-
PDF
- Split View
-
Views
-
Cite
Cite
Ben Wong, Lorraine Venturato, Matthew J. Oliver, Robert R. Quinn, Pietro Ravani, Jayna Holroyd-Leduc, Selection of peritoneal dialysis among older eligible patients with end-stage renal disease, Nephrology Dialysis Transplantation, Volume 32, Issue 2, February 2017, Pages 384–392, https://doi.org/10.1093/ndt/gfw367
Close - Share Icon Share
Abstract
Background: Older patients with end-stage renal disease (ESRD) are less likely to choose peritoneal dialysis (PD) over hemodialysis (HD). The reasons behind their choice of dialysis modality are not clear. This study seeks to determine the patient-perceived factors that influence ESRD patients' choice of dialysis modality among older ESRD patients who are deemed eligible for both PD and HD.
Methods: All patients had completed a multidisciplinary modality assessment, were deemed eligible for both PD and HD, and had received modality education. Semi-structured interviews were conducted and transcripts were read repeatedly to derive potential codes using line-by-line textual analysis. The Capability, Opportunity, Motivation – Behaviour (COM-B) and Theoretical Domain Framework (TDF), validated tools that were developed for designing behavioral change interventions, were used to help guide the coding framework.
Results: Among older ESRD patients who are deemed eligible for both PD and HD, factors relevant to their modality decision-making were identified with respect to physical strength/dexterity and having a sound mind (capability), external forces and constraints (opportunity), and values and beliefs (motivation). Often a combination of factors led to an individual's choice of a particular dialysis modality. However, preferences for PD were primarily based around convenience and maintaining a normal life, while a heightened sense of security was the primary reason for those who selected HD.
Conclusions: We have identified patient-perceived factors that influence choice of dialysis modality in older individuals with ESRD who are eligible for PD and HD. These factors should be considered and/or addressed within PD programs seeking to promote PD.
INTRODUCTION
People aged 75 years and older represent the fastest growing segment of the dialysis population [1]. Despite the potential advantages of peritoneal dialysis (PD), it is an under-utilized therapy in most jurisdictions, particularly among older patients [2]. The reasons why older end-stage renal disease (ESRD) patients are less likely to choose PD are not clear. Previous studies have been conducted to explore the influences and specific factors that patients identify as significant in choosing a specific dialysis modality [3–14]. However, most of these studies did not specifically focus on patients who have been systematically determined to be eligible for both dialysis modalities (defined as absence of any contraindications), provided uniform modality education, and allowed to choose either PD or hemodialysis (HD). Inherently, patients' perceptions identified through these studies may be clouded by their lack of choice, their underlying contraindicating physical and social factors, and variations in modality education. Moreover, previous studies included mostly younger patients whose perceptions about dialysis modalities may differ from those of older patients. Finally, most studies included prevalent HD and PD patients. Patients' perceptions may change over time and they may not necessarily recall their initial reasons for choosing a particular dialysis modality. It is therefore important to identify patient-perceived factors that influence their choice of dialysis modality at or close to the time that they make decisions.
Focusing on a specific cohort of patients who have been determined to be eligible for both PD and HD by a multi-disciplinary team (consisting of nephrologists, nurses and social workers) provides an opportunity to help clarify potential patient-level barriers to PD choice. The study objective was to determine potential biases and misconceptions from the perspective of the patient, exploring potential reasons why older ESRD patients choose PD less often than would be expected based on eligibility.
MATERIALS AND METHODS
Participants
A convenience sample of participants were chosen from Sunnybrook Health Sciences Centre in Toronto, Canada to include a roughly proportionate mix of pre-dialysis/dialysis patients deemed eligible for both dialysis modalities, and who had chosen HD or PD (either continuous ambulatory PD or continuous cycling PD), or who were as yet undecided. Sixteen semi-structured face-to-face interviews were conducted with eligible patients. The study was approved by the Research Ethics Board of Sunnybrook Health Sciences Centre in Toronto, Canada and the Conjoint Health Research Ethics Board of the University of Calgary.
All patients had completed a multidisciplinary modality assessment, were deemed eligible for both PD and HD, and had received modality education. Dialysis modality education was not designed in any way to ‘sell’ home dialysis and it was reviewed to ensure both dialysis modalities were presented in an unbiased manner. As part of dialysis modality education, all patients met with a designated modality coach, who is a registered nurse hired specifically to educate pre-dialysis patients. During the initial session, lasting 60–90 min, patients were introduced to an introductory PowerPoint module, which covered the various treatment options (PD, HD, home HD, conservative care). The module consisted of both simple texts and pictures, and covered the advantages and disadvantages of each of the respective modalities. If interested, patients were also given a tour of the HD unit and/or the home dialysis unit (where the patient could see a PD machine). Patients were then asked to return for a second session with the designated modality coach, during which patients were exposed to a PowerPoint module(s) focusing on their specific dialysis modalities of interest. The designated modality coach also ensured that all patients were given an information binder from the Kidney Foundation of Canada, which covered all aspects of living with chronic kidney disease (CKD), including diet, medications and dialysis. The majority of patients would already have received the information binder from the CKD clinic.
Pre-dialysis patients and those who had initiated dialysis within the preceding 6 months were included in the study. Additional inclusion criteria included: (i) medical stability with no acute medical problems or hospitalizations within the preceding month, (ii) no obvious significant cognitive impairment, (iii) English-speaking, (iv) 65 years of age or older and (v) willingness to provide informed consent.
Research approach
A semi-structured interview protocol (Supplementary data, Item S1) was used to guide the interviews, with questions designed to focus on the following areas: (i) perceived advantages/disadvantages of HD and effect on quality of life (ii) perceived advantages/disadvantages of PD and effect on quality of life and (iii) decision-making process used for modality selection and exploration of internal/external factors that influenced the decision. Prior to conducting the interviews, we revised the interview protocol iteratively based on feedback from physicians and nurses with relevant content knowledge.
Collectively, the research team, consisting of nephrologist researchers, a geriatrician researcher in knowledge translation, and a qualitative nurse researcher, is experienced in conducting qualitative research. An Independent Dialysis Navigator at Sunnybrook Health Sciences Centre provided the interviewer (B.W.) with a list of eligible patients. The interviewer is a nephrologist who was working on his Masters degree in Health Services Research. This study forms part of his thesis work. He was not involved in the care of the patients at Sunnybrook Health Sciences Centre and had not met any of the patients prior to the beginning of the study. The interviewer approached these patients in person regarding participation in the study, explained the study purpose, and obtained informed written consent from those interested.
Pre-dialysis patients who had selected a preferred dialysis modality and current HD and PD patients were interviewed until data saturation was reached [15]. All interviews lasted between 30 and 60 min and were held in a PD unit, HD unit or clinic room. Interviews were digitally audio-recorded, and transcribed verbatim with standard linguistic conventions for analysis. Transcripts were entered into NVivo, version 10.2 (QSR International), a computer software used to store, code and search data. Transcripts were read repeatedly to derive potential codes using line-by-line textual analysis (B.W.). The Capability, Opportunity, Motivation – Behaviour (COM-B) and Theoretical Domain Framework (TDF) were used to help guide the coding framework [16, 17]. The coding framework, along with supporting quotes, was reviewed and verified by two additional researchers (J.H.-L. and L.V.).
Potential barriers to implementing practice change (including professional and other health-related behaviors) can be explored using the TDF [17]. The TDF framework comprises 14 domains of theoretical constructs and had been validated for use in behavior change and implementation research. As an extension of the TDF, the COM-B system and behavior change wheel were developed as a method of mapping potential barriers to appropriate behavior change interventions [16]. The COM-B system involves three essential conditions: Capability (physical and psychological), Opportunity (social and physical) and Motivation (automatic and reflective). We believe this framework is appropriate in guiding the development of a coding scheme applicable to the evaluation of dialysis modality selection that is guided by patient choice. Previous studies have identified that patients often perceive a lack of choice in decision-making across all treatments for CKD [14]. All patients in our study were provided both PD and HD modality education and invited to choose a preferred dialysis modality. The assumption is that natural behavior stems from free choice.
RESULTS
We interviewed a total of 16 patients, half of whom were females. Three additional patients also satisfied the study inclusion criteria, but were uninterested in study participation. While most patients selected a dialysis modality soon after the receipt of modality education (nine PD, five HD), two patients remained undecided (Table 1). Six patients were between the ages of 65 and 70 years, seven were between the ages of 71 and 79 years, and three patients were age 80 years or older. Seven patients had started dialysis as inpatients, and three of these individuals eventually decided on HD. Many of the patients had immigrated from the Middle East, the Caribbean or Asia. A family member accompanied the patient during one-third of the interviews.
| Patient . | Age group . | Sex . | Modality choice . | Current modality . | Inpatient start? . |
|---|---|---|---|---|---|
| 1 | 65–70 | Male | HD | HD | No |
| 2 | ≥80 | Female | HD | HD | No |
| 3 | 65–70 | Female | HD | HD | Yes |
| 4 | 65–70 | Female | Unsure | HD | Yes |
| 5 | 71–79 | Female | PD | HD | Yes |
| 6 | 65–70 | Male | PD | Pre-dialysis | No |
| 7 | 71–79 | Male | PD | HD | No |
| 8 | 71–79 | Male | PD | Pre-dialysis | No |
| 9 | 71–79 | Male | PD | Pre-dialysis | No |
| 10 | 65–70 | Male | PD | Pre-dialysis | No |
| 11 | 71–79 | Male | PD | PD | No |
| 12 | 71–79 | Female | HD | HD | Yes |
| 13 | 71–79 | Female | Unsure | HD | Yes |
| 14 | ≥80 | Female | HD | HD | Yes |
| 15 | 65–70 | Female | PD | HD | Yes |
| 16 | 71–79 | Male | PD | Pre-dialysis | No |
| Patient . | Age group . | Sex . | Modality choice . | Current modality . | Inpatient start? . |
|---|---|---|---|---|---|
| 1 | 65–70 | Male | HD | HD | No |
| 2 | ≥80 | Female | HD | HD | No |
| 3 | 65–70 | Female | HD | HD | Yes |
| 4 | 65–70 | Female | Unsure | HD | Yes |
| 5 | 71–79 | Female | PD | HD | Yes |
| 6 | 65–70 | Male | PD | Pre-dialysis | No |
| 7 | 71–79 | Male | PD | HD | No |
| 8 | 71–79 | Male | PD | Pre-dialysis | No |
| 9 | 71–79 | Male | PD | Pre-dialysis | No |
| 10 | 65–70 | Male | PD | Pre-dialysis | No |
| 11 | 71–79 | Male | PD | PD | No |
| 12 | 71–79 | Female | HD | HD | Yes |
| 13 | 71–79 | Female | Unsure | HD | Yes |
| 14 | ≥80 | Female | HD | HD | Yes |
| 15 | 65–70 | Female | PD | HD | Yes |
| 16 | 71–79 | Male | PD | Pre-dialysis | No |
HD, hemodialysis; PD, peritoneal dialysis.
| Patient . | Age group . | Sex . | Modality choice . | Current modality . | Inpatient start? . |
|---|---|---|---|---|---|
| 1 | 65–70 | Male | HD | HD | No |
| 2 | ≥80 | Female | HD | HD | No |
| 3 | 65–70 | Female | HD | HD | Yes |
| 4 | 65–70 | Female | Unsure | HD | Yes |
| 5 | 71–79 | Female | PD | HD | Yes |
| 6 | 65–70 | Male | PD | Pre-dialysis | No |
| 7 | 71–79 | Male | PD | HD | No |
| 8 | 71–79 | Male | PD | Pre-dialysis | No |
| 9 | 71–79 | Male | PD | Pre-dialysis | No |
| 10 | 65–70 | Male | PD | Pre-dialysis | No |
| 11 | 71–79 | Male | PD | PD | No |
| 12 | 71–79 | Female | HD | HD | Yes |
| 13 | 71–79 | Female | Unsure | HD | Yes |
| 14 | ≥80 | Female | HD | HD | Yes |
| 15 | 65–70 | Female | PD | HD | Yes |
| 16 | 71–79 | Male | PD | Pre-dialysis | No |
| Patient . | Age group . | Sex . | Modality choice . | Current modality . | Inpatient start? . |
|---|---|---|---|---|---|
| 1 | 65–70 | Male | HD | HD | No |
| 2 | ≥80 | Female | HD | HD | No |
| 3 | 65–70 | Female | HD | HD | Yes |
| 4 | 65–70 | Female | Unsure | HD | Yes |
| 5 | 71–79 | Female | PD | HD | Yes |
| 6 | 65–70 | Male | PD | Pre-dialysis | No |
| 7 | 71–79 | Male | PD | HD | No |
| 8 | 71–79 | Male | PD | Pre-dialysis | No |
| 9 | 71–79 | Male | PD | Pre-dialysis | No |
| 10 | 65–70 | Male | PD | Pre-dialysis | No |
| 11 | 71–79 | Male | PD | PD | No |
| 12 | 71–79 | Female | HD | HD | Yes |
| 13 | 71–79 | Female | Unsure | HD | Yes |
| 14 | ≥80 | Female | HD | HD | Yes |
| 15 | 65–70 | Female | PD | HD | Yes |
| 16 | 71–79 | Male | PD | Pre-dialysis | No |
HD, hemodialysis; PD, peritoneal dialysis.
Choice of dialysis modality
Overall, patients did not sense bias in the modality education provided to them:
They give us like a manual about all types of dialysis that we can use and read the advantage and disadvantage of each one… so we came back with all these questions and we were well informed I should say too before making a final choice.
Rather, patients perceived autonomy in choosing their preferred dialysis modality:
I've spoken to different people but in the end, I mean obviously I heard what they have to say and I decided to do this way.
Summary of themes
physical strength and dexterity/sound mind,
external forces/constraints,
values and beliefs.
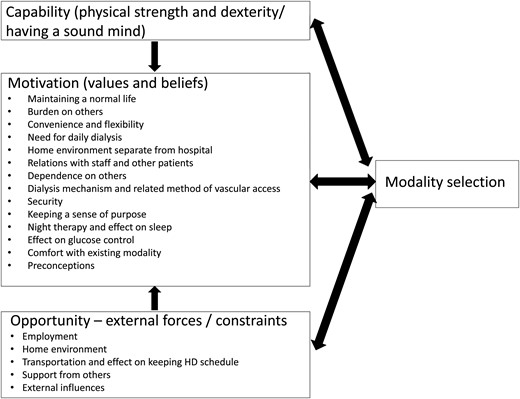
Key factors in dialysis modality selection mapped to the COM-B items of Capability, Opportunity and Motivation.
These key factors can be mapped to the COM-B items of Capability (physical strength and dexterity/sound mind), Opportunity (external forces/constraints) and Motivation (values and beliefs) (Table 2), and analyzed further using the sub-themes in each category.
Quotations from participants to illustrate each theme, mapping to the COM-B system
| Themes . | Quotations from participants . |
|---|---|
| Capability—physical strength and dexterity/having a sound mind | |
| Your strength to lift this stuff to put on the machine the bags of stuff, then you have to cut these boxes up, lots of boxes, every day you have about two boxes to throw out so you have to take a knife. (PD, age 71–79) | |
| You need a good memory to remember the steps of what to do and if the machine fails, you have to be able to switch to the manual bags and things like that. (PD, age 71–79) | |
| I realize my hand is not firm like years ago… when you do manual things with your hands.. I can't do it. (Unsure, age 65–70) | |
| Opportunity—external forces/constraints | |
| Employment | They said that PD would take place all night so that will give him the chance while he's resting he doesn't feel he need to break his day to come here to the hospital all day because he still works. (PD, age 71–79) |
| I am an accountant…I have clients… From home from office. (HD, age 65–70) | |
| Home environment | It's a lot of boxes to store in your, luckily I have a two bedrooms, so I have some space, but somebody with a one bedroom would have a difficult time. (PD, age 71–79) |
| You could trip easily with all this wiring and everything and spacing of our house is not big, so there are times to trip all the time. It's not a convenient place for what somebody needs, especially with the narrow hallways. (HD, age 71–79) | |
| Transportation and effect on keeping HD schedule | I live far from the hospital, so it be you know, with the winter especially, the snow or something like that, I can't keep it a time you know… you have to keep the time exactly for the hospital, so if the weather is bad or something happen and I can't keep it the time. (PD, age 71–79) |
| Wheeltrans is a transportation system that they set up that they pick you up at your home and bring you here and its $2.00 only. They are very reliable and really good. They call you the night before and tell you the time they are going to pick you up and they take me home from the hospital too. (HD, age ≥80) | |
| I'm always late, suppose I'm 2 hours late because I'm always late, right? … and I come what am I going to do you know…now they'll be upset, you know and it's a disadvantage because I'll get sick. (PD, age 65–70) | |
| Support from others | They'll bring the machine at home, they'll bring the supplies at home and there is a 24 hour number in case you want help you call them And on top of that, they will send a nurse to your house to set up the machine 3–4 times a week. (PD, age 65–70) |
| I could have the nurse for the rest of my life, or if I'm independent, I can have them until I tell myself I can do it on my own, and even though I am doing it on my own, there are mistakes to be made and they are only a stone throw away (PD, age 65–70) | |
| I'm a backup definitely… I'm always going to be there for (spouse) definitely for support and everything and I will be learning how to do the dialysis with (spouse). I've already learned a lot with changing the dressing too for the catheter because sometimes it gets overwhelming for (spouse) to do all that on (spouse) own, so I think we are going to carry on with trying to do the PD as well. (Spouse of patient who had selected PD, age 71–79) | |
| External influences | It's just a fact that the PD, my friend has been on it for so many years, so that might have been encouragement. (PD, age 71–79) |
| I went to my doctor, my general doctor who is a family doctor and I asked her about the two and she suggested that because of my age, it would be safer if I came to the hospital, rather than do it at home. She said to do to it at home, your home is constantly a hospital. (HD, age ≥80) | |
| Motivation—values and beliefs | |
| Maintaining a normal life | … So doing it at night time, hopefully when he gets up in the morning he'll start his day as per normal so that's not going to affect his daily routine. (PD, age 71–79) |
| The most important effect is to keep your life and to see which one is the best for maintaining your normal life or much close to normal situation. (PD, age 71–79) | |
| Burden on others | My wife has to drop me for hemo, I don't drive. I stopped driving some years now and the time it takes her to come and the time doing the hemo, it's tedious. (PD, age 71–79) |
| I live with a (spouse) who is 74 years old and it will be too much for (spouse) to take care of me. You know … in the night … if I am on the peritoneal. (Unsure, age 65–70) | |
| I live with my daughter and she has 3 kids, one is married now so it's only the two, and to me, it's hard for the family to have somebody like you who needs help and everything so I think I like coming over. (HD, age 71–79) | |
| Convenience and flexibility | You do it at your convenience. The supplies are brought to you. You have a nurse come if you want for the rest of your life… you have support 24 h a day and what else could you ask for. (PD, age 65–70) |
| To do it at home at night time would be convenient and it would give me free day to do whatever I like to do. In a hospital it wastes my day. I have to come for few hours and you know it ruins my day. That's the main thing (PD, age 71–79) | |
| I guess you have to come a certain time… whereas with the peritoneal dialysis, I have a choice. I could do it 3 times a day for 3 h, or I can do it 9 h at night. (PD, age 65–70) | |
| Need for daily dialysis | But later on, I thought, the peritoneal is an everyday thing… so I thought that for a while, to come to the hospital… to come for the hemo… you come and then you know for sure you are done… that four hours … you are done. And also, I have two days on my own without any dialysis… I can go anywhere and I know for sure that two days are for me. I like to enjoy that. Time with my family… very important. (Unsure, age 65–70) |
| Home environment separate from hospital | To do it at home… your home is constantly a hospital. You are constantly never let free of doing the dialysis; whereas when you come to the hospital you have a few days, and when you go home, you can enjoy your home. (HD, age ≥80) |
| Relations with staff and other patients | Everybody here has been kind and friendly and told me how long they've been on dialysis, talk to the people around me, and I am getting to feel concerned for them…. socialization at the same time. (HD, age ≥80) |
| Whoever's on duty you speak with them, but after the month of doing it, you start to feel you're missing some of them because you used to go in for training and you get to know them and they speak to you and you start to get a bond. (PD, age 71–79) | |
| Dependence on others | I felt I was still capable of doing it myself. There was less dependence on other people. (PD, age 71–79) |
| My spouse changes the bandages at home. Spouse was trained by them how to do it and everything, spouse does that but spouse does all the dressing and covering with plastic when I have to go in the shower. (PD, age 71–79) | |
| And also my pressure is checked and monitored and also the main injections that I receive, the iron and then Epo injection are also given through the machine, so you don't need to do that. These things little mental satisfaction for me. (Unsure, age 65–70) | |
| Being independent as opposed to being dependent, she is in some respects, not an easy person to help because she kind of wants to be able to do it herself and manage it herself… and that PD offers that to her in a way that the others didn't. (Spouse of patient who had selected PD, age 65–70) | |
| Dialysis mechanism and related method of vascular access | They said that it may not work in there, my blood vessel was too small or whatever it was, they said they may have to go up here… might have been a secondary factor but I mean they check it and they said that may not be put it in here… then the other started to talk about the other parts and I decided to go with this (peritoneal dialysis). (PD, age 65–70) |
| I don't like the idea of the blood… the blood coming out and going back in (laughs). Just a little fear of the blood. Peritoneal dialysis… there's not to see, because you know I have a tube that drains straight into the toilet so there's no blood… to me, it looks like a cleaner way of going. (PD, age 71–79) | |
| To me anything that is sticking to my body that is in my body is very uncomfortable because I am always having a problem with diabetes, you always have a tendency to be always scratching and with this one (PD catheter) here. (HD, age 71–79) | |
| He (friend who was on PD) was not comfortable with water in the belly. He's not comfortable with it. So I said to him, I said I would think myself to, I got to think of myself having a belly full of water as well, and then we talk about it later with his daughter and she said that yeah, most of the time my dad complains of his belly is always full. It took him almost a year to try having the PD. (HD, age 71–79) | |
| Security | So I was afraid of being alone and trying it all night what would happen if something went wrong during the night and I am sleeping… they said somebody would come in and help you, or help make sure you are set up correctly, and then, if you are in trouble, you just call somebody. I was afraid if I can't get through on the phone, or if I couldn't get the support I needed, I would be in big trouble, so I didn't trust myself… Really, fear… fear… more than anything is fear… in case something goes wrong and no one is there to help me. Because nobody is in the apartment to help me or know about it. After coming into the (HD) unit like this and talking to everyone I felt more confident that this was the right thing for me… I feel so confident on the nurses who are all so effective and so efficient and so really special. I don't worry about what's happening here. I feel like I am in good hands. (HD, age ≥80) |
| I was told that these nurses will come and train me and then they will be gone… so for me… I don't feel comfortable at my age… I don't feel comfortable with no one there… and if I get an infection (with PD), I heard that it is something very severe but this one (CVC), they change the dressing all the time… no infection will set in because here the nurses take care of you. (Unsure, age 65–70) | |
| I think because of my heart problem… that makes me want to be in the hospital. The doctors are here so that means I would get help right away. (HD, age 71–79) | |
| Keeping a sense of purpose | One reason that I mostly hear from the nurses is that you don't have to travel but you know what… to travel from my home to come here, yes…. I could say that by traveling, it's like I'm being pushed to be kicked out of my bed… a reason to go out. I can also go out to my other personal appointments, but this is something else, like also very important for your health so it kicks me out of bed to go and have this appointment. (Unsure, age 71–79) |
| That means I have a purpose every day. I mean, 3 times a week that I have an appointment to go. (HD, age 71–79) | |
| Night therapy and effect on sleep | The freedom of doing more, getting more done by doing it at home while you are sleeping… that is what attracted me. And if I can do that, get a good sleep, wake up next morning, I have the whole day and part of the night. (PD, age 71–79) |
| I have a CPAP on my face here and I have the machine at home. With the CPAP, I am having a hard time already, so I cannot imagine two machines attached to me. (HD, age 71–79) | |
| I am a person who don't sleep well, it has been like that for me… even before I had kidney problems. I sleep during the day, not in the night… so I thought, once I am hooked on to the peritoneal, I will be losing my sleep. (Unsure, age 65–70) | |
| Effect on glucose control | For peritoneal, the solution that they introduce to the stomach to the belly, is sugar based… so I am diabetic and that sugar based solution can increase my blood sugar level and with hemodialysis, it's the other way… I have got to worry about my sugar… here (at HD), that fear is gone. My diabetic condition, which I had for 15 years, is gone. (Unsure, age 65–70) |
| Comfort with existing modality | This, I am comfortable to do now. I didn't want to change my mind again to go to the other kind. I am now comfortable. (Initially unsure, then selected HD after patient had been started on HD as an inpatient, age ≥80) |
| Preconceptions | The PD infection… you have to be careful about that. I don't think the HD is a problem that much with it. I don't know. (PD, age 71–79) |
| To connect a vein to an artery it's against their nature. I mean you connect an oxygenated body of blood with one that should be clear, and in this case you bring toxins to the brain and that's not a good idea. (PD, age 71–79) | |
| Themes . | Quotations from participants . |
|---|---|
| Capability—physical strength and dexterity/having a sound mind | |
| Your strength to lift this stuff to put on the machine the bags of stuff, then you have to cut these boxes up, lots of boxes, every day you have about two boxes to throw out so you have to take a knife. (PD, age 71–79) | |
| You need a good memory to remember the steps of what to do and if the machine fails, you have to be able to switch to the manual bags and things like that. (PD, age 71–79) | |
| I realize my hand is not firm like years ago… when you do manual things with your hands.. I can't do it. (Unsure, age 65–70) | |
| Opportunity—external forces/constraints | |
| Employment | They said that PD would take place all night so that will give him the chance while he's resting he doesn't feel he need to break his day to come here to the hospital all day because he still works. (PD, age 71–79) |
| I am an accountant…I have clients… From home from office. (HD, age 65–70) | |
| Home environment | It's a lot of boxes to store in your, luckily I have a two bedrooms, so I have some space, but somebody with a one bedroom would have a difficult time. (PD, age 71–79) |
| You could trip easily with all this wiring and everything and spacing of our house is not big, so there are times to trip all the time. It's not a convenient place for what somebody needs, especially with the narrow hallways. (HD, age 71–79) | |
| Transportation and effect on keeping HD schedule | I live far from the hospital, so it be you know, with the winter especially, the snow or something like that, I can't keep it a time you know… you have to keep the time exactly for the hospital, so if the weather is bad or something happen and I can't keep it the time. (PD, age 71–79) |
| Wheeltrans is a transportation system that they set up that they pick you up at your home and bring you here and its $2.00 only. They are very reliable and really good. They call you the night before and tell you the time they are going to pick you up and they take me home from the hospital too. (HD, age ≥80) | |
| I'm always late, suppose I'm 2 hours late because I'm always late, right? … and I come what am I going to do you know…now they'll be upset, you know and it's a disadvantage because I'll get sick. (PD, age 65–70) | |
| Support from others | They'll bring the machine at home, they'll bring the supplies at home and there is a 24 hour number in case you want help you call them And on top of that, they will send a nurse to your house to set up the machine 3–4 times a week. (PD, age 65–70) |
| I could have the nurse for the rest of my life, or if I'm independent, I can have them until I tell myself I can do it on my own, and even though I am doing it on my own, there are mistakes to be made and they are only a stone throw away (PD, age 65–70) | |
| I'm a backup definitely… I'm always going to be there for (spouse) definitely for support and everything and I will be learning how to do the dialysis with (spouse). I've already learned a lot with changing the dressing too for the catheter because sometimes it gets overwhelming for (spouse) to do all that on (spouse) own, so I think we are going to carry on with trying to do the PD as well. (Spouse of patient who had selected PD, age 71–79) | |
| External influences | It's just a fact that the PD, my friend has been on it for so many years, so that might have been encouragement. (PD, age 71–79) |
| I went to my doctor, my general doctor who is a family doctor and I asked her about the two and she suggested that because of my age, it would be safer if I came to the hospital, rather than do it at home. She said to do to it at home, your home is constantly a hospital. (HD, age ≥80) | |
| Motivation—values and beliefs | |
| Maintaining a normal life | … So doing it at night time, hopefully when he gets up in the morning he'll start his day as per normal so that's not going to affect his daily routine. (PD, age 71–79) |
| The most important effect is to keep your life and to see which one is the best for maintaining your normal life or much close to normal situation. (PD, age 71–79) | |
| Burden on others | My wife has to drop me for hemo, I don't drive. I stopped driving some years now and the time it takes her to come and the time doing the hemo, it's tedious. (PD, age 71–79) |
| I live with a (spouse) who is 74 years old and it will be too much for (spouse) to take care of me. You know … in the night … if I am on the peritoneal. (Unsure, age 65–70) | |
| I live with my daughter and she has 3 kids, one is married now so it's only the two, and to me, it's hard for the family to have somebody like you who needs help and everything so I think I like coming over. (HD, age 71–79) | |
| Convenience and flexibility | You do it at your convenience. The supplies are brought to you. You have a nurse come if you want for the rest of your life… you have support 24 h a day and what else could you ask for. (PD, age 65–70) |
| To do it at home at night time would be convenient and it would give me free day to do whatever I like to do. In a hospital it wastes my day. I have to come for few hours and you know it ruins my day. That's the main thing (PD, age 71–79) | |
| I guess you have to come a certain time… whereas with the peritoneal dialysis, I have a choice. I could do it 3 times a day for 3 h, or I can do it 9 h at night. (PD, age 65–70) | |
| Need for daily dialysis | But later on, I thought, the peritoneal is an everyday thing… so I thought that for a while, to come to the hospital… to come for the hemo… you come and then you know for sure you are done… that four hours … you are done. And also, I have two days on my own without any dialysis… I can go anywhere and I know for sure that two days are for me. I like to enjoy that. Time with my family… very important. (Unsure, age 65–70) |
| Home environment separate from hospital | To do it at home… your home is constantly a hospital. You are constantly never let free of doing the dialysis; whereas when you come to the hospital you have a few days, and when you go home, you can enjoy your home. (HD, age ≥80) |
| Relations with staff and other patients | Everybody here has been kind and friendly and told me how long they've been on dialysis, talk to the people around me, and I am getting to feel concerned for them…. socialization at the same time. (HD, age ≥80) |
| Whoever's on duty you speak with them, but after the month of doing it, you start to feel you're missing some of them because you used to go in for training and you get to know them and they speak to you and you start to get a bond. (PD, age 71–79) | |
| Dependence on others | I felt I was still capable of doing it myself. There was less dependence on other people. (PD, age 71–79) |
| My spouse changes the bandages at home. Spouse was trained by them how to do it and everything, spouse does that but spouse does all the dressing and covering with plastic when I have to go in the shower. (PD, age 71–79) | |
| And also my pressure is checked and monitored and also the main injections that I receive, the iron and then Epo injection are also given through the machine, so you don't need to do that. These things little mental satisfaction for me. (Unsure, age 65–70) | |
| Being independent as opposed to being dependent, she is in some respects, not an easy person to help because she kind of wants to be able to do it herself and manage it herself… and that PD offers that to her in a way that the others didn't. (Spouse of patient who had selected PD, age 65–70) | |
| Dialysis mechanism and related method of vascular access | They said that it may not work in there, my blood vessel was too small or whatever it was, they said they may have to go up here… might have been a secondary factor but I mean they check it and they said that may not be put it in here… then the other started to talk about the other parts and I decided to go with this (peritoneal dialysis). (PD, age 65–70) |
| I don't like the idea of the blood… the blood coming out and going back in (laughs). Just a little fear of the blood. Peritoneal dialysis… there's not to see, because you know I have a tube that drains straight into the toilet so there's no blood… to me, it looks like a cleaner way of going. (PD, age 71–79) | |
| To me anything that is sticking to my body that is in my body is very uncomfortable because I am always having a problem with diabetes, you always have a tendency to be always scratching and with this one (PD catheter) here. (HD, age 71–79) | |
| He (friend who was on PD) was not comfortable with water in the belly. He's not comfortable with it. So I said to him, I said I would think myself to, I got to think of myself having a belly full of water as well, and then we talk about it later with his daughter and she said that yeah, most of the time my dad complains of his belly is always full. It took him almost a year to try having the PD. (HD, age 71–79) | |
| Security | So I was afraid of being alone and trying it all night what would happen if something went wrong during the night and I am sleeping… they said somebody would come in and help you, or help make sure you are set up correctly, and then, if you are in trouble, you just call somebody. I was afraid if I can't get through on the phone, or if I couldn't get the support I needed, I would be in big trouble, so I didn't trust myself… Really, fear… fear… more than anything is fear… in case something goes wrong and no one is there to help me. Because nobody is in the apartment to help me or know about it. After coming into the (HD) unit like this and talking to everyone I felt more confident that this was the right thing for me… I feel so confident on the nurses who are all so effective and so efficient and so really special. I don't worry about what's happening here. I feel like I am in good hands. (HD, age ≥80) |
| I was told that these nurses will come and train me and then they will be gone… so for me… I don't feel comfortable at my age… I don't feel comfortable with no one there… and if I get an infection (with PD), I heard that it is something very severe but this one (CVC), they change the dressing all the time… no infection will set in because here the nurses take care of you. (Unsure, age 65–70) | |
| I think because of my heart problem… that makes me want to be in the hospital. The doctors are here so that means I would get help right away. (HD, age 71–79) | |
| Keeping a sense of purpose | One reason that I mostly hear from the nurses is that you don't have to travel but you know what… to travel from my home to come here, yes…. I could say that by traveling, it's like I'm being pushed to be kicked out of my bed… a reason to go out. I can also go out to my other personal appointments, but this is something else, like also very important for your health so it kicks me out of bed to go and have this appointment. (Unsure, age 71–79) |
| That means I have a purpose every day. I mean, 3 times a week that I have an appointment to go. (HD, age 71–79) | |
| Night therapy and effect on sleep | The freedom of doing more, getting more done by doing it at home while you are sleeping… that is what attracted me. And if I can do that, get a good sleep, wake up next morning, I have the whole day and part of the night. (PD, age 71–79) |
| I have a CPAP on my face here and I have the machine at home. With the CPAP, I am having a hard time already, so I cannot imagine two machines attached to me. (HD, age 71–79) | |
| I am a person who don't sleep well, it has been like that for me… even before I had kidney problems. I sleep during the day, not in the night… so I thought, once I am hooked on to the peritoneal, I will be losing my sleep. (Unsure, age 65–70) | |
| Effect on glucose control | For peritoneal, the solution that they introduce to the stomach to the belly, is sugar based… so I am diabetic and that sugar based solution can increase my blood sugar level and with hemodialysis, it's the other way… I have got to worry about my sugar… here (at HD), that fear is gone. My diabetic condition, which I had for 15 years, is gone. (Unsure, age 65–70) |
| Comfort with existing modality | This, I am comfortable to do now. I didn't want to change my mind again to go to the other kind. I am now comfortable. (Initially unsure, then selected HD after patient had been started on HD as an inpatient, age ≥80) |
| Preconceptions | The PD infection… you have to be careful about that. I don't think the HD is a problem that much with it. I don't know. (PD, age 71–79) |
| To connect a vein to an artery it's against their nature. I mean you connect an oxygenated body of blood with one that should be clear, and in this case you bring toxins to the brain and that's not a good idea. (PD, age 71–79) | |
Quotations from participants to illustrate each theme, mapping to the COM-B system
| Themes . | Quotations from participants . |
|---|---|
| Capability—physical strength and dexterity/having a sound mind | |
| Your strength to lift this stuff to put on the machine the bags of stuff, then you have to cut these boxes up, lots of boxes, every day you have about two boxes to throw out so you have to take a knife. (PD, age 71–79) | |
| You need a good memory to remember the steps of what to do and if the machine fails, you have to be able to switch to the manual bags and things like that. (PD, age 71–79) | |
| I realize my hand is not firm like years ago… when you do manual things with your hands.. I can't do it. (Unsure, age 65–70) | |
| Opportunity—external forces/constraints | |
| Employment | They said that PD would take place all night so that will give him the chance while he's resting he doesn't feel he need to break his day to come here to the hospital all day because he still works. (PD, age 71–79) |
| I am an accountant…I have clients… From home from office. (HD, age 65–70) | |
| Home environment | It's a lot of boxes to store in your, luckily I have a two bedrooms, so I have some space, but somebody with a one bedroom would have a difficult time. (PD, age 71–79) |
| You could trip easily with all this wiring and everything and spacing of our house is not big, so there are times to trip all the time. It's not a convenient place for what somebody needs, especially with the narrow hallways. (HD, age 71–79) | |
| Transportation and effect on keeping HD schedule | I live far from the hospital, so it be you know, with the winter especially, the snow or something like that, I can't keep it a time you know… you have to keep the time exactly for the hospital, so if the weather is bad or something happen and I can't keep it the time. (PD, age 71–79) |
| Wheeltrans is a transportation system that they set up that they pick you up at your home and bring you here and its $2.00 only. They are very reliable and really good. They call you the night before and tell you the time they are going to pick you up and they take me home from the hospital too. (HD, age ≥80) | |
| I'm always late, suppose I'm 2 hours late because I'm always late, right? … and I come what am I going to do you know…now they'll be upset, you know and it's a disadvantage because I'll get sick. (PD, age 65–70) | |
| Support from others | They'll bring the machine at home, they'll bring the supplies at home and there is a 24 hour number in case you want help you call them And on top of that, they will send a nurse to your house to set up the machine 3–4 times a week. (PD, age 65–70) |
| I could have the nurse for the rest of my life, or if I'm independent, I can have them until I tell myself I can do it on my own, and even though I am doing it on my own, there are mistakes to be made and they are only a stone throw away (PD, age 65–70) | |
| I'm a backup definitely… I'm always going to be there for (spouse) definitely for support and everything and I will be learning how to do the dialysis with (spouse). I've already learned a lot with changing the dressing too for the catheter because sometimes it gets overwhelming for (spouse) to do all that on (spouse) own, so I think we are going to carry on with trying to do the PD as well. (Spouse of patient who had selected PD, age 71–79) | |
| External influences | It's just a fact that the PD, my friend has been on it for so many years, so that might have been encouragement. (PD, age 71–79) |
| I went to my doctor, my general doctor who is a family doctor and I asked her about the two and she suggested that because of my age, it would be safer if I came to the hospital, rather than do it at home. She said to do to it at home, your home is constantly a hospital. (HD, age ≥80) | |
| Motivation—values and beliefs | |
| Maintaining a normal life | … So doing it at night time, hopefully when he gets up in the morning he'll start his day as per normal so that's not going to affect his daily routine. (PD, age 71–79) |
| The most important effect is to keep your life and to see which one is the best for maintaining your normal life or much close to normal situation. (PD, age 71–79) | |
| Burden on others | My wife has to drop me for hemo, I don't drive. I stopped driving some years now and the time it takes her to come and the time doing the hemo, it's tedious. (PD, age 71–79) |
| I live with a (spouse) who is 74 years old and it will be too much for (spouse) to take care of me. You know … in the night … if I am on the peritoneal. (Unsure, age 65–70) | |
| I live with my daughter and she has 3 kids, one is married now so it's only the two, and to me, it's hard for the family to have somebody like you who needs help and everything so I think I like coming over. (HD, age 71–79) | |
| Convenience and flexibility | You do it at your convenience. The supplies are brought to you. You have a nurse come if you want for the rest of your life… you have support 24 h a day and what else could you ask for. (PD, age 65–70) |
| To do it at home at night time would be convenient and it would give me free day to do whatever I like to do. In a hospital it wastes my day. I have to come for few hours and you know it ruins my day. That's the main thing (PD, age 71–79) | |
| I guess you have to come a certain time… whereas with the peritoneal dialysis, I have a choice. I could do it 3 times a day for 3 h, or I can do it 9 h at night. (PD, age 65–70) | |
| Need for daily dialysis | But later on, I thought, the peritoneal is an everyday thing… so I thought that for a while, to come to the hospital… to come for the hemo… you come and then you know for sure you are done… that four hours … you are done. And also, I have two days on my own without any dialysis… I can go anywhere and I know for sure that two days are for me. I like to enjoy that. Time with my family… very important. (Unsure, age 65–70) |
| Home environment separate from hospital | To do it at home… your home is constantly a hospital. You are constantly never let free of doing the dialysis; whereas when you come to the hospital you have a few days, and when you go home, you can enjoy your home. (HD, age ≥80) |
| Relations with staff and other patients | Everybody here has been kind and friendly and told me how long they've been on dialysis, talk to the people around me, and I am getting to feel concerned for them…. socialization at the same time. (HD, age ≥80) |
| Whoever's on duty you speak with them, but after the month of doing it, you start to feel you're missing some of them because you used to go in for training and you get to know them and they speak to you and you start to get a bond. (PD, age 71–79) | |
| Dependence on others | I felt I was still capable of doing it myself. There was less dependence on other people. (PD, age 71–79) |
| My spouse changes the bandages at home. Spouse was trained by them how to do it and everything, spouse does that but spouse does all the dressing and covering with plastic when I have to go in the shower. (PD, age 71–79) | |
| And also my pressure is checked and monitored and also the main injections that I receive, the iron and then Epo injection are also given through the machine, so you don't need to do that. These things little mental satisfaction for me. (Unsure, age 65–70) | |
| Being independent as opposed to being dependent, she is in some respects, not an easy person to help because she kind of wants to be able to do it herself and manage it herself… and that PD offers that to her in a way that the others didn't. (Spouse of patient who had selected PD, age 65–70) | |
| Dialysis mechanism and related method of vascular access | They said that it may not work in there, my blood vessel was too small or whatever it was, they said they may have to go up here… might have been a secondary factor but I mean they check it and they said that may not be put it in here… then the other started to talk about the other parts and I decided to go with this (peritoneal dialysis). (PD, age 65–70) |
| I don't like the idea of the blood… the blood coming out and going back in (laughs). Just a little fear of the blood. Peritoneal dialysis… there's not to see, because you know I have a tube that drains straight into the toilet so there's no blood… to me, it looks like a cleaner way of going. (PD, age 71–79) | |
| To me anything that is sticking to my body that is in my body is very uncomfortable because I am always having a problem with diabetes, you always have a tendency to be always scratching and with this one (PD catheter) here. (HD, age 71–79) | |
| He (friend who was on PD) was not comfortable with water in the belly. He's not comfortable with it. So I said to him, I said I would think myself to, I got to think of myself having a belly full of water as well, and then we talk about it later with his daughter and she said that yeah, most of the time my dad complains of his belly is always full. It took him almost a year to try having the PD. (HD, age 71–79) | |
| Security | So I was afraid of being alone and trying it all night what would happen if something went wrong during the night and I am sleeping… they said somebody would come in and help you, or help make sure you are set up correctly, and then, if you are in trouble, you just call somebody. I was afraid if I can't get through on the phone, or if I couldn't get the support I needed, I would be in big trouble, so I didn't trust myself… Really, fear… fear… more than anything is fear… in case something goes wrong and no one is there to help me. Because nobody is in the apartment to help me or know about it. After coming into the (HD) unit like this and talking to everyone I felt more confident that this was the right thing for me… I feel so confident on the nurses who are all so effective and so efficient and so really special. I don't worry about what's happening here. I feel like I am in good hands. (HD, age ≥80) |
| I was told that these nurses will come and train me and then they will be gone… so for me… I don't feel comfortable at my age… I don't feel comfortable with no one there… and if I get an infection (with PD), I heard that it is something very severe but this one (CVC), they change the dressing all the time… no infection will set in because here the nurses take care of you. (Unsure, age 65–70) | |
| I think because of my heart problem… that makes me want to be in the hospital. The doctors are here so that means I would get help right away. (HD, age 71–79) | |
| Keeping a sense of purpose | One reason that I mostly hear from the nurses is that you don't have to travel but you know what… to travel from my home to come here, yes…. I could say that by traveling, it's like I'm being pushed to be kicked out of my bed… a reason to go out. I can also go out to my other personal appointments, but this is something else, like also very important for your health so it kicks me out of bed to go and have this appointment. (Unsure, age 71–79) |
| That means I have a purpose every day. I mean, 3 times a week that I have an appointment to go. (HD, age 71–79) | |
| Night therapy and effect on sleep | The freedom of doing more, getting more done by doing it at home while you are sleeping… that is what attracted me. And if I can do that, get a good sleep, wake up next morning, I have the whole day and part of the night. (PD, age 71–79) |
| I have a CPAP on my face here and I have the machine at home. With the CPAP, I am having a hard time already, so I cannot imagine two machines attached to me. (HD, age 71–79) | |
| I am a person who don't sleep well, it has been like that for me… even before I had kidney problems. I sleep during the day, not in the night… so I thought, once I am hooked on to the peritoneal, I will be losing my sleep. (Unsure, age 65–70) | |
| Effect on glucose control | For peritoneal, the solution that they introduce to the stomach to the belly, is sugar based… so I am diabetic and that sugar based solution can increase my blood sugar level and with hemodialysis, it's the other way… I have got to worry about my sugar… here (at HD), that fear is gone. My diabetic condition, which I had for 15 years, is gone. (Unsure, age 65–70) |
| Comfort with existing modality | This, I am comfortable to do now. I didn't want to change my mind again to go to the other kind. I am now comfortable. (Initially unsure, then selected HD after patient had been started on HD as an inpatient, age ≥80) |
| Preconceptions | The PD infection… you have to be careful about that. I don't think the HD is a problem that much with it. I don't know. (PD, age 71–79) |
| To connect a vein to an artery it's against their nature. I mean you connect an oxygenated body of blood with one that should be clear, and in this case you bring toxins to the brain and that's not a good idea. (PD, age 71–79) | |
| Themes . | Quotations from participants . |
|---|---|
| Capability—physical strength and dexterity/having a sound mind | |
| Your strength to lift this stuff to put on the machine the bags of stuff, then you have to cut these boxes up, lots of boxes, every day you have about two boxes to throw out so you have to take a knife. (PD, age 71–79) | |
| You need a good memory to remember the steps of what to do and if the machine fails, you have to be able to switch to the manual bags and things like that. (PD, age 71–79) | |
| I realize my hand is not firm like years ago… when you do manual things with your hands.. I can't do it. (Unsure, age 65–70) | |
| Opportunity—external forces/constraints | |
| Employment | They said that PD would take place all night so that will give him the chance while he's resting he doesn't feel he need to break his day to come here to the hospital all day because he still works. (PD, age 71–79) |
| I am an accountant…I have clients… From home from office. (HD, age 65–70) | |
| Home environment | It's a lot of boxes to store in your, luckily I have a two bedrooms, so I have some space, but somebody with a one bedroom would have a difficult time. (PD, age 71–79) |
| You could trip easily with all this wiring and everything and spacing of our house is not big, so there are times to trip all the time. It's not a convenient place for what somebody needs, especially with the narrow hallways. (HD, age 71–79) | |
| Transportation and effect on keeping HD schedule | I live far from the hospital, so it be you know, with the winter especially, the snow or something like that, I can't keep it a time you know… you have to keep the time exactly for the hospital, so if the weather is bad or something happen and I can't keep it the time. (PD, age 71–79) |
| Wheeltrans is a transportation system that they set up that they pick you up at your home and bring you here and its $2.00 only. They are very reliable and really good. They call you the night before and tell you the time they are going to pick you up and they take me home from the hospital too. (HD, age ≥80) | |
| I'm always late, suppose I'm 2 hours late because I'm always late, right? … and I come what am I going to do you know…now they'll be upset, you know and it's a disadvantage because I'll get sick. (PD, age 65–70) | |
| Support from others | They'll bring the machine at home, they'll bring the supplies at home and there is a 24 hour number in case you want help you call them And on top of that, they will send a nurse to your house to set up the machine 3–4 times a week. (PD, age 65–70) |
| I could have the nurse for the rest of my life, or if I'm independent, I can have them until I tell myself I can do it on my own, and even though I am doing it on my own, there are mistakes to be made and they are only a stone throw away (PD, age 65–70) | |
| I'm a backup definitely… I'm always going to be there for (spouse) definitely for support and everything and I will be learning how to do the dialysis with (spouse). I've already learned a lot with changing the dressing too for the catheter because sometimes it gets overwhelming for (spouse) to do all that on (spouse) own, so I think we are going to carry on with trying to do the PD as well. (Spouse of patient who had selected PD, age 71–79) | |
| External influences | It's just a fact that the PD, my friend has been on it for so many years, so that might have been encouragement. (PD, age 71–79) |
| I went to my doctor, my general doctor who is a family doctor and I asked her about the two and she suggested that because of my age, it would be safer if I came to the hospital, rather than do it at home. She said to do to it at home, your home is constantly a hospital. (HD, age ≥80) | |
| Motivation—values and beliefs | |
| Maintaining a normal life | … So doing it at night time, hopefully when he gets up in the morning he'll start his day as per normal so that's not going to affect his daily routine. (PD, age 71–79) |
| The most important effect is to keep your life and to see which one is the best for maintaining your normal life or much close to normal situation. (PD, age 71–79) | |
| Burden on others | My wife has to drop me for hemo, I don't drive. I stopped driving some years now and the time it takes her to come and the time doing the hemo, it's tedious. (PD, age 71–79) |
| I live with a (spouse) who is 74 years old and it will be too much for (spouse) to take care of me. You know … in the night … if I am on the peritoneal. (Unsure, age 65–70) | |
| I live with my daughter and she has 3 kids, one is married now so it's only the two, and to me, it's hard for the family to have somebody like you who needs help and everything so I think I like coming over. (HD, age 71–79) | |
| Convenience and flexibility | You do it at your convenience. The supplies are brought to you. You have a nurse come if you want for the rest of your life… you have support 24 h a day and what else could you ask for. (PD, age 65–70) |
| To do it at home at night time would be convenient and it would give me free day to do whatever I like to do. In a hospital it wastes my day. I have to come for few hours and you know it ruins my day. That's the main thing (PD, age 71–79) | |
| I guess you have to come a certain time… whereas with the peritoneal dialysis, I have a choice. I could do it 3 times a day for 3 h, or I can do it 9 h at night. (PD, age 65–70) | |
| Need for daily dialysis | But later on, I thought, the peritoneal is an everyday thing… so I thought that for a while, to come to the hospital… to come for the hemo… you come and then you know for sure you are done… that four hours … you are done. And also, I have two days on my own without any dialysis… I can go anywhere and I know for sure that two days are for me. I like to enjoy that. Time with my family… very important. (Unsure, age 65–70) |
| Home environment separate from hospital | To do it at home… your home is constantly a hospital. You are constantly never let free of doing the dialysis; whereas when you come to the hospital you have a few days, and when you go home, you can enjoy your home. (HD, age ≥80) |
| Relations with staff and other patients | Everybody here has been kind and friendly and told me how long they've been on dialysis, talk to the people around me, and I am getting to feel concerned for them…. socialization at the same time. (HD, age ≥80) |
| Whoever's on duty you speak with them, but after the month of doing it, you start to feel you're missing some of them because you used to go in for training and you get to know them and they speak to you and you start to get a bond. (PD, age 71–79) | |
| Dependence on others | I felt I was still capable of doing it myself. There was less dependence on other people. (PD, age 71–79) |
| My spouse changes the bandages at home. Spouse was trained by them how to do it and everything, spouse does that but spouse does all the dressing and covering with plastic when I have to go in the shower. (PD, age 71–79) | |
| And also my pressure is checked and monitored and also the main injections that I receive, the iron and then Epo injection are also given through the machine, so you don't need to do that. These things little mental satisfaction for me. (Unsure, age 65–70) | |
| Being independent as opposed to being dependent, she is in some respects, not an easy person to help because she kind of wants to be able to do it herself and manage it herself… and that PD offers that to her in a way that the others didn't. (Spouse of patient who had selected PD, age 65–70) | |
| Dialysis mechanism and related method of vascular access | They said that it may not work in there, my blood vessel was too small or whatever it was, they said they may have to go up here… might have been a secondary factor but I mean they check it and they said that may not be put it in here… then the other started to talk about the other parts and I decided to go with this (peritoneal dialysis). (PD, age 65–70) |
| I don't like the idea of the blood… the blood coming out and going back in (laughs). Just a little fear of the blood. Peritoneal dialysis… there's not to see, because you know I have a tube that drains straight into the toilet so there's no blood… to me, it looks like a cleaner way of going. (PD, age 71–79) | |
| To me anything that is sticking to my body that is in my body is very uncomfortable because I am always having a problem with diabetes, you always have a tendency to be always scratching and with this one (PD catheter) here. (HD, age 71–79) | |
| He (friend who was on PD) was not comfortable with water in the belly. He's not comfortable with it. So I said to him, I said I would think myself to, I got to think of myself having a belly full of water as well, and then we talk about it later with his daughter and she said that yeah, most of the time my dad complains of his belly is always full. It took him almost a year to try having the PD. (HD, age 71–79) | |
| Security | So I was afraid of being alone and trying it all night what would happen if something went wrong during the night and I am sleeping… they said somebody would come in and help you, or help make sure you are set up correctly, and then, if you are in trouble, you just call somebody. I was afraid if I can't get through on the phone, or if I couldn't get the support I needed, I would be in big trouble, so I didn't trust myself… Really, fear… fear… more than anything is fear… in case something goes wrong and no one is there to help me. Because nobody is in the apartment to help me or know about it. After coming into the (HD) unit like this and talking to everyone I felt more confident that this was the right thing for me… I feel so confident on the nurses who are all so effective and so efficient and so really special. I don't worry about what's happening here. I feel like I am in good hands. (HD, age ≥80) |
| I was told that these nurses will come and train me and then they will be gone… so for me… I don't feel comfortable at my age… I don't feel comfortable with no one there… and if I get an infection (with PD), I heard that it is something very severe but this one (CVC), they change the dressing all the time… no infection will set in because here the nurses take care of you. (Unsure, age 65–70) | |
| I think because of my heart problem… that makes me want to be in the hospital. The doctors are here so that means I would get help right away. (HD, age 71–79) | |
| Keeping a sense of purpose | One reason that I mostly hear from the nurses is that you don't have to travel but you know what… to travel from my home to come here, yes…. I could say that by traveling, it's like I'm being pushed to be kicked out of my bed… a reason to go out. I can also go out to my other personal appointments, but this is something else, like also very important for your health so it kicks me out of bed to go and have this appointment. (Unsure, age 71–79) |
| That means I have a purpose every day. I mean, 3 times a week that I have an appointment to go. (HD, age 71–79) | |
| Night therapy and effect on sleep | The freedom of doing more, getting more done by doing it at home while you are sleeping… that is what attracted me. And if I can do that, get a good sleep, wake up next morning, I have the whole day and part of the night. (PD, age 71–79) |
| I have a CPAP on my face here and I have the machine at home. With the CPAP, I am having a hard time already, so I cannot imagine two machines attached to me. (HD, age 71–79) | |
| I am a person who don't sleep well, it has been like that for me… even before I had kidney problems. I sleep during the day, not in the night… so I thought, once I am hooked on to the peritoneal, I will be losing my sleep. (Unsure, age 65–70) | |
| Effect on glucose control | For peritoneal, the solution that they introduce to the stomach to the belly, is sugar based… so I am diabetic and that sugar based solution can increase my blood sugar level and with hemodialysis, it's the other way… I have got to worry about my sugar… here (at HD), that fear is gone. My diabetic condition, which I had for 15 years, is gone. (Unsure, age 65–70) |
| Comfort with existing modality | This, I am comfortable to do now. I didn't want to change my mind again to go to the other kind. I am now comfortable. (Initially unsure, then selected HD after patient had been started on HD as an inpatient, age ≥80) |
| Preconceptions | The PD infection… you have to be careful about that. I don't think the HD is a problem that much with it. I don't know. (PD, age 71–79) |
| To connect a vein to an artery it's against their nature. I mean you connect an oxygenated body of blood with one that should be clear, and in this case you bring toxins to the brain and that's not a good idea. (PD, age 71–79) | |
Capability—physical strength and dexterity/having a sound mind
Some patients acknowledged the need to have adequate physical capacity, manual dexterity and a sound mind to self-administer PD at home. This was particularly relevant when patients were uremic and in need of imminent dialysis. Reference with respect to physical strength was made both regarding setting up the PD equipment and the disposal of supplies:
Your strength to lift this stuff to put on the machine… the bags of stuff, then you have to cut these boxes up, lots of boxes, every day you have about two boxes to throw out so you have to take a knife.
Opportunity—external forces/constraints
The theme external forces/constraints described all the factors extrinsic to the individual that influenced patients' modality selection.
Employment. A few patients continued to work and their choice of dialysis modality reflected the need to maintain regular daytime employment:
They said that PD would take place all night so that will give him the chance while he's resting… he doesn't feel he need to break his day to come here to the hospital all day because he still works.
Home environment. The home environment with respect to adequate physical space to accommodate the PD machine, and more importantly, the supplies, was pertinent to PD selection:
If we would have met somebody on it (PD), that it would have made a big difference and saw what it meant in the house, and how much time and space you need.
Transportation and effect on keeping HD schedule. For some patients, the requirement to arrive at HD on time posed a potential concern due to the distance between their residence and the HD facility and the possibility of inclement weather, while others had faith in keeping their scheduled HD spot with the pre-arranged special transportation service:
I live far from the hospital so, you know, with the winter especially, the snow or something like that, I can't keep a time you know, you have to keep the time exactly for the hospital.
Support from others. For some patients who had selected PD, the availability of caregivers to help administer PD in their own homes and the availability of around-the-clock support by telephone provided reassurance for those living alone. For others who had a co-habitant, the other person played a significant role in terms of being a ‘back-up’ support:
I could have the nurse (from home care) for the rest of my life, or if I'm independent, I can have them until I tell myself I can do it on my own, and even though I am doing it on my own, there are mistakes to be made and they are only a stone throw away.
External influences. Patients were also influenced to various extents by their family and friends, and interactions with health care professionals, regardless of their reason(s) for selecting a particular dialysis modality:
It's just a fact that the PD, my friend has been on it for so many years, so that might have been encouragement.
Motivation—values and beliefs
The theme values and beliefs referred to patients' intrinsic thought processes that consciously and subconsciously modified their modality decision-making. For most patients, their modality selection evolved mostly around sub-themes in this area.
Maintaining a normal life. The ability to continue to live a life that resembled their regular life, prior to the need for maintenance dialysis, was important to some patients, especially with consideration of the possibility of dialyzing at night:
The most important effect is to keep your life and to see which one is the best for maintaining your normal life or much close to normal situation.
Burden on others. Patients expressed concern about the effect of their treatment on their family, both in terms of transporting the patient to a health facility for in-center HD and helping with self-administering PD at home:
I live with my daughter and she has 3 kids, and to me, it's hard for the family to have somebody like you who needs help and everything, so I think I like coming over.
Convenience and flexibility. The comfort afforded by PD (enabling patients to dialyze in their own homes with the supplies delivered to them) and the ability to select their PD regimen (especially being able to dialyze overnight and have their day schedule open) were very important to some patients:
To do it at home at night time would be convenient and it would give me free day to do whatever I like to do. In a hospital it wastes my day. I have to come for few hours, and you know, it ruins my day. That's the main thing.
Need for daily dialysis. Some patients valued the days off from any HD treatments as opposed to requirement for daily administration of PD. They felt empowered to spend those days however they want:
But later on, I thought, the peritoneal is an everyday thing… so I thought that for a while, to come to the hospital… to come for the hemo… you come and then you know for sure you are done…. and also, I have two days on my own without any dialysis… I can go anywhere and I know for sure that two days are for me. I like to enjoy that. Time with my family … very important.
Home environment separate from hospital. Similar to the theme of daily dialysis, some patients preferred to keep their homes separate from the hospital and to avoid ‘medicalizing’ their homes by choosing HD:
To do it at home… your home is constantly a hospital. You are constantly never let free of doing the dialysis; whereas when you come to the hospital you have a few days, and when you go home you can enjoy your home.
Relations with staff and other patients. Relationship with nurses and other patients was important to some patients. For patients who had selected HD, some of them shared a bond with other patients because they felt they were interacting with people who could relate to their own medical problems. For PD patients, they developed a familiarity with the nursing staff because they interacted with the same staff during their training and there were much fewer PD nurses in comparison to HD nurses.
Everybody here has been kind and friendly and told me how long they've been on dialysis, talk to the people around me, and I am getting to feel concerned for them…. socialization at the same time.
Dependence on others. Some patients did not like being dependent on others when they felt they were still capable of caring for themselves, while others felt reassured that their care was dependent on their family or nursing staff:
I felt I was still capable of doing it myself. There was less dependence on other people.
And also my blood pressure is checked and monitored and also the main injections that I receive, the iron and then Epo injection are also given through the machine, so you don't need to do that. These things are little mental satisfaction for me.
Dialysis mechanism and related method of vascular access. The type of vascular access in relation to the respective dialysis modality was relevant to some patients. Patients took into account the procedures required for access creation (including the potential need for multiple surgeries for non-functional arteriovenous fistulas (AVFs) and potential exposure to blood with HD:
They said that it may not work in there, my blood vessel was too small or whatever it was, and they said that may not be put it in here, then the other started to talk about the other parts and I decided to go with this (peritoneal dialysis).
Security. Performing dialysis independently was a barrier for some patients, especially those who lived alone or with an older spouse. These patients remained apprehensive in spite of the knowledge that help was available (by phone) at all times and assisted PD (whereby a home care nursing staff assists with the connection/disconnection of PD equipment at their homes) could be arranged. Patients also sensed improved safety from supervised dialysis treatment due to their underlying medical comorbidities and the potential of missed infections when dialyzing alone:
Really, fear… fear… more than anything is fear… in case something goes wrong and no one is there to help me… because nobody is in the apartment to help me or know about it…
Keeping a sense of purpose. For some patients, attending HD sessions provided them a reason to leave their house in spite of the time commitment required when coming to dialysis:
That means I have a purpose every day. I mean, 3 times a week that I have an appointment to go.
Night therapy and effect on sleep. The option to perform PD at night during sleep was important to some patients given the resultant freedom afforded them during the day. However, this also posed potential concerns for other patients because of the potential effects on their sleep, especially if they were on other medical therapies at night, such as continuous positive airway pressure (CPAP) for treatment of obstructive sleep apnea. Some patients were also concerned about being connected to the PD machine at night if they had to use the bathroom.
The freedom of doing more, getting more done by doing it at home while you are sleeping. That is what attracted me. And if I can do that, get a good sleep, wake up next morning, I have the whole day and part of the night.
Effect on glucose control. For some diabetics, elevated blood sugar from the receipt of PD solution was concerning:
For peritoneal, the solution that they introduce to the belly, is sugar based… so I am diabetic and that sugar based solution can increase my blood sugar level and with hemodialysis, it's the other way.
Comfort with existing modality. Some patients found comfort in staying with their current dialysis modality:
This, I am comfortable to now. I didn't want to change my mind again to go to the other kind. I am now comfortable.
Preconceptions. Some patients had certain preconceptions and beliefs about health and illness that influenced their decision to select a particular dialysis modality. Specifically, there was a concern that infections associated with PD are more serious and another patient was troubled by the creation of an AVF for HD because of his belief that the artery and venous blood supply should remain separate.
The PD infection… you have to be careful about that. I don't think the HD is a problem that much with it. I don't know.
To connect a vein to an artery, it's against their nature. I mean you connect an oxygenated body of blood with one that should be clear, and in this case you bring toxins to the brain and that's not a good idea.
DISCUSSION
Among ESRD patients who are deemed eligible for both PD and HD, factors relevant to their modality decision-making were identified with respect to physical strength/dexterity and having a sound mind (Capability), external forces and constraints (Opportunity), and values and beliefs (Motivation). For most patients, a combination of factors led to the choice of a particular dialysis modality. However, preferences for PD were primarily based around convenience and maintaining a normal life. Although there were a number of reasons identified for choosing HD, the majority reported a heightened sense of security as a reason for selecting this modality. Concerns surrounding relative efficacy of one dialysis modality over another was not raised by anyone interviewed; patients were more concerned about the potential impact of a dialysis modality on their quality of life.
It has previously been noted that a reason behind patients' perceived lack of individual choice in decision-making about treatment relates to lack of information [14]. In fact, a recent systematic review found that patient-targeted educational interventions were associated with a 2-fold increase in the odds of a patient choosing PD [18]. Patients in our study were uniformly provided modality education for both types of dialysis, enabling identification of key factors behind patients' dialysis modality selection. The COM-B and TDF tools [16, 17] were helpful instruments in aiding the development of a coding scheme applicable to the evaluation of dialysis modality selection. The identified fundamental themes of physical strength/dexterity and having a sound mind, external forces and constraints, and values and beliefs correspond closely to the respective components of the ‘behavioral system’—capability, opportunity and motivation. Indeed, there is a close parallel between patient-level barriers to PD and the potential barriers to implementing practice change which the TDF and COM-B tools were designed to evaluate.
Older age has not been found to be associated with lower PD eligibility in adjusted analyses after accounting for barriers to self-care and family support [19]. This possibly suggests that the consistent association between older age and low PD utilization in the literature occurs because older patients have barriers to self-care and are therefore, not offered, or do not choose PD. Furthermore, availability of home care assistance has been shown to significantly increase the number of patients who can be safely offered PD by overcoming some of the barriers to self-care [20]. At the study site, home care assistance was available to PD eligible patients, though none of the study participants interviewed had utilized this service. In relation to patient's modality decision-making, we have identified several barriers to the administration of PD at home. Patients' modality choice stemmed mostly from their intrinsic values and beliefs, and to a lesser extent, external forces and constraints. Their selection of a particular dialysis modality is very much individualistic and reflects what they value more: the convenience and maintenance of a normal life provided by PD versus the heightened sense of security afforded by in-center HD.
Based on the themes identified, we endeavor to offer several practical suggestions that target potential interventions to the identified barriers. First, dialysis modality education should include identifying any potential physical or cognitive barriers and then appropriately linking patients to available home care supports to help address any such issues related to PD (capability and opportunity barriers). Additionally, it may be quite influential to offer patients the opportunity to speak to current PD patients and to observe the actual dialysis process in their home environments (opportunity barrier). A previous systematic review of qualitative studies looking into the patients' perspectives surrounding decision-making regarding treatment for CKD noted the importance of peer influence [14]. Thirdly, the proposition of HD as a backup should PD fail may provide a reassuring influence for some patients (motivation barrier). Fourth, the timing of modality education may play a pivotal role for some patients deciding between the different dialysis modalities (motivation barriers). In fact, timing of information has been noted to be a major factor influencing decision-making among patients with CKD [14]. For uremic patients who are in need of renal replacement therapy in the imminent future, some may naturally prefer the nursing support provided by HD given their general poor state of health at that time. Their perception may evolve once they start feeling better on dialysis, though this is countered by patients' preference for maintaining the status quo, which has previously been noted to be a key factor in influencing decision-making [14]. Once a definitive vascular access has been created, patients may be even more resistant to consider an alternative dialysis modality.
We recognize several limitations to our study. There may be patient-perceived PD barriers specific to certain cultures and these may not have been fully captured in our study. Although the HD unit used to recruit study participants does serve a diverse, multi-cultural population and our study participants reflected this, our study excluded non-English-speaking patients to avoid miscoding of data and took place in a single center. Furthermore, although the modality education was intended to be unbiased, the content of the modality educations may have influenced patients' perceptions of the relative advantages and disadvantages of PD and HD. There are also important strengths to our study. We aimed to identify barriers to PD perceived by older patients by focusing on older patients who have been systematically determined to be eligible for both dialysis modalities. All patients were provided uniform dialysis education and allowed to freely choose their preferred dialysis modality. Furthermore, to minimize reporting bias, we excluded patients who had selected their preferred dialysis modality in excess of 6 months ago.
In conclusion, we have identified patient-perceived factors and barriers that may influence older individuals' choice of dialysis modality in those who are candidates for either HD or PD. Patients' decision-making truly reflected their intrinsic preferences without any potential influences from physical and social PD contraindications or intentional biases in modality education. The choice of a particular dialysis modality was largely based on a combination of factors. However, older patients who selected PD appeared to value convenience and maintaining a normal life, while older patients who selected HD valued the perceived associated heightened sense of security. These factors should be considered and/or addressed by PD programs if they seek to make PD a more appealing modality option to individuals with ESRD.
SUPPLEMENTARY DATA
Supplementary data are available online at http://ndt.oxfordjournals.org.
ACKNOWLEDGEMENTS
We would like to acknowledge the support of all the staff associated with the home dialysis program at Sunnybrook Health Sciences Centre and thank all the study participants for their time and willingness to share their unique perspectives. Also, the countless hours that Ms Monika Khoury-Dool spent transcribing the interviews is very much appreciated.
AUTHORS' CONTRIBUTIONS
Research idea and study design: B.W.; data acquisition: B.W.; data analysis/interpretation: B.W., L.V., J.H.-L.; supervision or mentorship: L.V., M.O., R.Q., P.R., J.H.-L. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. B.W. takes responsibility that this study has been reported honestly, accurately, and transparently; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
CONFLICT OF INTEREST STATEMENT
M.O. and R.Q. are Co-inventors of the Dialysis Measurement Analysis and Reporting (DMAR) system. They receive support from Baxter Healthcare to build a PD catheter registry for the North American Research Consortium of the International Society of Peritoneal Dialysis. The results presented in this paper have not been published previously in whole or part, except in abstract format.
REFERENCES





Comments