-
PDF
- Split View
-
Views
-
Cite
Cite
Aurélie Sannier, Valentin Maisons, Mickael Bobot, Francois Vrtovsnik, Noemie Jourde-Chiche, Christophe Barba, Laurent Daniel, Nathalie Rioux-Leclercq, Cécile Vigneau, Jean-Michel Halimi, Jonathan Chemouny, MO646
PATHOLOGICAL PROGNOSTIC FACTORS IN DIABETIC NEPHROPATHY: A RETROSPECTIVE STUDY, Nephrology Dialysis Transplantation, Volume 36, Issue Supplement_1, May 2021, gfab094.0014, https://doi.org/10.1093/ndt/gfab094.0014Close - Share Icon Share
Abstract
Kidney Biopsies (KB) performed in patients with Type-2 diabetes (T2D) usually aim at differentiating diabetic nephropathy (DN) from other kidney diseases. However, KB could also help refining patients’ prognosis, both in terms of renal survival, and in terms of patient survival. In 2010, the Renal Pathology Society developed a pathological classification of DN, but the prognostic value of the described items , is still imperfectly documented. We aimed to assess the prognostic performances of these items to predict renal and patient survival.
Native KBs with diabetic and/or hypertensive nephropathy (DN/HN) performed in patients with T2D in four French centers were analyzed and scored according to the classification developed by the Renal Pathology Society. Clinical and biological data was collected from the patients’ records. Survival analyses were performed for renal survival (time to first dialysis or preemptive transplantation) and death after dichotomization of continuous data). For each of the analyses, we first established a model comprising clinical data only. We then assessed the benefit of adding each of the pathological item to the clinical model. Finally, we performed a backward stepwise analysis to identify items predictive of renal and/or patient survival.
We analyzed 165 biopsies with DN/HN from patients with T2D and with at least 12 months of follow-up (unless they reached an endpoint during the first year). Among them, 73 (44%) were male, 155 (94%) had hypertension, 53 (34%) hematuria, 22 (15%) had proliferative diabetic retinopathy (DR), 33 (23%) had non-proliferative DR, 90 (62%) had no DR (20 had missing data). Mean (SD) age was 63 (11), median [IQR] eGFRCKD-EPI was 29 [18;45] ml/min/1.73m², urinary protein-to-creatinine ratio was 0.38 [0.14;0.83] g/mmol, HbA1c was 7 [6.2;8.2] % and diabetes duration before KB was 10 [5;19] years. The median [IQR] follow-up was 33 months[18;57]. During the follow-up, 43 (26%) patients died and 69 (42%) required renal replacement therapy (RRT). The percentage of ischemic glomeruli, and presence of more than one area of arteriolar hyalinosis (ah=2), were predictive of renal survival and improved the predictive value of the model when added to clinical parameters. Presence of at least one convincing Kimmelstiel–Wilson lesion (nodular glomerulosclerosis or Class III DN) was predictive of death and similarly improved the predictive model (See figure).
Pathological findings on KB, as classified by the Renal Pathology Society, carry significant prognostic value in patients with T2D and DN/HN. Vascular lesions (presence of arteriolar hyalinosis and less than 7% of ischemic glomeruli) predicted the need for RRT, while nodular glomerulosclerosis was predictive of death.
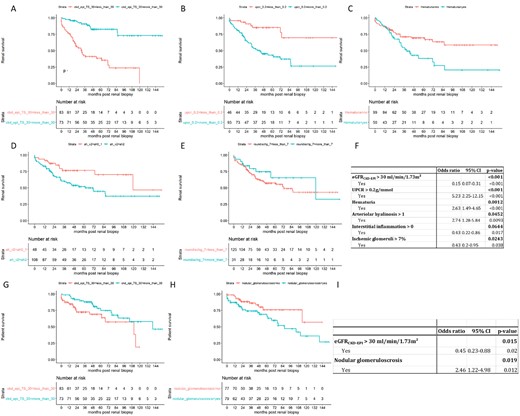
Upper and middle panels: Survival free of dialysis or preemptive transplantation according to (A) eGFRCKD-EPI below (red) or over (blue) 30 ml/min/1.73m², (B) UPCR below (red) or over (blue) 0.2 mg/mmol, (C) Hematuria absent (red) or present (blue), (D) Arteriolar hyalinosis 0-1(red) or 2 (blue), (E) Proportion of ischemic glomeruli below (red) or over (blue) 7%, (F) Adjusted Cox regression analysis for survival without dialysis of preemptive transplantation.
Lower panel: Patient survival according to (G) eGFRCKD-EPI below (red) or over (blue) 30 ml/min/1.73m², (H) Nodular glomerulosclerosis absent (red) or present (blue), (I) Adjusted Cox regression analysis for patients’ survival.
- ischemia
- hypertension
- hemodialysis
- kidney diseases
- diabetes mellitus
- diabetic nephropathy
- medical records
- diabetes mellitus, type 2
- biopsy
- creatinine
- hematuria
- follow-up
- hemoglobin a, glycosylated
- kidney glomerulus
- renal replacement therapy
- urinary tract
- dialysis procedure
- kidney
- pathology
- patient prognosis
- transplantation
- renal biopsy
- nodular glomerulosclerosis
- vascular lesions
- hyaline degeneration
- proliferative diabetic retinopathy
- prognostic factors
- cox proportional hazards models
- continuous data
- hypertensive nephropathy
- creatinine-based formula (ckd-epi)
- missing data





Comments