-
PDF
- Split View
-
Views
-
Cite
Cite
Naoki Kondo, Tomotake Kanai, Kazuya Yamada, Yusuke Sakazume, Satoshi Tabata, Fumie Ikarashi, Mayuko Takano, Takahiro Watanabe, Rika Kakutani, Yasufumi Kijima, Hiroyuki Kawashima, Hajime Ishikawa, Modified Boyes’ procedure for the multiple finger extensor tendon ruptures in patients with rheumatoid arthritis: A report of two cases, Modern Rheumatology Case Reports, Volume 7, Issue 1, January 2023, Pages 28–33, https://doi.org/10.1093/mrcr/rxac050
Close - Share Icon Share
ABSTRACT
Multiple subcutaneous extensor tendon ruptures in more than the ulnar three fingers sometimes occur in patients with rheumatoid arthritis accompanied by wrist deformity. In these situations, the flexor digitorum superficialis tendon of the middle finger (the FDS3 tendon) and that of the ring finger (the FDS4 tendon) are used for the transferred tendon (modified Boyes’ procedure). Here, we treated two patients with rheumatoid arthritis, whose extensor tendons of more than three fingers were ruptured, using the modified Boyes’ procedure. Case 1 had ruptures in four fingers (index through little), and Case 2 had ruptures in three fingers (middle through little). The FDS3 and FDS4 tendons were passed subcutaneously around the radial side of the wrist to the extensor sides and interlaced with the distal stump of the ruptured tendons. Switching of the finger movement was achieved smoothly in both cases. The post-operative evaluation showed an extension lag of −15° for the index finger 0° for the middle through the little fingers in Case 1, and 0° for the middle finger and −5° for the ring and little fingers in Case 2. The average post-operative extension lag was −3.5°. However, median nerve palsy occurred in both cases, and it gradually recovered. Stretching of the nerve by the correction of the wrist deformity and increased pressure in the carpal tunnel were supposed to be causes of this palsy. Modified Boyes’ procedure is a useful method for more than three ulnar finger extensor tendon ruptures; however, post-operative median nerve palsy should be considered.
Introduction
Rheumatoid arthritis (RA) is a chronic, systemic inflammatory disease that causes progressive joint damage leading to disability throughout life [1]. Approximately 70% of patients with RA develop pathologies of the hand [2]. Joint damage, including metacarpophalangeal (MP) joints, proximal interphalangeal joints, and subcutaneous tendon ruptures, is observed in quite a few patients with RA, and these events lead to severe deformities and impairment of gripping, grasping, and pinching [2].
Subcutaneous ruptures of the extensor tendons due to RA are still incident and require reconstruction surgery [3, 4]. In a recent report, the incidence of the extensor tendon rupture in rheumatoid patients was 4% (61 out of 1572 cases of rheumatoid wrists) [5]. Extensor tendon ruptures occurred at mechanically stressed sites, and the most frequent site was the extensor pollicis longus tendon (21 tendons), followed by the little finger extensor tendon (14 tendons), the ring finger extensor tendon (11 tendons), and other tendons [5].
Synovitis of the distal radioulnar joint often occurs in patients with RA, the protruded, deformed, and unstable ulnar head causes mechanical stress, and adjacent tendons such as the extensor digiti minimi (EDM), extensor digitorum communis (EDC)5, and EDC4 are vulnerable to the friction force exerted by the ulnar distal end [6].
Extensor tendon ruptures mainly occur in the little and ring fingers. Moore et al. reported that the EDC5 tendon is the most common, followed by the EDC4, the EDM, the EDC3, and extensor pollicis longus for tendon ruptures [7]. The treatment strategy is well established in cases of up to two ulnar finger extensor tendon ruptures. In the case of extensor tendon ruptures of the little finger, end-to-side suture from the distal end of the little finger to the intact ring finger is performed [2]. In case of ruptures of the extensor tendon of both the ring and little fingers, end-to-side suture from these fingers’ distal ends to the intact long finger is performed. Another option is to transfer the extensor indicis proprius (EIP) tendon to the distal ends of the ring and little fingers [2]. When the middle, ring, and little fingers are ruptured, the EIP can be used to power the ring and little fingers, and the middle finger extensor tendon can be sutured to the index communis extensor tendon [2].
However, multiple finger ruptures of more than three ulnar fingers, such as the middle finger and index finger extensor tendon rupture, sometimes occur because the EIP and EDC tendons for the index, middle, ring, and little fingers are located in the ‘same’ fourth dorsal compartment of the extensor tendons. In one report, 61% (38 hands out of 62 hands) had three or more extensor tendon ruptures [4]; therefore, rheumatologists cannot ignore multiple finger extensor tendon ruptures as a complication. In such cases, reconstruction as a treatment is difficult because the ipsilateral middle finger cannot be used as the donor tendon. The EIP tendon is used for tendon transfer, and the palmaris longus (PL) tendon is used for free tendon grafts [8]. Some reports have shown good clinical outcomes [9], but the use of the EIP tendon tends to result in poor outcomes because its muscle power is too weak to extend the three fingers fully. Free tendon interposition grafting using the PL tendon showed good results for 16 ruptured extensor tendons in seven wrists [10].
The flexor digitorum superficialis (FDS) tendon transfer was originally advocated by Boyes for radial nerve palsy. Patients who received this method learned to use a former finger flexor as an extensor. This method has also been used for extensor tendon ruptures of three or four fingers in the rheumatoid wrist [6, 11, 12].
In the original Boyes’ procedure, the FDS tendon is passed through the interosseous membrane of the forearm [11, 12]. In the modified Boyes’ procedure, the FDS tendon is passed through the subcutaneous tunnel at the distal radial forearm (at the level of the wrist joint) to correct the ulnar deviation of the fingers by pulling the tendons from the radial side of the forearm [6]. The usefulness of the modified Boyes’ procedure has not yet been elucidated in clinical settings. In addition, the technical challenges in the surgery, rehabilitation after surgery, and functional outcomes have not been clarified.
Here, we report the treatment experience of two RA patients who underwent tendon transfer using the modified Boyes’ procedure for multiple extensor tendon ruptures and recommend this method as a useful treatment option for three or more extensor tendon ruptures in patients with RA.
Case presentations
Written informed consent was obtained from both patients for publication of this case report and accompanying images. All the procedures were conducted in accordance with the Declaration of Helsinki (1964). Ethics Committee approval was obtained from Niigata University Medical and Dental Hospital (2018-0377).
Case 1
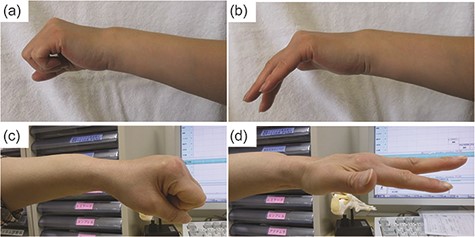
A 47-year-old right-handed woman, with RA for 20 years, complained that she could not hold things with her left hand. She was treated with 8 mg/week of methotrexate (MTX) and 3 mg/day of prednisolone (PSL). Although she could perform full grip motion (Figure 1(a)), she could not actively extend her left index through the little fingers. The active extension angles were −65°, −65°, −50°, and −50° in the index, middle, ring, and little fingers, respectively (Figure 1(b)).
Radiography of the wrist joint demonstrated Larsen grade IV findings and remarkable ulnar deviation in the proximal ray of the carpal bones (Figure 2(a,b)). She was diagnosed with a subcutaneous extensor tendon rupture of the index through the little fingers (four fingers). We performed left wrist arthrodesis (Feldon’s method) using Darrach’s procedure (Figure 2(c,d)), synovectomy of the wrist joint, and tendon reconstruction.

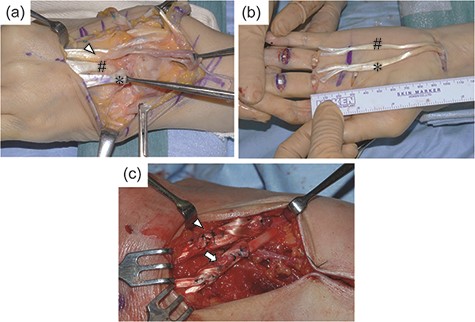
Intraoperatively, complete rupture of the EDM tendon, the EDC tendons of the index through the little fingers, and the EIP tendon were identified (Figures 3(a)). For tendon reconstruction, a tendon transfer method (modified Boyes’ procedure) was selected. The third and fourth superficial FDS tendons were pulled out from the proximal palmar region (Figure 3(b)) and passed subcutaneously around the radial side of the wrist to the extensor side and interlaced with the distal stump of the ruptured tendons. The FDS3 tendon was sutured with the EDC2 and EDC3 tendons, whereas the FDS4 tendon was sutured with the EDC4 and EDC5 tendons in an interlacing fashion, respectively (Figure 3(c)).
After surgery, a continuous local analgesic-injectable catheter was placed into the brachial plexus for 5 days. On Day 6 after surgery, the catheter was removed; however, numbness in the median nerve region remained, and the patient was diagnosed with median nerve palsy. On Day 8 after the primary surgery, the left carpal tunnel was released, and the median nerve was neurolysed. Sensory numbness gradually improved, and the patient completely recovered 8 months after the surgery.
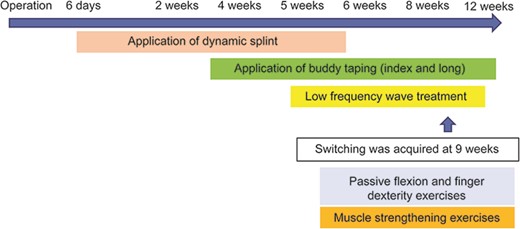
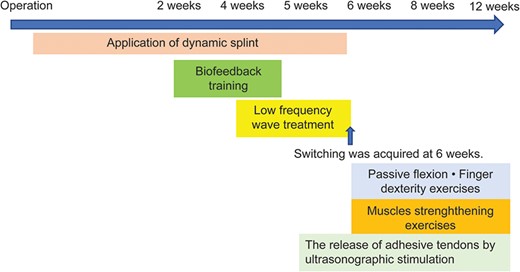
For occupational therapy, a dynamic splint was applied for 6 weeks after surgery, and active flexion and passive extension exercises were performed. Low-frequency wave therapy was performed between 5 and 12 weeks after surgery, and switching ability was acquired at 9 weeks. Training for skill movements was performed for 12 weeks (Figure 4). One year after the surgery, the patient was able to grip up to full range (Figure 1(c)), and active extension was −15° for the index finger and 0° for the middle through the little fingers (Figure 1(d)).
Case 2
A 56-year-old right-handed woman, with RA for 9 years, complained that she could not hold things with her right hand. She had been treated with 6 mg/week of MTX, 1 g/day of salazosulfapyridine, 200 mg/day of bucillamine, and 2.5 mg/day of PSL. Active flexion of the right middle through the little fingers was impossible. The active extension angles were −50°, −70°, and −70° in the middle, ring, and little fingers, respectively (Figure 5(a)). Radiography of the wrist joint demonstrated Larsen grade IV findings and spontaneous fusion of the radiolunate joint (Figure 6(a,b). We performed Darrach’s procedure (Figure 6(c,d)), synovectomy, and tendon reconstruction using the modified Boyes’ procedure. Intraoperatively, the EDM and EDC tendons of the middle through the little fingers were subcutaneously ruptured (Figure 7(a)).


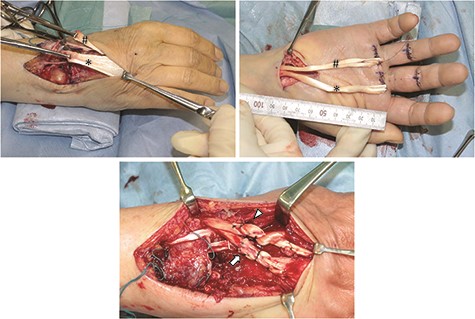
The FDS3 and FDS4 tendons were subcutaneously passed through (Figure 7(b)) and transferred to the dorsal side of the wrist. The radial sensory nerve was identified and released sufficiently to prevent contact with the FDS tendons. The FDS3 tendon was sutured with the EDC3 tendon, and the FDS4 tendon was sutured with the EDC4 and EDC5 tendons in an interlacing fashion, respectively (Figure 7(c)). In addition, we also performed carpal tunnel release to prevent post-operative median nerve palsy. We reconfirmed that the FDS tendons did not kink the median nerve.
For occupational therapy, a dynamic splint was applied for 6 weeks after surgery, and active flexion and passive extension exercises were performed. Biofeedback exercise was performed from 2 to 5 weeks after surgery. Low-frequency wave therapy was performed between 4 and 6 weeks after surgery, and switching ability was acquired at 6 weeks. Training for skill movements was performed for 12 weeks (Figure 8). One and a half years after the surgery, she was able to grip up to full range, and active extension was 0° for the middle finger and −5° for the ring and little fingers (Figure 5(b)). Immediately after the surgery, sensory numbness was detected in the median nerve region; however, it gradually improved in 12 weeks and the patient was able to grip up to full range.
The pre-operative Disabilities of the Arm, Shoulder and Hand (DASH) score [13] was 23.2 points. The DASH score improved to 3.7 points at 1.5 years after the surgery. She felt slight sensory numbness only at the tip of the thumb, index, and middle fingers.
Discussion
We consider these two cases to be worth reporting because the modified Boyes’ procedure is a useful method for three or more extensor tendon ruptures in patients with RA. Extensor tendon reconstruction is advised in patients with subcutaneous rupture of the extensor tendon due to RA.
The greater the number of ruptured extensor tendons, the more adverse the post-operative outcome [4]. Yoshizuka et al. defined an MP joint extension of >20° or an MP joint flexion <50° at 6 months after the reconstruction surgery as a poor outcome and reported that four out of eight poor outcome cases were triple extensor tendon ruptures [14]. They used end-to-side sutures of the ruptured EDC3 to EDC2 and EIP or PL tendon transfer as the reconstruction surgical procedure.
Useful and appropriate surgical procedures have not been established for cases of multiple finger tendon ruptures of more than three fingers [15]. Suzuki et al. compared the outcomes of four different surgical reconstructions for triple extensor tendon ruptures in the ulnar three fingers in 48 patients with RA. The surgical procedures were PL tendon grafting, EIP tendon transfers, end-to-side transfers with tension-reduced early mobilisation, or a combination of end-to-side and EIP transfers. The combination group showed the best clinical outcomes with the average MP joint extension (−3°), followed by the end-to-side (−12°), the EIP (−16°), and the PL (−21°) groups, respectively. They concluded that the combination of end-to-side and EIP transfer was an effective surgical reconstruction procedure for triple extensor tendon ruptures [16].
Another option is FDS tendon transfer. The tendon chosen as a donor for transfer must be sufficiently strong to perform its new function in its altered position. Of the forearm muscles, the FDS is the most powerful donor muscle (4.8 m-kg of work capacity) compared to other nominated tendons, such as FDP (4.5 m-kg), flexor carpi ulnaris (FCU) (2.0 m-kg), brachioradialis (1.9 m-kg), pronator teres (1.2 m-kg), flexor pollicis longus (1.2 m-kg), flexor carpi radialis (FCR) (0.8 m-kg), and PL (0.1 m-kg) for reconstruction, which makes it possible for the FDS to get sufficient amplitude as a donor tendon [17].
Compared to FDS3 or FDS4, FCR or FCU has extremely poor tendon excursion. And when FCR or FCU is used, its length is not long enough, so a free tendon grafting is needed to reach the distal end of the ruptured tendons. Actually, the tendon excursion of FCR and FCU is 35–50 and 33–44 mm, respectively. Those lengths are significantly shorter than the excursion of 65–88 mm in FDS3 and 65 mm in FDS4 [18]. The superior outcome can be acquired by using FDS3 and FDS4 as a source of force.
Chung et al. examined the clinical outcomes of 46 patients (51 wrists) with extensor tendon ruptures due to rheumatoid wrists. The mean post-operative extension lag was −8°, and the satisfactory score was 74. The lower the extension lag, the better the satisfactory score [19].
In our two cases, the extension lag of one finger was more than −10°, and those of the other six fingers were less than −8°. The mean MP extension lag was −3.6° (−15 to 0°), which was comparable to the combination procedure of end-to-side and EIP transfer [16].
The limitations of this procedure were post-operative median nerve palsy and decreased dexterity due to the difficulty in switching the finger movement. In fact, Motomiya reported one case of decreased dexterity due to the difficulty of switching [20]. In our case, switching was successfully achieved in both cases.
The median nerve was stretched by the correction of deformity with arthrodesis in Case 1. Post-operative swelling increased the pressure in the carpal tunnel. These two factors were the main causes of post-operative median nerve palsy. In Case 2, the median nerve was not supposed to be stretched because this case was performed using only Darrach’s procedure. It was desirable to release the carpal tunnel when the wrist joint surgery was performed combined with this kind of tendon surgery. The median nerve was sufficiently released, and the FDS tendons were transferred far from the path of the median nerve. However, median nerve palsy was incident, even in Case 2.
Median nerve palsy should be paid the most careful attention in the modified Boyes’ procedure. The main technical challenges of modified Boyes’ are to release the median nerve thoroughly and pull up the transferred FDS tendons as proximally as possible by releasing the forearm fascia not to constrict the median nerve.
The limitations of this report are that (1) only two cases are not sufficient to detect the genuine efficacy of the modified Boyes’ procedure and (2) the results of this procedure were not compared with the group of EIP tendon transfer and the end-to-side suture of the EDC3 tendon to the EDC2 tendon in case of three-finger tendon ruptures.
In conclusion, the modified Boyes’ procedure is a method that uses FDS tendons as the transferred tendons for multiple finger extensor tendon ruptures, and the FDS tendons are passed through the subcutaneous tunnel. We encountered two patients with RA with multiple finger extensor tendon ruptures who underwent the modified Boyes’ procedure. It is useful for the functional recovery of finger extension, although post-operative median nerve palsy needs attention.
Conflict of interest
None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Patient consent
Written informed consent was obtained from both patients for publication of this case report and accompanying images. All the procedures were conducted in accordance with the Declaration of Helsinki (1964).
Ethical approval
Ethics Committee approval was obtained from Niigata University Medical and Dental Hospital (2018-0377).
Author contributions
N.K. performed surgery and organised this case report. N.K. and K.Y. collected images and prepared all the figures. H.I. supervised the surgical procedure. N.K. wrote the manuscript. T.K., Y.S., S.T., F.I., M.T., T.W., R.K., Y.K., H.K., and H.I. read and reviewed the manuscript and have approved the submission.



