-
PDF
- Split View
-
Views
-
Cite
Cite
Emily J See, Aminu K Bello, Adeera Levin, Meaghan Lunney, Mohamed A Osman, Feng Ye, Gloria E Ashuntantang, Ezequiel Bellorin-Font, Mohammed Benghanem Gharbi, Sara Davison, Mohammad Ghnaimat, Paul Harden, Htay Htay, Vivekanand Jha, Kamyar Kalantar-Zadeh, Peter G Kerr, Scott Klarenbach, Csaba P Kovesdy, Valerie Luyckx, Brendon Neuen, Donal O’Donoghue, Shahrzad Ossareh, Jeffrey Perl, Harun Ur Rashid, Eric Rondeau, Saad Syed, Laura Sola, Irma Tchokhonelidze, Vladimir Tesar, Kriang Tungsanga, Rumeyza Turan Kazancioglu, Angela Yee-Moon Wang, Chih-Wei Yang, Alexander Zemchenkov, Ming-Hui Zhao, Kitty J Jager, Fergus Caskey, Vlado Perkovic, Kailash K Jindal, Ikechi G Okpechi, Marcello Tonelli, John Feehally, David C Harris, David W Johnson, Availability, coverage, and scope of health information systems for kidney care across world countries and regions, Nephrology Dialysis Transplantation, Volume 37, Issue 1, January 2022, Pages 159–167, https://doi.org/10.1093/ndt/gfaa343
Close - Share Icon Share
Abstract
Health information systems (HIS) are fundamental tools for the surveillance of health services, estimation of disease burden and prioritization of health resources. Several gaps in the availability of HIS for kidney disease were highlighted by the first iteration of the Global Kidney Health Atlas.
As part of its second iteration, the International Society of Nephrology conducted a cross-sectional global survey between July and October 2018 to explore the coverage and scope of HIS for kidney disease, with a focus on kidney replacement therapy (KRT).
Out of a total of 182 invited countries, 154 countries responded to questions on HIS (85% response rate). KRT registries were available in almost all high-income countries, but few low-income countries, while registries for non-dialysis chronic kidney disease (CKD) or acute kidney injury (AKI) were rare. Registries in high-income countries tended to be national, in contrast to registries in low-income countries, which often operated at local or regional levels. Although cause of end-stage kidney disease, modality of KRT and source of kidney transplant donors were frequently reported, few countries collected data on patient-reported outcome measures and only half of low-income countries recorded process-based measures. Almost no countries had programs to detect AKI and practices to identify CKD-targeted individuals with diabetes, hypertension and cardiovascular disease, rather than members of high-risk ethnic groups.
These findings confirm significant heterogeneity in the global availability of HIS for kidney disease and highlight important gaps in their coverage and scope, especially in low-income countries and across the domains of AKI, non-dialysis CKD, patient-reported outcomes, process-based measures and quality indicators for KRT service delivery.
KEY LEARNING POINTS
What is already known about this subject?
health information systems (HIS) are fundamental tools for the surveillance of health services, estimation of disease burden and prioritization of healthcare resources;
the first iteration of the Global Kidney Health Atlas highlighted significant variability in the availability of HIS for kidney disease within and between countries; and
coverage of HIS for kidney disease was particularly poor in low resource settings and across the domains of acute kidney injury (AKI) and non-dialysis chronic kidney disease (CKD).
What this study adds?
this study goes beyond an examination of the availability of HIS to explore in detail the collection and reporting of clinical outcomes, process-based measures and quality indicators for service delivery, especially as they relate to kidney replacement therapy (KRT);
registries for KRT remain poorly available in low-income countries, while registries for AKI and non-dialysis CKD are scarce across all income groups. National registries are largely limited to high-income countries, while registries in low-income countries tend to operate at local or regional levels; and
major gaps in the scope of registries include infrequent measurement and reporting of patient-reported outcome measures, process-based measures and quality indicators for delivery of KRT. Fewer low-income countries collected these metrics compared with high-income countries.
What impact this may have on practice or policy?
establishing and strengthening HIS for kidney disease should be a national and international priority;
incorporating patient-reported outcomes, process-based measures and quality metrics into existing HIS infrastructure may improve the quality of care for patients with kidney disease; and
low- and lower-middle-income countries may require provision of financial support, technical expertise and mentorship by established systems to ensure success.
INTRODUCTION
Health information systems (HIS) play an essential role in health service monitoring and benchmarking by ensuring the timely availability of robust and reliable health data. Comprising registries, disease surveillance systems, facility databases and electronic health records, these systems can be used to quantify disease burden and outcomes [1,2], evaluate the quality and safety of care [3,4], develop and implement health-related policies [5–8], identify differences between and within health services and recognize areas that incur unnecessary healthcare costs [2,9–13]. Increasingly, HIS are also being utilized in the health research setting, where they have been successfully integrated into cohort studies and clinical trials to increase efficiency and reduce expenditures [14–16].
Variability in the availability of HIS for kidney disease within and between countries was reported by the first iteration of the Global Kidney Health Atlas (GKHA), especially in low resource settings [17]. This finding was not unexpected given the costs and resources required to establish and maintain such systems and is supported by earlier studies, which found that almost half of HIS for kidney disease were based in Europe [18–20]. The scope and content coverage of HIS for kidney disease has not been previously studied, but may be another important source of heterogeneity. Therefore, the objectives of this study were two-fold: first, to perform a temporal comparison of the availability, nature of provider participation and geographic coverage of kidney disease HIS with the 2017 GKHA and second, to comprehensively examine their scope, with respect to measurement and reporting of clinical outcomes, process-based measures and quality indicators.
MATERIALS AND METHODS
The second iteration of the GKHA was a multinational cross-sectional survey conducted by the International Society of Nephrology (ISN), which was administered electronically to representatives of all 182 countries with ISN affiliate societies between July and October 2018. Countries were grouped by World Bank income group classification. A comprehensive description of the sampling approach, survey development, data handling and statistical analysis is available in the GKHA methodology paper [21,22]. In short, a systematic search of the published literature and other data sources (including annual reports of kidney registries and databases) was undertaken to estimate the burden of kidney replacement therapy (KRT). Then, a survey questionnaire of three key opinion leaders from each country was carried out, to collect details on national kidney care practices. Further assistance from international contacts, collaborators, ISN leaders and regional board members was also sought to review the consistency of regional data. The project was approved by the University of Alberta research ethics committee (protocol number: PR000063121).
The questionnaire was designed in five modules that corresponded to each of the six building blocks of health systems towards universal health coverage. One module related specifically to HIS, which included registries, quality indicators and disease detection programs. Compared with the first iteration of the GKHA, the current survey focused in more detail on the global capacity and readiness to deliver KRT. Countries were asked to provide data on the availability and geographic coverage (national, regional or local) of their kidney disease registries, as well as the nature of provider participation (mandatory or voluntary). Information pertaining to the scope and content of registries was also requested, with specific questions tailored to each registry type: dialysis [etiology of end-stage kidney disease (ESKD), KRT modality, process-based measures, hospitalizations, patient-reported outcome measures and mortality]; transplantation (etiology of ESKD, transplant source, process-based measures, hospitalizations, patient-reported outcome measures and mortality); non-dialysis chronic kidney disease (CKD; coverage of all CKD stages or restriction to stages 4–5); and acute kidney injury (AKI; risk factors, etiology, incidence, hospitalizations, requirement for KRT and mortality). Patient-reported outcome measures were defined as health outcomes reported directly by the patient without interpretation of their response by others. They included satisfaction, fatigue, pain and quality of life. Process-based measures referred to markers of anemia, bone disease and blood pressure control.
The proportion of centres in each country that used a HIS to measure and report quality indicators for KRT was also explored. For hemodialysis and peritoneal dialysis, these indicators included patient-reported outcome measures (e.g. fatigue, quality of life, satisfaction and pain), blood pressure, small solute clearance (e.g.Kt/V and creatinine clearance), hemoglobin/hematocrit, bone mineral markers (e.g. calcium, phosphate and parathyroid hormone), technique survival and patient survival. For kidney transplantation, these indicators included patient-reported outcome measures, delayed graft function, rejection rates, renal allograft function, graft survival and patient survival.
To examine local practices for the screening and detection of kidney disease, the survey also explored whether specific ethnic groups were considered to be at increased risk for AKI and CKD, and whether detection programs based on national policy and/or guidelines existed. Countries were asked about whether cases of AKI or CKD were identified through a ‘reactive' approach (identification through routine practice), an ‘active, routine' approach (active screening of high-risk populations during routine health encounters) or an ‘active, specific' approach (active screening of high-risk populations through specific screening processes). Specific screening practices for CKD in the following high-risk groups were also covered: hypertension, diabetes, cardiovascular disease, autoimmune disease, elderly, urological disorders, chronic users of nephrotoxic agents, high-risk ethnic groups and family history of CKD.
RESULTS
Among 182 invited countries, 160 countries (88%) participated in the GKHA survey, comprising 97.8% of the world’s population. Of these, 154 countries responded to the questions about HIS (85%). Non-respondent countries were evenly distributed across regions and income groups and mostly represented smaller countries (Supplementary data, Table S1). Between the first and second iterations of the GKHA, the number of respondent countries providing information on HIS increased by 37. Complete details on the response rate and population coverage of the survey have been published elsewhere [22].
Availability of renal registries
The survey demonstrated wide variation in the availability of registries within and between ISN regions and World Bank income groups (Table 1 andFigure 1). Individual results according to country are presented inSupplementary data, Table S2. Despite finding that the majority of countries had dialysis registries (n = 101, 66%) and more than half had registries for transplantation (n = 88, 57%), few low-income countries had dialysis registries (n = 4, 18%) and none had registries for transplantation. Just 13 countries (8%) had registries for AKI, while non-dialysis CKD registries were only available in 19 countries (12%). There were no obvious differences in the availability of AKI or CKD registries between high- and low-income countries. Notably, few countries in South Asia had registries of any type. These figures are comparable to those reported by the first iteration of the GKHA, suggesting minimal improvement in registry availability in the 2 years between surveys.
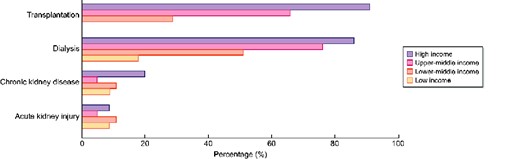
Percentage of countries with registries for AKI, non-dialysis CKD, dialysis and transplantation, by World Bank income group.
Availability of registries for AKI, CKD, dialysis and transplantation, by ISNregion (n = 154)
| Region . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| Overall | 13 (8) | 19 (12) | 101 (66) | 88 (57) |
| ISN region | ||||
| Africa | 4 (10) | 3 (7) | 18 (44) | 6 (15) |
| Eastern and Central Europe | 2 (11) | 1 (5) | 17 (89) | 17 (89) |
| Latin America | 1 (6) | 5 (28) | 14 (78) | 13 (72) |
| Middle East | 1 (9) | 1 (9) | 6 (55) | 8 (73) |
| NIS and Russia | 1 (14) | 2 (29) | 5 (71) | 6 (86) |
| North America | 0 (0) | 0 (0) | 4 (44) | 3 (33) |
| North and East Asia | 1 (14) | 2 (29) | 7 (100) | 7 (100) |
| OSEA | 1 (7) | 2 (13) | 10 (67) | 8 (53) |
| South Asia | 0 (0) | 0 (0) | 2 (29) | 1 (14) |
| Western Europe | 2 (10) | 3 (15) | 18 (90) | 19 (95) |
| Region . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| Overall | 13 (8) | 19 (12) | 101 (66) | 88 (57) |
| ISN region | ||||
| Africa | 4 (10) | 3 (7) | 18 (44) | 6 (15) |
| Eastern and Central Europe | 2 (11) | 1 (5) | 17 (89) | 17 (89) |
| Latin America | 1 (6) | 5 (28) | 14 (78) | 13 (72) |
| Middle East | 1 (9) | 1 (9) | 6 (55) | 8 (73) |
| NIS and Russia | 1 (14) | 2 (29) | 5 (71) | 6 (86) |
| North America | 0 (0) | 0 (0) | 4 (44) | 3 (33) |
| North and East Asia | 1 (14) | 2 (29) | 7 (100) | 7 (100) |
| OSEA | 1 (7) | 2 (13) | 10 (67) | 8 (53) |
| South Asia | 0 (0) | 0 (0) | 2 (29) | 1 (14) |
| Western Europe | 2 (10) | 3 (15) | 18 (90) | 19 (95) |
NIS, newly independent states; OSEA, Oceania and South East Asia.
Availability of registries for AKI, CKD, dialysis and transplantation, by ISNregion (n = 154)
| Region . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| Overall | 13 (8) | 19 (12) | 101 (66) | 88 (57) |
| ISN region | ||||
| Africa | 4 (10) | 3 (7) | 18 (44) | 6 (15) |
| Eastern and Central Europe | 2 (11) | 1 (5) | 17 (89) | 17 (89) |
| Latin America | 1 (6) | 5 (28) | 14 (78) | 13 (72) |
| Middle East | 1 (9) | 1 (9) | 6 (55) | 8 (73) |
| NIS and Russia | 1 (14) | 2 (29) | 5 (71) | 6 (86) |
| North America | 0 (0) | 0 (0) | 4 (44) | 3 (33) |
| North and East Asia | 1 (14) | 2 (29) | 7 (100) | 7 (100) |
| OSEA | 1 (7) | 2 (13) | 10 (67) | 8 (53) |
| South Asia | 0 (0) | 0 (0) | 2 (29) | 1 (14) |
| Western Europe | 2 (10) | 3 (15) | 18 (90) | 19 (95) |
| Region . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| Overall | 13 (8) | 19 (12) | 101 (66) | 88 (57) |
| ISN region | ||||
| Africa | 4 (10) | 3 (7) | 18 (44) | 6 (15) |
| Eastern and Central Europe | 2 (11) | 1 (5) | 17 (89) | 17 (89) |
| Latin America | 1 (6) | 5 (28) | 14 (78) | 13 (72) |
| Middle East | 1 (9) | 1 (9) | 6 (55) | 8 (73) |
| NIS and Russia | 1 (14) | 2 (29) | 5 (71) | 6 (86) |
| North America | 0 (0) | 0 (0) | 4 (44) | 3 (33) |
| North and East Asia | 1 (14) | 2 (29) | 7 (100) | 7 (100) |
| OSEA | 1 (7) | 2 (13) | 10 (67) | 8 (53) |
| South Asia | 0 (0) | 0 (0) | 2 (29) | 1 (14) |
| Western Europe | 2 (10) | 3 (15) | 18 (90) | 19 (95) |
NIS, newly independent states; OSEA, Oceania and South East Asia.
Provider participation in registries
The nature of provider participation varied by registry type and by World Bank income group (Table 2). Compared with the first iteration of the GKHA, more countries in this survey mandated provider participation in dialysis registries, including all low-income countries (n = 4, 100%) and two-thirds of high-income countries (n = 30, 63%). Similarly, the percentage of countries with mandatory provider participation in transplantation registries also increased between surveys, both in lower-middle (n = 5, 50%) and high-income (n = 37, 73%) countries. For AKI registries, provider participation was mandatory in 8 of 13 countries (62%); among the 19 countries with non-dialysis CKD registries, participation was mandatory in 10 countries (53%). Participation was voluntary for all available registries in South Asian countries.
Provider participation in registries for AKI, CKD, dialysis and transplantation, by World Bank income group (n = 154 countries)
| Participation . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| Mandatory | ||||
| Overall | 8 (62) | 10 (53) | 60 (59) | 57 (65) |
| Low income | 2 (100) | 2 (100) | 4 (100) | 0 (0) |
| Lower-middle income | 2 (50) | 3 (75) | 10 (56) | 5 (50) |
| Upper-middle income | 0 (0) | 1 (50) | 16 (52) | 15 (56) |
| High income | 4 (80) | 4 (36) | 30 (63) | 37 (73) |
| Voluntary | ||||
| Overall | 5 (38) | 8 (42) | 36 (37) | 26 (30) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 2 (50) | 0 (0) | 7 (39) | 3 (30) |
| Upper-middle income | 2 (100) | 1 (50) | 11 (35) | 9 (33) |
| High income | 1 (20) | 7 (64) | 18 (38) | 14 (27) |
| Missing or unknown | ||||
| Overall | 0 (0) | 1 (5) | 5 (5) | 5 (6) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 0 (0) | 1 (25) | 1 (6) | 2 (20) |
| Upper-middle income | 0 (0) | 0 (0) | 4 (13) | 3 (11) |
| High income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Participation . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| Mandatory | ||||
| Overall | 8 (62) | 10 (53) | 60 (59) | 57 (65) |
| Low income | 2 (100) | 2 (100) | 4 (100) | 0 (0) |
| Lower-middle income | 2 (50) | 3 (75) | 10 (56) | 5 (50) |
| Upper-middle income | 0 (0) | 1 (50) | 16 (52) | 15 (56) |
| High income | 4 (80) | 4 (36) | 30 (63) | 37 (73) |
| Voluntary | ||||
| Overall | 5 (38) | 8 (42) | 36 (37) | 26 (30) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 2 (50) | 0 (0) | 7 (39) | 3 (30) |
| Upper-middle income | 2 (100) | 1 (50) | 11 (35) | 9 (33) |
| High income | 1 (20) | 7 (64) | 18 (38) | 14 (27) |
| Missing or unknown | ||||
| Overall | 0 (0) | 1 (5) | 5 (5) | 5 (6) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 0 (0) | 1 (25) | 1 (6) | 2 (20) |
| Upper-middle income | 0 (0) | 0 (0) | 4 (13) | 3 (11) |
| High income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Provider participation in registries for AKI, CKD, dialysis and transplantation, by World Bank income group (n = 154 countries)
| Participation . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| Mandatory | ||||
| Overall | 8 (62) | 10 (53) | 60 (59) | 57 (65) |
| Low income | 2 (100) | 2 (100) | 4 (100) | 0 (0) |
| Lower-middle income | 2 (50) | 3 (75) | 10 (56) | 5 (50) |
| Upper-middle income | 0 (0) | 1 (50) | 16 (52) | 15 (56) |
| High income | 4 (80) | 4 (36) | 30 (63) | 37 (73) |
| Voluntary | ||||
| Overall | 5 (38) | 8 (42) | 36 (37) | 26 (30) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 2 (50) | 0 (0) | 7 (39) | 3 (30) |
| Upper-middle income | 2 (100) | 1 (50) | 11 (35) | 9 (33) |
| High income | 1 (20) | 7 (64) | 18 (38) | 14 (27) |
| Missing or unknown | ||||
| Overall | 0 (0) | 1 (5) | 5 (5) | 5 (6) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 0 (0) | 1 (25) | 1 (6) | 2 (20) |
| Upper-middle income | 0 (0) | 0 (0) | 4 (13) | 3 (11) |
| High income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Participation . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| Mandatory | ||||
| Overall | 8 (62) | 10 (53) | 60 (59) | 57 (65) |
| Low income | 2 (100) | 2 (100) | 4 (100) | 0 (0) |
| Lower-middle income | 2 (50) | 3 (75) | 10 (56) | 5 (50) |
| Upper-middle income | 0 (0) | 1 (50) | 16 (52) | 15 (56) |
| High income | 4 (80) | 4 (36) | 30 (63) | 37 (73) |
| Voluntary | ||||
| Overall | 5 (38) | 8 (42) | 36 (37) | 26 (30) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 2 (50) | 0 (0) | 7 (39) | 3 (30) |
| Upper-middle income | 2 (100) | 1 (50) | 11 (35) | 9 (33) |
| High income | 1 (20) | 7 (64) | 18 (38) | 14 (27) |
| Missing or unknown | ||||
| Overall | 0 (0) | 1 (5) | 5 (5) | 5 (6) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 0 (0) | 1 (25) | 1 (6) | 2 (20) |
| Upper-middle income | 0 (0) | 0 (0) | 4 (13) | 3 (11) |
| High income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Geographic coverage of registries
Nearly all dialysis registries were national, especially in high (n = 47, 98%) and upper-middle (n = 28, 90%) income countries (Table 3). Among low-income countries, two (50%) had national dialysis registries and one (25%) had a local dialysis registry. For transplantation, national registries were more commonly found in high (n = 43, 84%) or upper-middle (n = 26, 96%) income countries, rather than lower-middle-income countries (n = 6, 60%). Less than half of all AKI registries were national (n = 6, 46%), compared with more than two-thirds of non-dialysis CKD registries (n = 13, 68%). The percentage of countries with national non-dialysis CKD registries in this survey (n = 13, 68%) was much lower than the 89% of countries reported in the previous GKHA, suggesting that new non-dialysis CKD registries have tended to be regional or local.
Geographic coverage of registries for AKI, CKD, dialysis and transplantation, by World Bank income group (n = 154 countries)
| Geographic coverage . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| National | ||||
| Overall | 6 (46) | 13 (68) | 90 (89) | 75 (85) |
| Low income | 2 (100) | 1 (50) | 2 (50) | 0 (0) |
| Lower-middle income | 0 (0) | 2 (50) | 13 (72) | 6 (60) |
| Upper-middle income | 0 (0) | 1 (50) | 28 (90) | 26 (96) |
| High income | 4 (80) | 9 (82) | 47 (98) | 43 (84) |
| Regional | ||||
| Overall | 2 (15) | 4 (21) | 15 (15) | 9 (10) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 2 (50) | 2 (50) | 4 (22) | 2 (20) |
| Upper-middle income | 0 (0) | 0 (0) | 2 (6) | 0 (0) |
| High income | 0 (0) | 2 (18) | 9 (19) | 7 (14) |
| Local | ||||
| Overall | 4 (31) | 7 (37) | 13 (13) | 11 (13) |
| Low income | 0 (0) | 1 (50) | 1 (25) | 0 (0) |
| Lower-middle income | 2 (50) | 2 (50) | 4 (22) | 3 (30) |
| Upper-middle income | 1 (50) | 1 (50) | 2 (6) | 1 (4) |
| High income | 1 (20) | 3 (27) | 6 (13) | 7 (14) |
| Missing or unknown | ||||
| Overall | 1 (8) | 0 (0) | 13 (13) | 11 (13) |
| Low income | 0 (0) | 0 (0) | 1 (25) | 0 (0) |
| Lower-middle income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Upper-middle income | 1 (50) | 0 (0) | 0 (0) | 0 (0) |
| High income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Geographic coverage . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| National | ||||
| Overall | 6 (46) | 13 (68) | 90 (89) | 75 (85) |
| Low income | 2 (100) | 1 (50) | 2 (50) | 0 (0) |
| Lower-middle income | 0 (0) | 2 (50) | 13 (72) | 6 (60) |
| Upper-middle income | 0 (0) | 1 (50) | 28 (90) | 26 (96) |
| High income | 4 (80) | 9 (82) | 47 (98) | 43 (84) |
| Regional | ||||
| Overall | 2 (15) | 4 (21) | 15 (15) | 9 (10) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 2 (50) | 2 (50) | 4 (22) | 2 (20) |
| Upper-middle income | 0 (0) | 0 (0) | 2 (6) | 0 (0) |
| High income | 0 (0) | 2 (18) | 9 (19) | 7 (14) |
| Local | ||||
| Overall | 4 (31) | 7 (37) | 13 (13) | 11 (13) |
| Low income | 0 (0) | 1 (50) | 1 (25) | 0 (0) |
| Lower-middle income | 2 (50) | 2 (50) | 4 (22) | 3 (30) |
| Upper-middle income | 1 (50) | 1 (50) | 2 (6) | 1 (4) |
| High income | 1 (20) | 3 (27) | 6 (13) | 7 (14) |
| Missing or unknown | ||||
| Overall | 1 (8) | 0 (0) | 13 (13) | 11 (13) |
| Low income | 0 (0) | 0 (0) | 1 (25) | 0 (0) |
| Lower-middle income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Upper-middle income | 1 (50) | 0 (0) | 0 (0) | 0 (0) |
| High income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Some countries have registries with more than one type of geographic coverage.
Geographic coverage of registries for AKI, CKD, dialysis and transplantation, by World Bank income group (n = 154 countries)
| Geographic coverage . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| National | ||||
| Overall | 6 (46) | 13 (68) | 90 (89) | 75 (85) |
| Low income | 2 (100) | 1 (50) | 2 (50) | 0 (0) |
| Lower-middle income | 0 (0) | 2 (50) | 13 (72) | 6 (60) |
| Upper-middle income | 0 (0) | 1 (50) | 28 (90) | 26 (96) |
| High income | 4 (80) | 9 (82) | 47 (98) | 43 (84) |
| Regional | ||||
| Overall | 2 (15) | 4 (21) | 15 (15) | 9 (10) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 2 (50) | 2 (50) | 4 (22) | 2 (20) |
| Upper-middle income | 0 (0) | 0 (0) | 2 (6) | 0 (0) |
| High income | 0 (0) | 2 (18) | 9 (19) | 7 (14) |
| Local | ||||
| Overall | 4 (31) | 7 (37) | 13 (13) | 11 (13) |
| Low income | 0 (0) | 1 (50) | 1 (25) | 0 (0) |
| Lower-middle income | 2 (50) | 2 (50) | 4 (22) | 3 (30) |
| Upper-middle income | 1 (50) | 1 (50) | 2 (6) | 1 (4) |
| High income | 1 (20) | 3 (27) | 6 (13) | 7 (14) |
| Missing or unknown | ||||
| Overall | 1 (8) | 0 (0) | 13 (13) | 11 (13) |
| Low income | 0 (0) | 0 (0) | 1 (25) | 0 (0) |
| Lower-middle income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Upper-middle income | 1 (50) | 0 (0) | 0 (0) | 0 (0) |
| High income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Geographic coverage . | AKI,N (%) . | CKD,N (%) . | Dialysis,N (%) . | Transplantation,N (%) . |
|---|---|---|---|---|
| National | ||||
| Overall | 6 (46) | 13 (68) | 90 (89) | 75 (85) |
| Low income | 2 (100) | 1 (50) | 2 (50) | 0 (0) |
| Lower-middle income | 0 (0) | 2 (50) | 13 (72) | 6 (60) |
| Upper-middle income | 0 (0) | 1 (50) | 28 (90) | 26 (96) |
| High income | 4 (80) | 9 (82) | 47 (98) | 43 (84) |
| Regional | ||||
| Overall | 2 (15) | 4 (21) | 15 (15) | 9 (10) |
| Low income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lower-middle income | 2 (50) | 2 (50) | 4 (22) | 2 (20) |
| Upper-middle income | 0 (0) | 0 (0) | 2 (6) | 0 (0) |
| High income | 0 (0) | 2 (18) | 9 (19) | 7 (14) |
| Local | ||||
| Overall | 4 (31) | 7 (37) | 13 (13) | 11 (13) |
| Low income | 0 (0) | 1 (50) | 1 (25) | 0 (0) |
| Lower-middle income | 2 (50) | 2 (50) | 4 (22) | 3 (30) |
| Upper-middle income | 1 (50) | 1 (50) | 2 (6) | 1 (4) |
| High income | 1 (20) | 3 (27) | 6 (13) | 7 (14) |
| Missing or unknown | ||||
| Overall | 1 (8) | 0 (0) | 13 (13) | 11 (13) |
| Low income | 0 (0) | 0 (0) | 1 (25) | 0 (0) |
| Lower-middle income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Upper-middle income | 1 (50) | 0 (0) | 0 (0) | 0 (0) |
| High income | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Some countries have registries with more than one type of geographic coverage.
Content coverage of registries
Questions pertaining to the content of registries were included for the first time in this iteration of the GKHA. Almost all dialysis registries collected data on the modality of KRT (n = 96, 95%), as well as the etiology of ESKD (n = 91, 90%) and patient mortality (n = 83, 82%;Figure 2). When analyzed by income group, fewer low-income countries collected these metrics compared with high-income countries. Process-based measures for dialysis were recorded by registries in most high-income countries (n = 40, 83%), but by only half of registries in low-income countries (n = 2). Patient-reported outcome measures for dialysis were recorded by one-quarter of countries overall (n = 24, 24%).
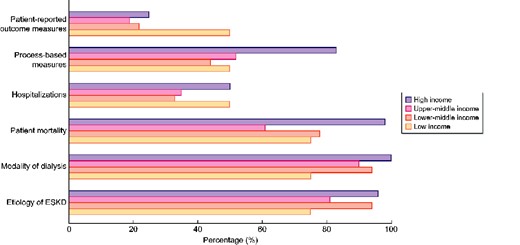
Percentage of countries with dialysis registries covering specific content, by World Bank income group.
With respect to transplantation registries, the majority of countries captured the donor source (n = 85, 97%), and most collected data on patient mortality (n = 76, 86%) and ESKD etiology (n = 75, 85%;Figure 3). Less than half of countries reported process-based measures for transplantation (n = 37, 42%) or hospitalizations (n = 36, 41%), and less than one-quarter of countries recorded patient-reported outcome measures for transplantation (n = 18, 20%), with no difference according to World Bank income group.
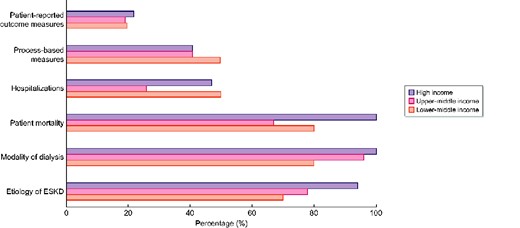
Percentage of countries with transplantation registries covering specific content, by World Bank income group.
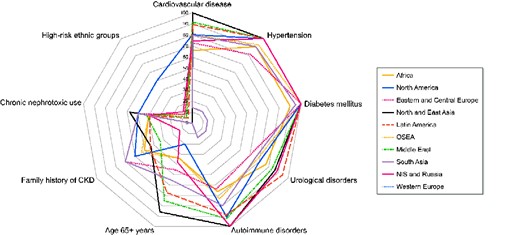
Percentage of countries adopting specific practices to identify CKD among individuals in high-risk groups, by ISN region.
Most countries with AKI registries collected data on its etiology (n = 10, 77%), incidence (n = 9, 69%), requirement for KRT (n = 9, 69%) and patient mortality (n = 9, 69%). Fewer countries with AKI registries reported AKI-related hospitalizations (n = 7, 54%) or risk factors (n = 6, 46%). Where available, non-dialysis CKD registries generally covered the whole spectrum of CKD (n = 12, 63%), with registries in five countries (26%) covering only advanced CKD (i.e. stages 4–5).
Measurement and reporting of quality indicators for KRT
Data pertaining to measurement and reporting of key quality indicators for KRT were also collected for the first time in this survey. Commonly measured and reported indicators for hemodialysis service delivery included blood pressure and hemoglobin/hematocrit, followed by small solute clearance, technique survival and patient survival (Supplementary data, Figure S1). The proportion of centres increased from low- to high-income countries across all parameters. With regard to peritoneal dialysis service delivery, blood pressure and hemoglobin/hematocrit were also frequently measured and reported, as was patient survival (Supplementary data, Figure S2). Technique survival and small solute clearance were not reported by many countries, especially those in low-income settings. For countries in which kidney transplantation was available, patient survival, graft survival and kidney allograft function were measured and reported more often than rejection and delayed graft function (Supplementary data, Figure S3). Patient-reported outcome measures for hemodialysis, peritoneal dialysis and transplantation were infrequently measured and reported by all countries, but especially in low- and lower-middle income settings.
Identification of high-risk groups
Information on how countries identified and/or screened patients for AKI and CKD was also collected. Just 6 countries (4%) had AKI detection programs in place and 35 countries (23%) had programs to detect CKD. Where available, the most common method of AKI detection was active screening, either through routine health encounters (n = 4, 67%), specific screening processes (n = 3, 50%) and/or a reactive approach (n = 2, 33%). High-income countries tended to implement CKD detection programs through a reactive approach (n = 8, 47%) or by active screening at routine health encounters (n = 7, 41%). The only low-income country with a CKD detection program also performed active screening during routine health encounters.
Very few low-income countries identified ethnic groups at higher risk for AKI (n = 3, 14%) or CKD (n = 0, 0%), compared with over one-third of high-income countries (n = 21 for AKI, 38%;n = 20 for CKD, 36%). Individuals with diabetes mellitus, hypertension, cardiovascular disease and urological disorders were more frequently screened for CKD than those of older age or high-risk ethnic group, those with a family history of CKD and chronic users of nephrotoxic medications (Figure 4).
DISCUSSION
This study goes beyond an examination of the availability of HIS for kidney disease to explore the measurement and reporting of clinical outcomes, process-based measures and quality indicators for service delivery, especially as they relate to KRT. Compared with the first iteration of the GKHA, it covered more countries and captured trends over time, including the presence of new registries. The findings of this study highlight key deficiencies in the availability, coverage and scope of HIS for kidney disease. Dialysis and transplantation registries remained poorly available in low-income countries, while AKI and non-dialysis CKD registries continued to be scarce across all income groups. Although an increasing number of countries mandated provider participation, national registries were still largely limited to the high-income setting. Major gaps in the scope of registries included the measurement and reporting of patient-reported outcomes, process-based measures and quality indicators for KRT service delivery. Almost no countries had AKI detection programs in place, while CKD detection programs were generally implemented through routine health encounters and targeted individuals with diabetes mellitus, hypertension and cardiovascular disease, rather than those from high-risk ethnic groups.
These findings have important implications for both low- and high-income countries [18,19]. First, the persistently low prevalence of KRT registries in low-income countries limits their access to local data on the epidemiology of ESKD and the outcomes of KRT, which impedes the delivery of accessible and cost-effective kidney care [8,23,24]. Second, significant gaps in the availability of AKI and non-dialysis CKD registries in both low- and high-income countries are concerning because both conditions occur commonly and are associated with substantial morbidity, mortality, resource consumption and healthcare costs [25,26]. AKI and non-dialysis CKD registries could provide useful information to monitor important trends in disease incidence, identify novel risk factors and document their natural history. They could also be used to anticipate the future demands on health resources relating to the development of ESKD, and to audit compliance with recommended management. Third, the paucity of countries incorporating patient-reported outcomes, process-based measures and quality indicators into their HIS leads to a lost opportunity to better understand the patient experience and perception of the quality of care. Patient-reported outcomes are increasingly recognized as important targets for therapeutic interventions [27], while process-based measures and quality indicators are useful tools for auditing the standard of care, benchmarking health services and identifying opportunities for improvement.
Addressing these gaps requires identification and prioritization of the areas of greatest need [28]. Because KRT is associated with substantial healthcare costs and significant variability in outcomes, establishing dialysis and transplantation registries is of high importance, since they could allow more efficient use of resources. For low-income countries, the cost of developing such registries could be minimized by either incorporating them into existing registries, expanding the coverage of local registries to a national scale or adapting established models for disease surveillance to local settings [29,30]. Increasing the availability of AKI and non-dialysis CKD registries could be achieved inexpensively through the use of electronic health records and administrative databases since both have a computable phenotype; linkage to hospitalization and mortality data could also be achieved using existing infrastructure [31,32]. In light of the potential cost associated with measuring and collecting patient-reported outcomes and process-based measures, identification of the outcomes of greatest importance to patients and clinicians is first necessary, which has been one of the key objectives of the Standardized Outcomes in Nephrology (SONG) initiative [33]. Where possible, validated tools should be used to ensure that the collected data are meaningful and comparable. The specific quality metrics selected for inclusion in the HIS should be individualized based on local relevance.
Prior to implementing changes to HIS infrastructure, consideration must be given to ensuring their quality, accuracy and security. This requires the availability of an adequate regulatory framework, trained and skilled personnel, financial and logistic support and a functioning information technology system. Data collection methods should be continuously monitored to assess quality, and instruments for secure data storage, processing and analysis must be in place [18]. HIS oversight should be transparent and any output should be accessible to individuals, clinicians, governing bodies and policy makers. Simple systems that do not overburden staff, but that allow comparisons between and within health services would be of particular benefit [34–36].
Establishing such systems in low-income countries presents a unique challenge [13,37,38]. Infrastructure for the diagnosis and screening of kidney disease may be unavailable or centralized in major towns, limiting rural residents’ access to testing. Collection of longitudinal data concerning disease prevalence and outcomes could be impeded by the migratory nature of some populations or by a lack of national census data for use as a reference population. A lack of trained personnel (i.e. data collectors, coders, analysts and epidemiologists) could also pose a barrier, and ongoing infrastructure and resource limitations could compromise HIS sustainability [29,39]. Strategies to address these challenges must be considered prior to the development or expansion of HIS in low resource settings.
This study has several key strengths. The GKHA is the most comprehensive report of global readiness and capacity for kidney care, and provides important and unique insights into the availability, coverage and scope of HIS for kidney disease. The survey was based on a well-validated framework for assessing care capacity that leverages the widely applied World Health Organization health system building blocks. Regional and national stakeholders with knowledge of local contexts carefully reviewed responses to ensure data accuracy. Participating countries represented nearly the entire global population, with excellent coverage across all ISN regions and World Bank income levels. Despite these strengths, this study also has certain limitations. A total of 15% of countries were missing, which may have impacted on the representativeness of the data or introduced bias. Population surveys are prone to subjective responses (i.e. social desirability bias) and depend on respondents’ knowledge and experiences. Additional aspects of HIS, such as quality, validity and regulation were beyond the scope of this study, but are important to consider when assessing an HIS’s value.
In summary, significant gaps remain in the global coverage of HIS for kidney disease, particularly in low-income countries, across the domains of AKI, non-dialysis CKD and in the measurement and reporting of patient-reported outcomes, process-based measures and quality indicators for KRT service delivery. Establishing and strengthening HIS should be a priority at both national and global levels to enable accurate estimation of the burden of kidney disease and to ensure that available resources are appropriately channelled to areas of greatest need. Financial and technical support for HIS in low- and lower-middle-income countries should be accelerated, and a collaborative approach with oversight and mentoring by established systems should be implemented to increase their likelihood of success. Integration of patient-reported outcomes, process-based measures and quality metrics into new and existing HIS could drive important improvements in the quality of kidney care.
SUPPLEMENTARY DATA
Supplementary data are available at ndt online.
ACKNOWLEDGEMENTS
The authors thank Sandrine Damster (Research Project Manager at the ISN) and Alberta Kidney Disease Network staff (G. Houston, S. Szigety and S. Tiv) for helping to organize and conduct the survey and providing project management support; Jo-Ann Donner (Awards, Endorsements, ISN-ANIO Programs Coordinator) for helping with the manuscript management and submission process; ISN staff (Charu Malik, Claire Van Der Linden, Luisa Straniand and Luca Segantini) for their support; the GKHA steering committee; the executive committee of the ISN; ISN regional leadership and the leaders of the ISN Affiliate Societies at the regional and country levels for their help, particularly with identification of survey respondents and data acquisition, which ensured the success of this initiative. None of the persons acknowledged received compensation for their role in the study.
FUNDING
This work was supported by the ISN (grant RES0033080 to the University of Alberta). Role of the funder/sponsor: the ISN provided administrative support for the design and implementation of the study and data collection activities. The authors were responsible for data management, analysis and interpretation, as well as manuscript preparation, review and approval, and the decision to submit the manuscript for publication.
CONFLICT OF INTEREST STATEMENT
D.W.J. has received consultancy fees, research grants, speaker’s honoraria and travel sponsorships from Baxter Healthcare and Fresenius Medical Care. He was supported by the National Health and Medical Research Council Practitioner Fellowship. H.H. has received research grants from Johnson & Johnson Company and Singhealth new investigator grant (NIG). A.Y.-M.W. has received speaker honoraria and travel grants from Sanofi Renal and Fresenius Kabi and research grants from Sanofi Renal and Baxter Healthcare. All other authors have no conflict of interest to declare.
DATA AVAILABILITY STATEMENT
The data underlying this article are available in the article and in its online supplementary material.
REFERENCES
- hypertension
- hemodialysis
- kidney diseases
- cardiovascular diseases
- diabetes mellitus
- renal transplantation
- kidney failure, chronic
- renal failure, acute
- cost of illness
- delivery of health care
- ethnic group
- health services
- income
- information systems
- nephrology
- quality indicators
- renal replacement therapy
- dialysis procedure
- kidney
- surveillance, medical
- low income
- patient self-report





Comments