-
PDF
- Split View
-
Views
-
Cite
Cite
Janani Rangaswami, Roy O Mathew, Raviprasenna Parasuraman, Ekamol Tantisattamo, Michelle Lubetzky, Swati Rao, Muhammad S Yaqub, Kelly A Birdwell, William Bennett, Pranav Dalal, Rajan Kapoor, Edgar V Lerma, Mark Lerman, Nicole McCormick, Sripal Bangalore, Peter A McCullough, Darshana M Dadhania, on behalf of the American Society of Transplantation’s Kidney-Pancreas Community of Practice (AST-KPCOP) Cardiovascular Disease Workgroup, Cardiovascular disease in the kidney transplant recipient: epidemiology, diagnosis and management strategies, Nephrology Dialysis Transplantation, Volume 34, Issue 5, May 2019, Pages 760–773, https://doi.org/10.1093/ndt/gfz053
Close - Share Icon Share
Abstract
Kidney transplantation (KT) is the optimal therapy for end-stage kidney disease (ESKD), resulting in significant improvement in survival as well as quality of life when compared with maintenance dialysis. The burden of cardiovascular disease (CVD) in ESKD is reduced after KT; however, it still remains the leading cause of premature patient and allograft loss, as well as a source of significant morbidity and healthcare costs. All major phenotypes of CVD including coronary artery disease, heart failure, valvular heart disease, arrhythmias and pulmonary hypertension are represented in the KT recipient population. Pre-existing risk factors for CVD in the KT recipient are amplified by superimposed cardio-metabolic derangements after transplantation such as the metabolic effects of immunosuppressive regimens, obesity, posttransplant diabetes, hypertension, dyslipidemia and allograft dysfunction. This review summarizes the major risk factors for CVD in KT recipients and describes the individual phenotypes of overt CVD in this population. It highlights gaps in the existing literature to emphasize the need for future studies in those areas and optimize cardiovascular outcomes after KT. Finally, it outlines the need for a joint ‘cardio-nephrology’ clinical care model to ensure continuity, multidisciplinary collaboration and implementation of best clinical practices toward reducing CVD after KT.
INTRODUCTION
Kidney transplantation (KT) is the treatment of choice for patients with end-stage kidney disease (ESKD) and is associated with improved outcomes and reduced mortality [1]. Although the survival benefit with KT is largely attributable to reduction in cardiovascular disease (CVD) burden (Figure 1), KT recipients continue to remain at higher risk for CVD-related morbidity and mortality when compared with the general population [3, 4]. Additionally, CVD represents the leading cause of death in KT recipients with a functioning allograft [5, 6]. The post-KT milieu represents the confluence of several traditional and nontraditional cardiovascular (CV) risk factors contributing to the significant CVD risk in this population [7]. KT recipients have a high prevalence of preexisting as well as de novo traditional CVD risk factors, such as hypertension (40–90% of patients) [8, 9], diabetes (24–42%) [10], dyslipidemia (50%) [11] and smoking (25%) [12]. Nontraditional risk factors include the adverse metabolic effects of immunosuppression, chronic anemia, hyperhomocysteinemia, chronic inflammation, proteinuria and chronic allograft nephropathy [13]. These risk factors result in increased risk of the entire spectrum of CVD, such as coronary artery disease (CAD), heart failure (HF), valvopathy, cerebrovascular disease, pulmonary hypertension (PH) and cardiac arrhythmias.
![Prevalence of CVD in adult end-stage renal disease (ESRD) patients, by treatment modality (2015). Special analyses, USRDS ESRD Database. Point prevalent hemodialysis, peritoneal dialysis and transplant patients aged ≥22 years, who are continuously enrolled in Medicare Parts A and B and with Medicare as primary prayer from 1 January to 31 December 2015, and ESRD service date is at least 90 days prior to 1 January 2015 [2]. The data reported here have been supplied by the USRDS. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US government. AMI, acute myocardial infarction; CVA/TIA, cerebrovascular accident/transient ischemic attack; PAD, peripheral arterial disease; VTE/PE, venous thromboembolism and pulmonary embolism; SCA/VA, sudden cardiac arrest and ventricular arrhythmias.](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/ndt/34/5/10.1093_ndt_gfz053/1/m_gfz053f1.jpeg?Expires=1750181055&Signature=Kxap2sl0K~leg0yCQSm~USP4JgW3UYevYWNqN5LO0PYs3f0m8YR4ZfbI3d9rUAgq39kzRNyu20cXiTaGlPvACd81tJhUM1~XHSK3Wf2vja7cn6OKY1TIoeeGMONNI1NFWlFRUkBIptjw-4aW7~LzjsLHHhzly3ObtVNLGOi0TJJ1Q-yxAg2ywj0Um67hCaD54sec8BsGEjY4tu6oAde0Dib8jW7V2TESSLwyNjpYAfIKjnjHdaHrMhxForZz1MtXrWUhDhjtuX6uNzyvj7rdJLP8pJ7nrq-f03SyE~x~eGnUR7nfpBZ1-ThoBrn-ycmhPOBHsE0r-OrP08bBaDF7Jg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Prevalence of CVD in adult end-stage renal disease (ESRD) patients, by treatment modality (2015). Special analyses, USRDS ESRD Database. Point prevalent hemodialysis, peritoneal dialysis and transplant patients aged ≥22 years, who are continuously enrolled in Medicare Parts A and B and with Medicare as primary prayer from 1 January to 31 December 2015, and ESRD service date is at least 90 days prior to 1 January 2015 [2]. The data reported here have been supplied by the USRDS. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US government. AMI, acute myocardial infarction; CVA/TIA, cerebrovascular accident/transient ischemic attack; PAD, peripheral arterial disease; VTE/PE, venous thromboembolism and pulmonary embolism; SCA/VA, sudden cardiac arrest and ventricular arrhythmias.
The current emphasis on post-KT care is preferentially centered around prevention of rejection and immunosuppression-related complications, with a less clearly defined agenda for prioritizing CVD-related morbidity and mortality as a modifiable outcome. Thus, while a CV evaluation is performed frequently pre-KT, the emphasis on CVD risk factor modification and disease management tends to fall into a ‘snapshot’ assessment pre-KT, rather than on a continuum from the pre-KT to the post-KT sphere. The management of CVD risk factors and disease phenotypes are further limited by the underrepresentation of patients with chronic kidney disease (CKD) and/or KT in major CV outcomes trials, thus resulting is less robust evidence-based practices and delivery of potentially beneficial therapies in this population [14]. In this review, we summarize the risk factors for CVD post-KT and their management. Next, we outline the various CVD phenotypes with pertinent data in the post-KT setting, as well as gaps in the existing literature. Finally, we describe barriers to delivery of optimal CVD care in patients with ESKD, and suggest a multidisciplinary ‘cardio-nephrology’ team approach that may optimize CVD care post-KT.
METHODOLOGY
Members of the American Society of Transplantation’s Kidney-Pancreas Community of Practice (AST-KPCOP) Cardiovascular Disease Workgroup held a series of teleconferences and web-based communications from July to November 2018 to (i) identify the topics to address in this comprehensive narrative on CVD in KT recipients, (ii) perform literature review and collate a bibliography using MEDLINE (1966–present) and the Cochrane Central Register of Controlled Trials as the primary sources for the literature search limited to human studies and the English language, (iii) identify key conference proceedings and relevant online data sources and (iv) create an outline for the manuscript and identify lead authors for each of the sections. Key relevant search words and medical subject heading (MeSH) descriptors are provided in the Supplementary table, S1. Preliminary drafts were collated into a single draft by two main authors (J.R. and R.O.M.) and distributed to the workgroup for edits prior to finalizing the submission. All authors had continuous access to the working document to provide input, critical review and revisions.
CARDIOVASCULAR AND METABOLIC RISK FACTORS AFTER KIDNEY TRANSPLANTATION
Hypertension as a risk factor
Hypertension following KT is both a result and cause of kidney allograft dysfunction; in addition, it is associated with adverse CV outcomes as well as premature CVD-related mortality [15, 16]. While treatment targets post-KT should probably be similar to those with CKD, there are no trials in post-KT patients comparing different blood pressure (BP) targets [17]. Kasiske et al. performed a retrospective cohort analysis of 1666 KT recipients and identified that each 10 mmHg of systolic blood pressure (SBP) increase was associated with 5% increased risk of allograft failure and death [8]. These data were recently validated in a recent post hoc study of the Folic Acid for Vascular Outcome Reduction in Transplantation (FAVORIT) cohort, which showed that every 20 mmHg increase in SBP over baseline was associated with a 32% increase in CVD and a 13% increase in mortality. Interestingly, a decrease in diastolic blood pressure (DBP) ≤70 mmHg was associated with CVD and mortality as well, while higher levels were not [18].
In addition to preexisting hypertension, transplant-related factors such as CKD stage posttransplant, vascular pathology and treatment with calcineurin inhibitors (CnI) and steroids are involved in the pathogenesis of de novo hypertension post- KT [13]. The use of CnI-based immunosuppressive regimens and steroid maintenance therapy have been associated with a high prevalence of post-KT hypertension [19]. In a meta-analysis of 34 randomized controlled trials (RCTs) comparing a maintenance steroid group with complete avoidance or withdrawal of steroids, Knight and Morris showed a reduced incidence in hypertension with steroid avoidance or withdrawal (SAW) [risk ratio (RR) 0.90; 95% confidence interval (CI) 0.85–0.94] [20]. However, the utilization of SAW for its potential benefits with hypertension and other cardio-metabolic risk factors [including posttransplant diabetes mellitus (DM) and hyperlipidemia] [20] must be weighed against the reported increased risk with acute rejection in pooled data analyses [20, 21]. Finally, despite a demonstrable benefit in long-term renal function with the use of belatacept-based immunosuppression, hypertension was still a significant factor in these KT recipients posttransplantation. In a pooled analysis of belatacept trials, only modest reductions in SBP and DBP were seen in those on belatacept compared with those on CnIs [22, 23].
Early post-KT BP targets tend to be more liberal (<160/90 mmHg) with the intention of maintaining optimal renal allograft perfusion and reducing the risk of renovascular thrombosis [17]. After the first month, BP control targets should mirror nontransplant CKD settings to reduce end organ damage [16]. The American College of Cardiology Foundation/American Heart Association 2017 Guidelines on Blood Pressure Management recommend a treatment target of <130/80 mmHg for post-KT recipients (IIa), as well as a recommendation to use calcium channel blockers as the initial drug of choice (IIa) on the basis of improved glomerular filtration rate (GFR) and allograft survival shown with this drug class [17, 24]. This is likely because of the known effects of intrarenal vasoconstriction and increased systemic vascular resistance with the usage of CnIs [25], which to some extent are reversed by calcium channel blockers [26]. Data supporting the use of angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) are inconsistent, with a large retrospective study of about 39 000 KT recipients in the Collaborative Study Cohort showing no difference in adverse CV events in the ACEI/ARB group versus other antihypertensive medications [27]. In contrast, another study suggested a cardiovascular benefit for ACEIs/ARBs may be seen, but not until a longer follow time of 10 years [28]. A meta-analysis of eight randomized trials of renin–angiotensin–aldosterone system inhibitors (RAASi) versus placebo/standard of care in KT recipients by Hiremath et al. [29] showed that RAASi did not significantly alter all-cause mortality (RR 0.96; 95% CI 0.62–1.51), transplant failure (RR 0.76; 95% CI 0.49–1.18) or creatinine level doubling (RR 0.84; 95% CI 0.51–1.39) compared with the control group [29]. There was significantly higher risk for hyperkalemia with RAAS blockade (RR 2.44; 95% CI 1.53–3.90). Given the concern for hyperkalemia and the potential to exacerbate pre-renal azotemia with the use of RAASi, the RAASi may be best reserved for the subset of post-KT recipients with hypertension and additional comorbidities that support the need for RAASi therapy (i.e. proteinuria or HF after KT). However, with appropriate potassium and estimated glomerular filtration rate (eGFR) monitoring, the use of RAASi has been demonstrated to be generally safe [30, 31]. The availability of the novel oral antihyperkalemic agents (patiromer and sodium zirconium cyclosilicate) may offer the opportunity to test the potential benefits of RAASi in the post-KT settings in a controlled fashion [32, 33]. It must be mentioned that there are limited data on the risk/benefit profiles of the novel antihyperkalemic agents in the post-KT setting, although small single center experiences have reported the ability to maintain target therapeutic tacrolimus levels with concomitant use of these drugs when administered as per labeling specifications [34].
Dyslipidemia and hyperhomocysteinemia: risk for atherogenic CVD
Dyslipidemia is highly prevalent post-KT, and is exacerbated by comorbid conditions such as obesity, posttransplant DM, proteinuria and immunosuppression, especially with the mammalian target of rapamycin (mTOR) inhibitors. In one of the first large randomized control studies of KT and CV outcomes, 2106 recipients were randomized to fluvastatin versus placebo in the Assessment of Lescol in Renal Transplantation (ALERT) study [35]. While low-density lipoprotein (LDL) was decreased by 32%, no difference was seen between groups in the primary composite outcome of adverse cardiac events after mean follow-up of 5.1 years (RR 0.83; 95% confidence interval 0.64–1.06). However, in a 2-year extension study, a long-term benefit was shown in the fluvastatin arm, with 35% relative reduction in the risk of cardiac death or definite nonfatal myocardial infarction (MI) [hazard ratio (HR) 0.65; 95% CI 0.48–0.88] [36]. The most recent Kidney Disease: Improving Global Outcomes (KDIGO) guidelines on dyslipidemia recommend treating all adult KT patients with a statin regardless of LDL concentration [37]. At this time, there are no data reported on the use of the proprotein convertase subtilisin/kexin-9 (PCSK9) inhibitors in KT recipients. Several classes of immunosuppressive agents including glucocorticoids and mTOR inhibitors have been associated with abnormal lipid profiles, including hypertriglyceridemia. Dose adjustments of these agents may improve dyslipidemia to some extent [38, 39]. Interestingly, a recent sub-study of the MECANO randomized trial spoke against increase in cardiovascular outcomes related to use of mTOR inhibitors versus CnI [40]. In this analysis of early transition to mTOR inhibitors from calcineurin inhibitors for graft preservation in 224 Dutch KT recipients, no differences were observed in predicted versus actual cardiovascular outcomes over 7 years following transplantation between the cyclosporine and everolimus groups. The majority of patients in both groups (>70%) received statins and had controlled BP. The findings of this study suggest that prior observational evidence of a possible increased cardiovascular risk profile with mTOR inhibitor use may have been confounded by indication (worsening renal function) or an overall higher risk profile of patients offered mTOR inhibitors.
Hyperhomocysteinemia is considered a nontraditional atherogenic risk factor, and is particularly prevalent in CKD [41, 42]. However, therapeutic manipulation of elevated homocysteine levels in advanced CKD and in the KT population has not shown reduction in CV clinical endpoints [43]. The FAVORIT trial randomized 4110 KT recipients with clinically stable and elevated homocysteine levels after 6 months post-KT to either a high-dose folic acid (5 mg), vitamin B6 (50 mg) and vitamin B12 (1000 μg), or low-dose vitamin B6 (1.4 mg) and vitamin B12 (2 μg) without folic acid [44]. After mean follow-up of 4 years, the high-dose multivitamin group did not have reduction in the primary composite arteriosclerotic CVD outcome of MI, stroke, CVD death, resuscitated sudden death, coronary artery or renal artery revascularization, lower extremity arterial disease, carotid endarterectomy or angioplasty, or abdominal aortic aneurysm repair compared with the low-dose multivitamin group (hazard ratio 0.99; 95% CI 0.84–1.17). Finally, a systematic review and meta-analysis also showed no cardiovascular benefits of homocysteine-lowering medication in patients with CKD, including KT [45]. Given the available evidence, homocysteine-lowing therapy as a primary cardiovascular prevention in advanced CKD, ESKD or post-KT is not currently recommended.
Tobacco use after KT and cardiovascular risk
Cigarette smoking has been associated with increased risk of CVD, malignancies, allograft failure and death in KT recipients. In fact, the negative impact of cigarette smoking on patient survival post-KT is similar to DM [46]. In a study of >1300 KT recipients, a smoking history of 11–25 pack-years was associated with increased relative risk of CV events of 1.56 [12]. The relative risk increased further to 2.14 with >25 pack-years of smoking. Li et al. recently reported the results of a tobacco smoking status survey administered across 2223 US dialysis centers [47]. Of 22 230 patients studied, 13% were active smokers. Mortality probabilities increased with greater exposure to smoking (17, 22, 23 and 27% for never, moderate, former and heavy smokers, respectively; P < 0.001), as did incidence rates for first hospitalization (23, 27, 27 and 30%, respectively; P < 0.001) Thus, KT candidates and recipients should be encouraged to quit smoking via nonpharmacological and pharmacological methods, including physician/provider-based brief advice strategies during office visits [48]. Although there are limited data on the impact of smoking cessation post-KT, it is a reasonable assumption that the KT recipient will also benefit from smoking cessation like the general population. Efforts should be made to screen annually for active cigarette smoking in potential and actual KT recipients, with targeted efforts to reduce the burden of cigarette smoking in this population. Table 1 summarizes the multidisciplinary approach to smoking cessation that is applicable to KT recipients.
| Psychosocial counseling | ||
| Sources of counselors |
| |
| Pharmacologic interventions | ||
| First-line pharmacotherapy | Mechanism of action | Clinical use |
| Nicotine replacement therapy |
| First line for pharmacologic intervention
|
| Sustained-release bupropion |
|
|
| Varenicline |
| Renally excreted, needs dose adjustment in patients with impaired renal function |
| Second-line pharmacotherapy | ||
| Nortriptyline | Noradrenergic actions substituting for the noradrenergic actions of nicotine receptor antagonist |
|
| Clonidine | α-2-adrenergic receptor agonist | Side effects including dry mouth and sedation is higher in the therapy group in a dose-dependent fashion |
| Psychosocial counseling | ||
| Sources of counselors |
| |
| Pharmacologic interventions | ||
| First-line pharmacotherapy | Mechanism of action | Clinical use |
| Nicotine replacement therapy |
| First line for pharmacologic intervention
|
| Sustained-release bupropion |
|
|
| Varenicline |
| Renally excreted, needs dose adjustment in patients with impaired renal function |
| Second-line pharmacotherapy | ||
| Nortriptyline | Noradrenergic actions substituting for the noradrenergic actions of nicotine receptor antagonist |
|
| Clonidine | α-2-adrenergic receptor agonist | Side effects including dry mouth and sedation is higher in the therapy group in a dose-dependent fashion |
| Psychosocial counseling | ||
| Sources of counselors |
| |
| Pharmacologic interventions | ||
| First-line pharmacotherapy | Mechanism of action | Clinical use |
| Nicotine replacement therapy |
| First line for pharmacologic intervention
|
| Sustained-release bupropion |
|
|
| Varenicline |
| Renally excreted, needs dose adjustment in patients with impaired renal function |
| Second-line pharmacotherapy | ||
| Nortriptyline | Noradrenergic actions substituting for the noradrenergic actions of nicotine receptor antagonist |
|
| Clonidine | α-2-adrenergic receptor agonist | Side effects including dry mouth and sedation is higher in the therapy group in a dose-dependent fashion |
| Psychosocial counseling | ||
| Sources of counselors |
| |
| Pharmacologic interventions | ||
| First-line pharmacotherapy | Mechanism of action | Clinical use |
| Nicotine replacement therapy |
| First line for pharmacologic intervention
|
| Sustained-release bupropion |
|
|
| Varenicline |
| Renally excreted, needs dose adjustment in patients with impaired renal function |
| Second-line pharmacotherapy | ||
| Nortriptyline | Noradrenergic actions substituting for the noradrenergic actions of nicotine receptor antagonist |
|
| Clonidine | α-2-adrenergic receptor agonist | Side effects including dry mouth and sedation is higher in the therapy group in a dose-dependent fashion |
Posttransplantation DM as a CVD risk factor
The development of posttransplantation diabetes mellitus (PTDM) and worsening of preexisting DM represent a major cardiovascular risk factor post-KT [49]. In a study of 1410 consecutive KT recipients observed for a median of 6.7 years (range 0.3–13.8 years), those with PTDM had higher all-cause and CV mortality [1.54 (1.09–2.17) and 1.80 (1.10–2.96)], while patients with impaired glucose tolerance (IGT) had higher all-cause, but not CV mortality [1.39 (1.01–1.91) and 1.04 (0.62–1.74)] compared with those with a normal glucose tolerance test [50]. CnIs are known to affect pancreatic beta cell function and the increased risk of PTDM with tacrolimus compared with cyclosporine was demonstrated in the DIRECT (Diabetes Incidence after Renal Transplantation: Neoral C(2) Monitoring Versus Tacrolimus) trial, which was a 6-month, open-label, randomized, multicenter study of 682 KT recipients randomized to cyclosporine (CsA) versus tacrolimus-based maintenance regimens [51]. The primary safety endpoint of PTDM or impaired fasting glucose (IFG) occurred in 26% of CsA-treated patients compared with 34% in tacrolimus group (P = 0.046). A recent randomized control study by Wissing et al. showed the benefit of switching tacrolimus to CsA in KT recipients who developed PTDM, with 34% of subjects in the CsA conversion group versus 10% in the tacrolimus continuation group resolving their PTDM (P = 0.01) [52]. However, it must be remembered that nephrotoxicity profiles associated with tacrolimus and CsA, albeit somewhat different, are still important and may have long-term consequences on the graft survival [53]. mTOR inhibitors, by reducing pancreatic beta cell proliferation and decreasing insulin sensitivity, may also increase the risk of PTDM [54]. The use of maintenance corticosteroids is another major risk factor for PTDM and patients on steroid-free regimens for a long term carry a 30% reduced risk overall of developing PTDM [55]. However, steroid withdrawal may not be beneficial based on data from a RCT of patients on chronic steroids versus early withdrawal, where 36% of subjects were diagnosed with PTDM at 5 years in both groups [56]. In a meta-analysis of RCTs comparing a steroid maintenance group versus complete avoidance or withdrawal in KT, Knight and Morris found a relative risk reduction for PTDM of 36% (RR 0.64; 95% CI 0.50–0.83); however, this benefit came with an increased risk of acute rejection when compared with the group on maintenance steroids (RR 1.56; 95% CI 1.31–1.87) [20]. The increased risk of rejection and a null signal for patient and allograft loss with steroid avoidance or withdrawal after KT was also confirmed in a Cochrane analysis by Haller et al. [21]. A systematic review and meta-analysis of six RCTs comparing KT outcomes between belatacept and CnI showed lower rates of PTDM at 12 months (odds ratio 0.43; 95% CI 0.24–0.78, P = 0.006, I2 = 18%) with the use of belatacept, in addition to better median eGFR at 12 and 24 months [23]. The risk/benefit analysis of using belatacept to reduce CVD risk post-KT must be weighed against potential risk for posttransplant lymphoproliferative disorder, especially in Epstein-Barr virus-negative recipients. Given the elevated CVD risk with PTDM, initiating screening for PTDM with glycated hemoglobin levels after 3 months post-KT is desirable, to provide early and goal directed management for reduction of cardio-metabolic risk after KT.
Obesity
Obesity at the time of KT is associated with both increased mortality as well as death-censored graft loss [57]. It exacerbates several other CVD risk factors, including hypertension, PTDM, dyslipidemia, metabolic syndrome and inflammation while still independently predicting increased adverse CV events [57, 58]. Additional weight gain post-KT is common, with an average weight gain of 5–10% in the first year, with age >45 years, female gender, African American ethnicity and preexisting obesity associated with highest risk [59]. The relationship between obesity and metabolic syndrome/PTDM after KT is complex and represents the confluence of preexisting metabolic risk with the superimposed effects of immunosuppressive regimens that may complicate glycemic control [60, 61]. For KT candidates, lifestyle changes should be strongly encouraged, with a role for bariatric surgery in selected patients to make otherwise good transplant candidates acceptable for the KT wait list. Though data for bariatric surgery are limited in patients with CKD, one study suggested that despite higher length of stay and reoperation rates, 30-day mortality was the same in CKD subjects when compared with those without CKD [62]. Emerging data suggest that bariatric surgery may be an effective and safe option for achieving a body mass index goal of <35 kg/m2 prior to transplantation [62]. Bariatric surgery following KT has also been associated with favorable clinical outcomes, notably improvements in glycemic and BP control [64]. A review by Camilleri et al. identified potential complications in the KT recipient, following bariatric surgery [64]. The greatest risk noted is the risk of hyperoxaluria and resultant nephrolithiasis or oxalate nephropathy [65]. The risk of hyperoxaluria and related problems appears to be most common after Roux-En-Y gastric bypass surgery. The risk following restrictive bariatric surgery (gastric banding or sleeve gastrectomy) appears to be much lower; however, longer term studies are needed to ensure that this conclusion is correct [64]. Thus, close monitoring of renal function would be required following bariatric surgery in a KT recipient, especially if bypass surgery is performed. Finally, immunosuppression dosing following bariatric surgery is less predictable [64]. Many immunosuppressants (tacrolimus, mycophenolate and sirolimus) may need increased dosing following bariatric surgery and close monitoring of levels of these medications should be undertaken if bariatric surgery is performed in a KT recipient. Figure 2 provides a summary of the management of traditional cardiovascular risk factors after KT.
ATHEROSCLEROTIC CARDIOVASCULAR DISEASE IN THE KIDNEY TRANSPLANT RECIPIENT
Recent reports indicate that noncardiovascular causes of mortality, specifically infection and malignancy combined, exceed CV mortality risk in KT patients with or without diabetes. This was explored in the FAVORIT study cohort by Weinrauch et al. [66]. In their analysis, the authors found that the long-term survival of KT recipients was significantly impacted by infectious and malignant complications as well as CV complications. However, the differences were small, and CVD, specifically atherosclerotic CVD, remained a major contributor to death with a functioning allograft. Thus, despite competing causes of mortality and adverse outcomes, CAD is an important cause of morbidity and mortality among KT recipients [67].
CAD is one of the targets of preoperative medical clearance among patients undergoing evaluation for KT [68]. CAD pre-KT increases the risk of the primary composite outcome of cardiovascular mortality, acute coronary syndrome (ACS) and need for revascularization after KT [69]. Noninvasive testing is the preferred initial screening modality for CAD, including dobutamine stress echocardiography and myocardial perfusion imaging; however, the predictive value of a positive noninvasive test for immediate posttransplant cardiovascular outcomes is unclear [70, 71]. Coronary angiography is a better predictor of posttransplant CVD-associated mortality, but the use of angiography is limited due to concerns about adverse events, especially renal injury in those not yet on dialysis [72]. However, it remains to be determined if preoperative risk stratification and ultimately revascularization, when indicated, will improve cardiovascular outcomes following KT. Two RCTs (Coronary Artery Revascularization Prophylaxis—CARP and the Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echo-V—DECREASE-V) demonstrated that there was no postoperative mortality or adverse CV event reduction with a prophylactic revascularization approach among patients with angiographically confirmed CAD or stress-induced ischemia about to undergo elective vascular surgery [73, 74]. The American College of Cardiology Foundation/American Heart Association 2012 Guidelines on the risk stratification of CVD prior to KT does not recommend routine revascularization in asymptomatic patients as part of the workup process for KT listing [75]. In a recent propensity score-matched analysis of 17,304 patients in the United States Renal Data System (USRDS) database transplanted between 2006 and 2013, stress testing in the 18 months prior to KT was not associated with a reduction in death, total MI or fatal MI within 30 days of KT after adjustment for differences in demographics and comorbidities [71]. That the stress tests were intended for screening as opposed to investigation of ischemic symptoms is supported by the low rate of coronary angiography (13.3%) and revascularization (2.1%) in the propensity-matched cohort. Nevertheless, once evidence of ischemic heart disease (typically by noninvasive cardiac stress testing) is found in the potential KT candidate, careful serial cardiovascular assessment must continue during wait-list time [76].
Naylor et al. have reported on overall stability in trends in early hospital readmission after KT between 2002 and 2014 despite increasing recipient age and comorbidities [77]. Despite these data, long-term CAD-related adverse events remain an important concern in KT recipients. Hypolite et al. explored the relationship of KT with ACS hospitalizations using information on ESKD patients on the wait list and within 3 years after transplantation [78]. Among diabetic patients, pretransplantation medical optimization and ultimately renal replacement therapy with a KT led to significant reductions in the incidence of hospitalization for ACS. Subsequent analyses have suggested the importance of preoperative CAD on long-term posttransplantation outcomes. Specifically, the presence of abnormal noninvasive stress testing and/or abnormal coronary angiography have been identified as predictors of long-term adverse outcomes, including cardiovascular outcomes, post-KT [79, 80]. In addition, the correction of angiographically significant CAD, with either percutaneous coronary intervention or coronary artery bypass grafting, is associated with improved long-term survival following KT than medical management [81]. A major limitation of the analyses is the observational nature of the studies and the inherent associated biases and confounders. Large prospective randomized studies will be needed to determine the efficacy of preoperative coronary revascularization on posttransplant cardiovascular outcomes.
Specific treatments for CAD in KT recipients have only been analyzed in a small number of studies. The ALERT trial did not demonstrate a significant difference in the primary combined CV endpoint (RR 0.83; 95% CI 0.64–1.06; P = 0.139) [35], but there was a significant reduction in the separate outcomes of cardiac death and nonfatal MI with fluvastatin therapy [0.65 (0.48–0.88); P = 0.005]. The cholesterol treatment trialists collaboration evaluated the ALERT trial as part of a large meta-analysis of trials examining cholesterol lowering among patients with CKD or on dialysis [82]. In this meta-analysis, the outcome of interest was major vascular event (major coronary event—nonfatal MI or death from coronary heart disease), coronary revascularization or stroke, and mortality, subdivided into vascular and nonvascular causes. The individual HR for this outcome identified for the ALERT trial was 0.76 (95% CI 0.64–0.92). In general, there seems to be little harm and likely cardiovascular benefit to initiating or continuing statin therapy in patients with a functioning KT.
Aspirin use has not been studied in a formal RCT in patients with a functioning renal transplant. Dad et al. performed a secondary analysis of aspirin use in the FAVORIT trial [83]. This was a post hoc analysis that found no benefit to baseline use of aspirin on multiple CVD-related outcomes or mortality, after propensity score matching. Currently, no clear recommendation can be made regarding aspirin use for primary prevention of CAD in KT recipients.
VALVULAR HEART DISEASE IN THE KIDNEY TRANSPLANT RECIPIENT
Echocardiographic evidence of valvular heart disease (VHD) in patients with CKD is common and appears to be more prevalent as eGFR decreases [84]. This observation is important as ESKD patients with severe VHD are often excluded from KT [85]. Characteristics of CKD patients that contribute to VHD include accelerated calcification, myocardial hypertrophy and increasing cavity size due to increased volume. There is a graded relationship between progressive decline in eGFR and the prevalence of calcification, hospitalizations, adverse CV events and death. It is not known if KT reverses valvular calcification. Kocyigit et al. examined the prevalence of aortic and mitral valve calcification in KT recipients [86]. Of 89 KT recipients examined, only 14 patients had no evidence of valvular calcification. Correlation analysis found no association of valvular calcification with either pre-KT dialysis vintage or post-KT duration. Further studies will be needed to identify the effects of KT on stabilization of preexisting valvular calcification and related morbidities.
It is not known if the progression of VHD is slower post-KT compared with pre-transplant status. However, progression of VHD over time is likely in patients with long-term kidney allografts and many will eventually need valve replacement. In a study by Abbott and colleagues, hospitalizations for VHD (aortic, mitral, tricuspid, pulmonic or combined) were lower among patients after KT as compared with before KT (0.68/1000 person-years and 0.84/1000 person-years, respectively) [85]. A study of valve surgeries between 1991 and 2004 by Sharma et al. showed that aortic valve replacement (66%) was most frequent, followed by mitral (25%), and only 9% underwent combined aortic/mitral valve repair [87]. Mitral valve replacement was associated with a higher risk of death as compared with aortic valve replacement. Additionally, the use of tissue valves versus non-tissue valves was associated with a lower mortality rate.
Aortic valve replacement has seen dramatic advances in recent years, particularly with the introduction of Transcatheter Aortic Valve Replacement/Implantation (TAVR/TAVI, hereafter will be referred as TAVR). Outcomes among patients with KT undergoing TAVR versus open surgical replacement have only been examined in retrospective analyses, with variable outcomes reported. Fox et al. reported minimal complications following TAVR in a small sample of 26 KT recipients comparing TAVR with surgical repair (one stroke at 12 months following TAVR) [88]. On the other hand, Al-Rashid et al. reported a series of cases from a single center in Germany in which KT recipients experienced a 2-year mortality following TAVR of 53%, as compared with 31% in patients with open surgical repair [89]. Larger studies will be needed to identify more reliable estimates of outcomes following TAVR in KT recipients.
HEART FAILURE IN THE KIDNEY TRANSPLANT RECIPIENT
HF is a major cause of morbidity and mortality in patients with ESKD, with a reported prevalence among dialysis patients of 12–36 times that of the general population [2, 90, 91]. The strong correlation between reduced ejection fraction (EF) and mortality was demonstrated by de Mattos et al. in a population selected for KT wait listing, such that every point increase in left ventricular EF (LVEF) was associated with a 2.5% decrease in adjusted mortality risk [92]. HF post-KT remains a major contributor to CVD-related hospitalizations after KT since 2005, with HF accounting for 16% of all hospitalizations [93]. Recent data suggest that while absolute rates of major adverse cardiovascular events (MACE) were stable over the period of 2004–13, 78% of all MACE (6.5% of the study population) were driven by HF [94]. Although preexisting cardiomyopathy impacts KT outcomes, a functioning KT can also influence the magnitude and clinical course of preexisting cardiomyopathy.
KT is associated with improvement in EF over time in most individuals. Wali et al. described a cohort of 103 patients with LVEF <40% (mean EF 31.6 ± 6.7%) with a median of two HF hospitalizations before KT evaluation with no inducible ischemia [95]. In this cohort, mean pre KT EF increased from 32% to 52% at 1 year of transplantation (P = 0.002). By 1-year post-KT, 72/103 (70%) patients had an EF of >50% and 16 patients improved their EF to 40–50%. Similar experiences have been reported in other single institution studies [96–98]. Another single center experience reported that KT patients with baseline mean EF of 35% had similar outcomes to those with normal EF in terms of graft and patient survival, largely due to improvement in EF post-KT [99]. These data suggest that restoration of eGFR and reversal of the uremic milieu may play a role in restoration or improvement of myocardial mechanics and function in patients with preexisting cardiomyopathy. This is further strengthened by observations showing improvement in global longitudinal strain (GLS) serially in children with CKD and maintenance dialysis, after KT [100]. However, in an analysis of left ventricular and right ventricular (RV) strain in subjects on maintenance dialysis with follow-up values post-KT (mean follow-up post-KT was 338 days) by Xu et al., biventricular strain abnormalities persisted post-KT even with preserved EF, thus suggesting that subclinical abnormalities in myocardial mechanics may persist even when other conventional measures of myocardial function such as EF are within normal range [101]. This also suggests that the duration required for recovery of strain abnormalities may extend to longer periods of time post-KT, warranting long-term follow-up and the use of goal-directed therapies for HF to optimize these findings, even beyond preservation/restoration of EF post-KT.
There are limited controlled data on the optimal pharmacotherapy of HF specific to KT recipients. Management of HF in the context of KT involves integrating available evidence-based therapies for HF in CKD (based on the degree of allograft function) as well as transplant-specific factors such as immunosuppressive agents. In terms of the potential differential effects of CnI versus mTOR inhibitors on cardiovascular effects, the open-label, Efficacy, Safety and Evolution of Cardiovascular parameters in Renal Transplant Recipients (ELEVATE) trial randomized KT recipients at 10–14 weeks after transplant to convert from CnI to everolimus or remain on standard CnI therapy [102]. The mean change in left ventricular mass index from randomization was similar with everolimus versus CnI, and mean pulse wave velocity remained stable with both everolimus and CnI. At Month 24, left ventricular hypertrophy was present in 42% versus 38% of everolimus and CnI patients, respectively. Major adverse cardiac events occurred in 1.1% and 4.2% of everolimus-treated and CnI-treated patients at 12 months (P = 0.018) and 2.3% and 4.5% at 24 months (P = 0.145), respectively. Thus, switching from a CnI to an mTOR-based regimen did not reduce prespecified cardiovascular metrics in this analysis, and the optimal immunosuppressive regimen in terms of hypertension and HF risk reduction is still a subject for future studies. This was additionally reviewed recently by Paoletti wherein the benefit of mTOR inhibitors on left ventricular mass appears to be BP independent and may also extend to reductions in arterial stiffness. Again, further studies will be needed to confirm such benefits [103].
There is conflicting evidence on the efficacy of RAASi and HF outcomes in KT recipients. The Study on Evaluation of Candesartan Cilexetil after Kidney Transplantation (SECRET) trial, which randomized 700 KT recipients to candesartan versus placebo, was terminated prematurely after mean follow-up of 20 months, due to a much lower than expected rate of the primary outcome of all-cause mortality, cardiovascular morbidity or graft failure [104]. In contrast, Paoletti et al. reported on 70 KT recipients on standard immunosuppression with CnI (CsA or tacrolimus), mycophenolate mofetil and steroids randomized to lisinopril versus usual care [28]. Event-free survival for a composite endpoint of death, major cardiovascular events, renal graft loss or creatinine doubling was better with ACEI but no significant differences in renal outcomes allograft loss. In a meta-analysis of eight trials examining clinical outcomes with RAASi in KT recipients by Hiremath et al. (only one trial specifically used HF as a primary outcome), no difference in all-cause mortality was observed with ACEI/ARB therapy versus placebo (RR for all-cause death 0.96; 95% CI 0.62–1.51; P = 0.9). There was significantly higher risk for hyperkalemia with RAAS blockade noted (RR 2.44; 95% CI 1.53–3.90) [29]. Currently, there are limited data on the impact of other goal-directed medical therapies including beta blockers, vasodilators and mineralocorticoid receptor antagonists on HF outcomes after KT, highlighting the need for future studies to define best strategies for the use of these agents in HF after KT.
The deleterious impact of preexisting and de novo HF on KT outcomes has been described in in large database analyses as well as single center investigations. Among 27 011 KT recipients whose outcomes were tracked in the USRDS database by Lentine et al. (1995–2011), the cumulative incidence of de novo HF was 10.2% at 12 months and 18.3% at 36 months [105]. De novo HF predicted death (HR 2.6; 95% CI 2.4–2.9) and death-censored graft failure (HR 2.7; 95% CI 2.4–3.0) in this report. Another analysis of the incidence de novo HF after KT over the period of 1998–2010 within the USRDS by Lenihan et al showed that the risk for developing de novo post-KT HF had declined significantly between 1998 and 2010, with no apparent change in subsequent mortality [106]. A recent study of 111 subjects showed that reduced GLS peritransplant is associated with increased risk of CVD events or death post-KT [107]. Patients who experienced an event were older, more frequently had a history of CAD and had higher left ventricular filling/longitudinal diastolic annular velocity (E/e′) than those who did not. GLS was significantly associated with event-free survival even after adjusting for age, sex, race–ethnicity, hypertension, diabetes, history of CAD or HF, and E/e′. Larger studies are needed in the future to define the incremental predictive value of GLS over clinical and other echocardiographic parameters for adverse CVD events following KT.
PULMONARY HYPERTENSION IN THE KIDNEY TRANSPLANT RECIPIENT
PH is a major comorbidity in patients with CKD and ESKD and has emerged as a major prognostic factor pre- and post-KT. PH is defined by a mean pulmonary artery (PA) pressure of 25 mmHg or more at rest, as measured by right heart catheterization (RHC) [108]. While RHC is the ‘gold standard’ for the diagnosis of PH, transthoracic echocardiography is the most commonly used technique to assess pulmonary pressures in practice, given the expensive and invasive nature of RHC [109]. In the absence of significant RV outflow obstruction, estimation of the RV systolic pressure (RVSP) from peak tricuspid regurgitation velocity allows the interchangeable use of RVSP and PA systolic pressure (PASP) in studies and clinical practice. The severity of PH based on PASP is classified as: normal, <35 mmHg, mild, 35–45 mmHg, moderate, 45–60 mmHg and severe, >60 mmHg.
The current World Health Organization classification of PH comprises of five groups, of which several underlying conditions that predispose to Groups 1–4 of PH are highly prevalent in CKD and ESKD [109]. The PEPPER study (PH in patients with CKD on dialysis and without dialysis) identified pre-capillary PH (pulmonary arterial hypertension in the absence of elevated PCWP) in 13% of patients (4/31) with RHC data before and after dialysis initiation [110]. Group 2 PH represents the most common type of PH in patients with CKD, given that left ventricular HF is estimated to affect 30–50% of patients with CKD [111]. Hypoxic lung disease that underlies the pathophysiology of Group 3 PH often coexists with CKD. These include unusually the high burden of obstructive sleep apnea (OSA), obesity and Chronic obstructive pulmonary disease (COPD) reported in CKD population [112, 113]. The 3- to 8-fold higher risk of pulmonary embolism reported in patients with CKD when compared with those without CKD, may contribute to chronic thromboembolic pulmonary hypertension (Group 4 PH) in these patients [114]. Finally, Group 5 PH encompasses unexplained PH in patients with CKD and ESKD, of which PH secondary to the hemodynamic effects of arteriovenous fistulae is an important etiology. Figure 3 briefly summarizes the approach to PH in the KT recipient. Detailed recommendations for the workup of PH in the potential/actual KT recipient are provided in the 2012 American Heart Association/American College of Cardiology Foundation Guidelines for the evaluation of PH among KT candidates as well as in a comprehensive summary by Lentine et al. [109, 115].
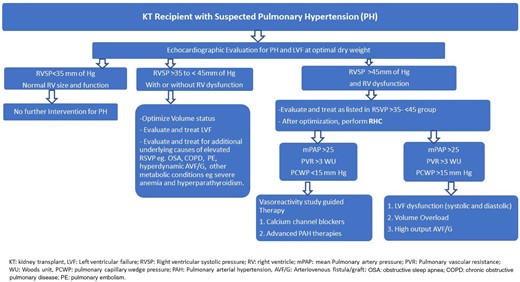
Clinical approach to the kidney allograft recipient with suspected pulmonary hypertension.
Issa et al. demonstrated that a pretransplant RVSP of >50 mmHg was independently associated with worse renal allograft outcomes, in a cohort of 215 KT recipients [116]. The HR for posttransplant death was 3.75 (P = 0.016) with RVSP values of >50 mmHg, with dialysis vintage being the strongest correlate with RVSP severity. In a cohort of 638 transplant recipients, patients with PH prior to transplant had a lower graft survival rate at 5 years versus patients without PH (54.6% versus 76.0%, P < 0.05) and were nearly twice as likely to experience overall graft failure [adjusted hazard ratio (AHR) 1.3; 95% CI 1.11–1.51] during the study period [117]. In a single-center cohort of 35 patients who underwent simultaneous heart kidney transplantation during 1996–2015, delayed graft function of the renal allograft occurred in 37% of patients, for which preoperative PH was identified as an independent risk factor [118]. These data demonstrate the importance of managing PH preoperatively in both kidney and heart–kidney allograft recipients.
ARRHYTHMIAS IN THE KIDNEY TRANSPLANT RECIPIENT
Patients with CKD have an increased risk for cardiac arrhythmias and sudden death given the unphysiological electrolyte balance associated with diminished renal function as well as the structural and functional changes that accompanied the uremic milieu [119, 120]. Atrial fibrillation (AF) represents the most common sustained arrhythmia in CKD [119]. In a study of over 60 000 Medicare patients, it was found that approximately 6.4% of patients were diagnosed with AF prior to KT [121]. A USRDS database analysis in 2006 demonstrated the 12- and 36-month incidence of new onset AF after KT to be 3.6% and 7.3%, respectively [122]. AF requiring hospitalization was shown to be associated with a 34% increase in all-cause mortality driven largely by CVD deaths in KT recipients in a historical cohort study of 39 628 subjects in the USRDS database. Similarly, Lentine et al. demonstrated that AF is also associated with an increased risk of death (AHR 3.2; 95% CI 2.9–3.6) and death-censored graft loss (AHR 1.9; 95% CI 1.6–2.3) [122]. In this analysis, risk factors for posttransplantation AF included older recipient age, male gender, white race, CKD from hypertension and CAD. Extended pretransplantation dialysis duration, PTDM and graft failure were also identified as potentially modifiable correlates of AF.
Patients with AF are typically on anticoagulation for stroke prevention and therefore many will require continued anticoagulation in the peritransplant period. Small series have demonstrated acceptable bleeding risk in patients who are on warfarin therapy at the time of transplant [123, 124]. There currently is a paucity of data on the use of the new direct oral anticoagulants (DOACs) and their safety in the peritransplant period. Careful consideration of the different DOACs and their dosing adjustments in renal impairment is critical to maintaining the safety profile of these drugs in transplant patients. In this context, the reader is directed to the summary from the recently concluded KDIGO consensus conference on CKD and arrhythmias for more details on DOAC dosing in CKD [119]. Apixaban and rivaroxaban have minimal drug interactions with tacrolimus, while dabigatran has potential for more significant interactions with CnIs, with CsA having more potential drug–drug interactions than those seen with tacrolimus [125]. CnI levels should be carefully monitored when using these newer medications. In addition, fluctuating renal function after transplant may alter the half-life of these drugs.
Ventricular arrhythmias are of increased concern after KT as they are associated with sudden death and poor outcomes in subjects with CKD [126]. The risk of sudden death in KT patients is reportedly as high as 15% [127, 128], and it is presumed that many of these deaths are related to ventricular arrhythmias. A single-center experience with electrophysiological monitoring in the early post-KT period demonstrated that ventricular arrhythmias occurred in as many as 30% of patients after transplantation [129]. Male gender, dialysis vintage and high preexisting coronary calcification scores were predictors of post-KT ventricular arrhythmias in this study. Higher quality data are needed to quantify the burden of post-KT ventricular arrhythmias to reduce the risk of sudden death in this population.
CONCLUSIONS AND FUTURE DIRECTIONS
CVD remains an understudied and undertreated source of morbidity and mortality in KT recipients. While the magnitude of disease burden is reduced when compared with patients on maintenance dialysis, it still remains a significant contributor to worse patient and allograft outcomes post-KT. Patients with CKD are generally excluded from major cardiovascular outcome trials, and this phenomenon of aversion to including patients with CKD in cardiovascular trials and providing appropriate goal-directed medical and interventional therapies (renalism) extends into KT [130, 131]. KT recipients continue to be undertreated with regards to cardiovascular risk factor management despite the well-known burden of CVD [132]. In addition, cardiovascular care is fragmented across the continuum of CKD, dialysis and transplantation, with shifting clinical care teams, variable screening protocols and lack of consensus on optimal management of CVD pre- and post-KT [133] (Figure 4). To this end, encouraging participation of KT recipients in cardiovascular trials will facilitate a better understanding of the nuances of CVD management in this unique population based on high-quality data. Public reporting of long-term allograft and patient outcomes will help potential KT recipients and referring nephrologists compare outcomes of patient with CVD, and thus set higher and competitive standards for optimizing long-term patient survival. Finally, encouraging ‘cardio-nephrology’ multidisciplinary clinical care models pre- and post-KT may help reduce care fragmentation and prioritize CVD screening and treatment [134]. These measures will help reduce the impact of CVD in KT recipients and optimize long-term patient and allograft outcomes in a cost-effective manner.
Care fragmentation in patients with cardiovascular disease before and after kidney transplantation.
ACKNOWLEDGEMENTS
This manuscript is a work product of the American Society of Transplantation's (AST) Kidney/Pancreas Work Group on Cardiovascular Disease. The Writing Group wishes to acknowledge the Education Committee of the American Society of Transplantation, staff members of the American Society of Transplantation and the Kidney/Pancreas Community of Practice and the peer reviewers for Nephrology Dialysis Transplantation for their valuable input and feedback with this project. The Writing Group also acknowledges Professor Carlos Zayas, MD, Director of Transplant Nephrology at Augusta University, Georgia for his input during the preparation of this manuscript.
CONFLICT OF INTEREST STATEMENT
None declared. The authors declare that this manuscript has not been published previously in whole or in part.
(See related article by Van Laecke and Abramowicz. Cardiovascular disease in kidney transplant recipients: leave no stone unturned. Nephrol Dial Transplant 2019; 34: 727--730)
REFERENCES
US Renal Data System. USRDS 2008 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases,
Badiou S, Cristol JP, Mourad G.
Kidney Disease: Improving global outcomes (KDIGO) Transplant Work Group.
Author notes
Janani Rangaswami and Roy O. Mathew authors contributed equally to this manuscript.



![Approach to the management of traditional cardiovascular risk factors in kidney transplant recipients [13, 17, 37]. HbA1C, glycosylated hemoglobin; ASA, aspirin; BMI, body mass index.](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/ndt/34/5/10.1093_ndt_gfz053/1/m_gfz053f2.jpeg?Expires=1750181055&Signature=Nm43uOLk2vqbVIRHEZ96jOxvTMwNOOmhdhivGml4mDpyf0SnkjSqeKHWUk7KUVw8PhR5Np6L7gcx0Vmn6wOBThVaS46cU2BEYkFtT9XIpPMdA5AMzTqnaS1JlUrAmf7fdxsfapBlwZju8SiWJLvEzNkLUFfU8FSih855bgSmZ2jFeaDeUq98jh5hheBSVFoNerXtddnDhD0MSrc8DeeNIACu4k1YVLiKU8xkb7HH0pGtwsJyHv~7wI2DDH09WvCeOgM-oZWxaDHnaB7ZuzZSKyd0esH2VWKHjbTpXcbchx3JCZxcN3f7vKL3dr25MA6ccoG-EM44zp1bDb1F4-WA7A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


Comments