-
PDF
- Split View
-
Views
-
Cite
Cite
Hanjie Zhang, Alhaji Cherif, Peter Kotanko, SO059
ASSOCIATION OF ALL-CAUSE MORTALITY WITH PRE-HEMODIALYSIS PULSE PRESSURE IN CHRONIC HEMODIALYSIS PATIENTS, Nephrology Dialysis Transplantation, Volume 35, Issue Supplement_3, June 2020, gfaa139.SO059, https://doi.org/10.1093/ndt/gfaa139.SO059Close - Share Icon Share
Abstract
Chronic and end-stage kidney disease patients experience significantly increased risk of cardiovascular morbidity and mortality due to multitude of interlinked pathophysiological processes inducing metabolic and inflammatory conditions. Pulse pressure (PP) reports cardiac and vascular conditions, where consistently high PP values are associated with atrial fibrillation, aortic insufficiency, arterial stiffness or arteriovenous malformation, and low PP values may be associated with aortic valve stenosis, cardiac insufficiency or cardiac tamponade. However, the association of pre-hemodialysis (pre-HD) PP with mortality among hemodialysis patients is not well understood. In this study, we aim to explore the extent to which PP is associated with mortality.
We analyzed pre-HD PP (calculated as pre-HD SBP minus pre-HD DBP) between 1/2001 and 12/2012 in hemodialysis patients treated in U.S. Fresenius Medical Care facilities. A 3-months baseline period was defined as months 4 to 6 after hemodialysis initiation, all-cause mortality was noted during follow-up. Only patients who survived baseline were included. Censoring events were renal transplantation, modality change, or study end. We built Cox proportional hazards models with spline terms, allowing us to model nonlinear effects of pre-HD PP as a continuous variable and its relationship with all-cause mortality.
We included 152,625 patients. Mean age was 60.8 years, 59% were white and 56% were male. During a median follow-up of 26.0 months 40.4% patients died. We found that for patients with pre-HD PP between 49.2 mmHg and 74.7 mmHg, were associated with better survival. In contrast, a PP below 49.2 mmHg and above 74.7 mmHg were associated with higher mortality. Similar nonlinear effects are seen in SBP for a given pre-HD PP value (see Fig. 1).
The association of pre-HD PP with mortality is nonlinear, and a better understanding of the nonlinearity will provide further insights into disentangling the associated mediators affecting its dynamics. Our findings may aid risk stratification in HD patients.
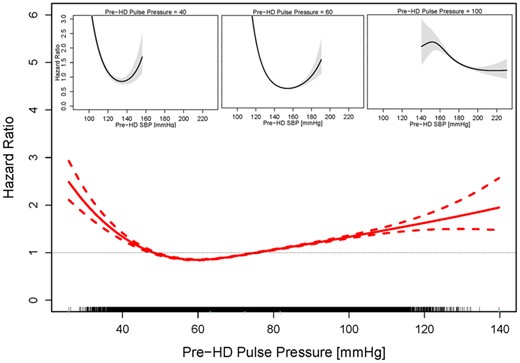
Figure 1: Association between pre-HD pulse pressure and all-cause mortality. HRs (solid line) and 95% CIs (dashed lines) of pre-HD pulse pressure. The tick marks on the x-axis represents individual patients.
- aortic valve insufficiency
- aortic valve stenosis
- congenital arteriovenous malformation
- atrial fibrillation
- cardiac tamponade
- hemodialysis
- renal transplantation
- kidney failure, chronic
- heart failure
- cardiovascular system
- follow-up
- heart
- morbidity
- mortality
- ticks
- arterial stiffness
- hemangioma, arteriovenous
- stratification
- pulse pressure
- interval data





Comments