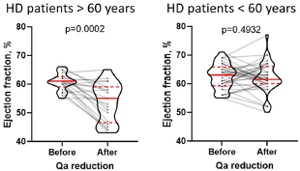
Changes in ejection fraction as a result of Qa reduction in HD patients >60 and <60 years old.
We believe that this can be explained by an abrupt increase in afterload against the background of a decreased compensatory heart capability in the elderly. At the same time, a decrease in the EF after Qa reduction in the elderly may indirectly indicate that conventional EF in the elderly is maintained by a presence of a high-flow AVF. Evaluation of EF against this background creates a putative picture of well-being and can mask the development of heart failure with reduced EF for a long time.
We noted a lower efficacy of Qa reduction as a method of reducing both cardio-fistula recirculation and cardiovascular risk in the elder patients compared to the younger patients on maintenance HD. Elder patients seem to require a different approach to reduce cardiovascular risk than younger patients.
- arteriovenous fistula
- cardiovascular diseases
- vascular flow
- cardiac output
- heart disease risk factors
- doppler ultrasound
- pathologic fistula
- glomerular filtration rate
- adult
- cause of death
- edetic acid
- intraoperative care
- masks
- personal satisfaction
- prospective studies
- surgical procedures, operative
- heart
- surgery specialty
- edetate disodium
- cardiotoxicity
- ejection fraction
- ventricular afterload
- older adult
- cardiac development
- fluid flow





Comments