-
PDF
- Split View
-
Views
-
Cite
Cite
Lukas Lehner, Fabian Halleck, Dmytro Khadzhynov, Eva Schrezenmeier, Klemens Budde, Oliver Staeck, SP730
THE EFFECT OF DELAYED GRAFT FUNCTION ON LONG TERM GRAFT SURVIVAL STRATIFIED BY KDPI BASED DONOR KIDNEY QUALITY CATEGORIES, Nephrology Dialysis Transplantation, Volume 32, Issue suppl_3, May 2017, Page iii387, https://doi.org/10.1093/ndt/gfx157.SP730Close - Share Icon Share
INTRODUCTION AND AIMS: Delayed graft function (DGF) is associated with impaired graft survival in kidney transplant recipients. The kidney donor profile index (KDPI) is increasingly evaluated as a prognostic tool to predict graft quality. However, there is few data that examined the contribution of DGF and donor kidney quality to impaired graft outcomes.
METHODS: This retrospective single center study included 580 adult patients who received a deceased donor kidney from 2000-2010. KDPI was calculated using OPTN data as reference and long-term outcomes (mean 8.0 years) were assessed.
RESULTS: Overall mean KDPI was 66%. Further categorization according to KDPI <35% (n=99), 35-85% (n=264) and >85% (n=217) resulted in a very high mean KDPI of 95% in the group with the highest KDPI. Due to the nature of the European Senior Program (ESP) this group showed a significantly higher recipient age (64 years compared to 47 and 48 years in the <35% and 35-85% groups, respectively). As expected, at 10 years patients living with functioning graft (71.9%, 58.5%, 31.3%) and death censored graft survival (86.7%, 76.9%, 55.6%) decreased with increasing KDPI (Fig.1 a,b). Intriguingly, rates of DGF <35%: 35.4%, 35-85%: 50.0%, >85% 53.9%) did not increase proportionally with higher KDPI. This might represent the ESP driven effect by local allocation of kidneys ≥65 years in order to lower cold ischemia time. However, DGF had a significant negative effect on long term graft survival in all KDPI categories (Fig.1 c,d). A multivariate Cox regression analysis adjusted for KDPI and cold ischemia time revealed DGF as an independent risk factor for premature graft loss (HR 1.97, p<0.001).
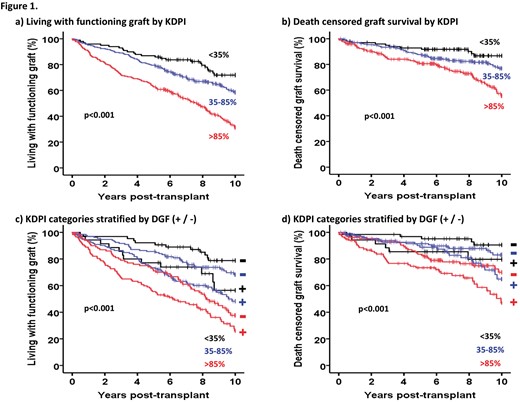
SP730 Figure





Comments