-
PDF
- Split View
-
Views
-
Cite
Cite
Raluca Popa, Radu Sascau, Cristian Statescu, Vlad Vasiliu, Andreea Neamtu, Andreea Bucur, Mehmet Kanbay, Dimitrie Siriopol, MO146
RENAL FUNCTION MEDIATES THE EFFECT OF FLUID EXCESS ON LUNG CONGESTION IN PATIENTS WITH HFREF, Nephrology Dialysis Transplantation, Volume 36, Issue Supplement_1, May 2021, gfab092.0024, https://doi.org/10.1093/ndt/gfab092.0024Close - Share Icon Share
Abstract
Despite impressive improvements in treatment strategies, heart failure (HF) morbidity and mortality remain substantially high worldwide. Pulmonary congestion is considered the leading cause for hospital admissions and death among patients with HF. The aim of this study is to investigate if the effect of fluid status, as assessed by bioimpedance spectroscopy (BIS) on lung congestion is mediated by renal function, inflammation or cardiac function.
This was a prospective observational study of outpatient adults referred for clinically indicated transthoracic echocardiograms at an academic hospital between 2016 and 2018. A left ventricular ejection fraction (LVEF) below 45% was required for inclusion (HFrEF).
Mediation is the process through which an exposure causes disease. We hypothesized that some of the total effect of extracellular water (ECW) to intracellular water (ICW) (as assessed by bioimpedance) ratio on lung congestion (as assessed by lung ultrasonography) is mediated by C-reactive protein (CRP), left atrium volum index (LAVI) or estimated glomerular filtration rate (eGFR) – the mediators.
Our study included 153 patients. The mean age and eGFR values of the population at baseline were 67.1 years and 66.5 ml/min/1.73m2. The mean median value for CRP was 25.6 (IQR 9.0-56.4) mg/L.
Figure 1 depicts the structural equation models with the calculated magnitude of the direct and indirect effects of ECW/ICW on the B-lines number in our population. In this model, the fluid status has both direct and indirect effects on lung congestion. Specifically, it has a direct effect on LAVI and eGFR, which in turn have a direct effect on the number of B-lines. Therefore, the indirect effect mediated by LAVI and eGFR accounts for a significant proportion of 27.6% of the total effect of ECW/ICW on lung congestion
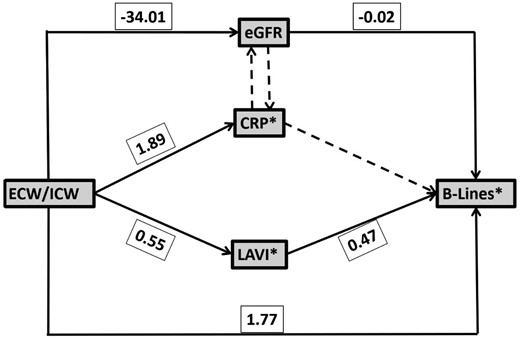
Path analysis illustrated by the structural equation model with standardized coefficients of direct effects for HFrEF patients. Dashed lines represent non‐significant pathways (tested, but not included in the model) and solid lines represent significant pathways (included in the model).
Although ECW/ICW has a direct effect on inflammation, this doesn’t have any effect on renal function or lung congestion.
We show that eGFR and LAVI partly mediate the effect of ECW/ICW on lung congestion in patients with HFrEF. While the deleterious effects of fluid overload on lung congestion have long been recognized, this study provides evidence for a relationship of significant magnitude linking fluid overload with decreased eGFR and increased LAVI, which in turn lead to elevations in the B-lines number.
This work was supported by a grant of the Ministery of Research and Innovation, CNCS-UEFISCDI, project number PN-III-P1-1.1-PD-2016-0287, within PNCDI III and by a grant of the “Grigore T. Popa” University of Medicine and Pharmacy, contract number 27505/2018.
- left ventricular ejection fraction
- left atrium
- inflammation
- renal function
- heart failure
- pulmonary congestion
- adult
- outpatients
- pharmacies
- spectrum analysis
- c-reactive protein
- morbidity
- mortality
- pharmacy (field)
- excess fluid volume
- echocardiography, transthoracic
- cardiac function
- hospital admission
- glomerular filtration rate, estimated
- bioelectrical impedance
- lung ultrasonography
- heart failure with reduced ejection fraction
- b-lines





Comments