-
PDF
- Split View
-
Views
-
Cite
Cite
Curtis M Craig, Katelyn R Schwieters, Bradley A Drahos, Nichole L Morris, A Pilot Study on the Role of Experience and Patient Gender on MARCH Treatment Sequence, Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e2041–e2048, https://doi.org/10.1093/milmed/usac383
Close - Share Icon Share
ABSTRACT
The brevity of training for soldiers and combat medics to learn how to provide treatment on the battlefield may restrict optimal performance for treating chest and airway injuries, particularly when treating female soldiers. The present study tested treatment performance on patient simulators by battlefield medic trainees to determine whether there is a need for more extensive training on chest and airway procedures on female soldiers.
Battlefield medic trainees treated male and female patient simulators in counterbalanced order. The assessment considered the effects of patient gender and order on procedures performed, particularly critical chest and airway interventions such as needle chest decompression (NCD), and considered the appropriate order of treatment tasks. Four coders rated video footage of three simulated procedures, i.e., tourniquet, chest seal (front and back application), and NCD, using a binary coding system to determine completeness and order correctness according to the Massive hemorrhage, Airway, Respiration, Circulation, and Head injury/Hypothermia (MARCH) mnemonic.
Results from analysis of variance showed that when presented with a female patient first, trainees performed significantly fewer total procedures on both the female and male simulators. More experienced trainees completed significantly more procedures compared to trainees with minimal experience. Results from the binary logistic regression showed that trainees with more experience and trainees presented with the male patient simulator first performed significantly more procedures in the correct order. Finally, an examination of the NCD procedure found that trainees presented with the female patient simulator first had more errors and that trainees with less experience were less likely to perform the procedure adequately.
The findings suggest that treating a female patient first may lead to undertreatment of both patients. Furthermore, the observed differences in treating sensitive areas of the body (e.g., near female breasts) suggest providing greater opportunities for trainees to practice often missed or incorrectly performed procedures. Treating a female patient remains a novel experience for many trainees, such that trainees are less likely to fully treat a female patient and are less likely to treat female soldiers for the most life-threatening injuries. In fact, the initial presentation of the female patient simulator appeared to affect experienced trainees, suggesting that removing the experience of novelty and stress requires more extensive exposure and alternative training. The study’s small sample size with a wide range of trainee experience may limit the findings, which may fail to capture some study effects. Finally, the study did not request trainees’ experience treating female soldiers, so future studies should examine the extent to which experience is predictive of performance. There is a need for more interactive approaches in patient simulations to provide opportunities for practice, especially those that require the treatment of sensitive areas.
INTRODUCTION
Responding to a combat casualty on the battlefield requires rescuers to engage in a set of difficult and rapid decision-making processes when assessing and treating a fellow soldier for what are potentially life-threatening injuries. The early interventions during the resuscitation of a casualty may influence patient outcomes,1 and a variety of contextual factors influences medical decision-making, including the visual presentation or characteristics of the patient.2 In military medicine, the mechanism or type of injury affects decisions regarding medical evacuation and triage of combat casualties, patient stability for transport, evacuation timelines, and biases in decision-making.3 Furthermore, the experience level influences military medical decision-making and performance in treating multiple casualties. Past studies show that when treating two patients, novice emergency responders either were very thorough in treating only one of the patients or conducted basic treatment on both patients, while more experienced paramedics provided more thorough, balanced care to both patients, suggesting that novices and experts may be enabling different cognitive strategies while treating patients.4 Similarly, first-year first responders’ ability to apply the Sort, Assess, Lifesaving interventions, Treatment/Transport triage algorithm accurately decreased 3 months after completing initial training, and over-triaging was a frequently made error.5
Novice Trainees and Combat Medic Simulation Training
Given the aforementioned complexity of the battlefield resuscitation processes, training rescuers in military medicine is constrained by limited training time focused on a pool of nonphysician paraprofessionals (i.e., novices),6 which prevents initial development of rapid and effective heuristic decision-making that is effective in complex domains.7 To better facilitate skill acquisition both for combat medics and basic combat lifesavers (CLSs), training focuses on instruction in useful algorithmic procedures taught both pedagogically and through simulation.8 The use of simulation has been widely accepted in medical education and can be used to enhance new skill sets, maintain existing skill sets, or assess the effectiveness of such interventions in practice.9 Simulation is effective because it allows for practicing problem scenarios in a realistic context similar in both concrete features and core concepts to the real-life scenario,10 which promotes the best transfer of learning for novices.11 Generally, repeated trauma simulation leads to improvements in prehospital trauma care.12
MARCH Mnemonic
The typical treatment protocol for a combat casualty on the battlefield requires rescuers to follow a standardized treatment algorithm to assess the patient’s body for injuries. Training rescuers in military medicine relies on skill-based training of critical procedures, emphasizing the ability to learn and perform a series of specific procedures that comprise a critical life-saving task by following a patient assessment algorithm to assess and treat in order: Massive hemorrhage, Airway, Respiration, Circulation, and Head injury/Hypothermia (MARCH).6,13 The MARCH mnemonic, see Figure 1, is a reliable checklist used by Tactical Combat Casualty Care (TCCC)-trained individuals (e.g., pararescuemen, corpsmen, and medics) to help remember the proper order of treatment when providing tactical field care and tactical evacuation during combat operations.14,15
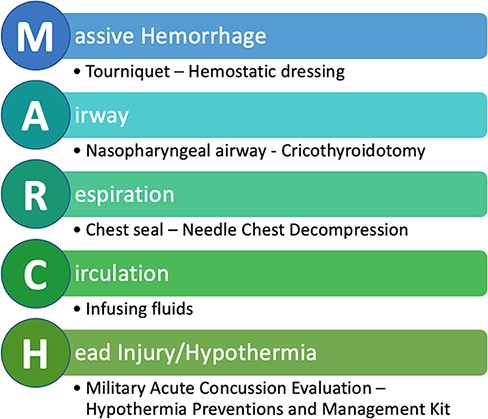
MARCH mnemonic and associated procedures in proper treatment order modified from the Tactical Combat Casualty Care Handbook, Version 5.
Order Errors/Task Sequence
Procedural tasks (e.g., MARCH) require an individual to follow a certain sequence of actions.16,17 High demands on attention and low automaticity mark the early phases of skill acquisition.18 Novices do not have easy recognition of the applicable situation, nor do they easily recall the relevant steps and order they should follow, and this need to effortfully recognize and recall leads to higher mental demands on those less-practiced.19 Furthermore, unusual or novel events and stimuli,20 distractions and interruptions,17 and stress21 may effectively overload the available mental resources an individual needs to correctly respond to a situation that they otherwise might perform well. Thus, even though people may know what the correct steps are, they sometimes fail to execute them correctly.22
Chest/Airway Injuries and Female Soldiers
Correct and rapid recognition of the applicable trauma care scenario and recall of the correct treatment steps and their order are critical for saving lives. The MARCH algorithm teaches first responders the proper order for treating the most immediate and critical situations first.14 Urgent battlefield casualties often require life-saving interventions, and a lack of intervention or delay of intervention is associated with increased mortality.23
An intervention most frequently performed incorrectly or missed altogether during prehospital combat medic activity is the treatment of chest injuries.1,24,25 Less frequently performed procedures show higher rates of incorrectly performed intervention, suggesting that a lack of exposure to chest injuries may contribute to skill degradation in performing chest interventions when such interventions become necessary.1
The military active duty population is growing increasingly diverse with 16.9% of its active duty population consisting of women.26 As the military diversifies, so does the need to recognize that there may be differences in risk of injury on the battlefield. Female soldiers are also at a greater risk of chest and abdomen injuries and have overall higher death rates compared to male soldiers.27,28 Rescuers often take longer to expose a female patient (i.e., are more reluctant) to diagnose injuries to the chest and torso, and more medical errors occur when treating a female patient.29,30
Enhancing combat medic simulation training with a focus on chest and airway procedures may be an effective countermeasure to this issue. However, widely available patient simulators are often masculine in appearance.31 Limiting trainees to only male simulators may be inadequate in terms of transferring learning of procedures to female patients. When trainees first performed treatment of a simulated gunshot wound (GSW) on a female patient simulator, they tended to commit more errors on the female patient simulator than the male patient simulator, even when controlling for trainee experience.32 Therefore, it is important to prepare trainees to treat both female and male casualties, especially for treating sensitive areas of the body that are anatomically different (e.g., chest).32
Current Study
To explore this potential issue, we present the results of a battlefield trauma care simulation study performed with combat medic trainees to treat a series of typical battlefield wounds on male and female-retrofitted patient simulators. The applicable task order to follow was MARCH. We hypothesized that female patient simulators are a novel experience because of their scarcity, which increases mental demand and draws trainees’ attention from the treatment task. Furthermore, we hypothesized that because of the social scrutiny and expectations around the treatment of women’s bodies (e.g., trainee exposure to the Sexual Harassment/Assault Response and Prevention or SHARP program), trainees will experience stress.21 Based on these hypotheses, we predicted that combat medicine trainees, particularly novices, will perform more poorly, i.e., more errors in the critical task order and a higher likelihood of forgetting procedures, on novel female patient simulators while treating sensitive area injuries (e.g., chest) compared to standard male patient simulators.
METHOD
Participants
In total, 36 participants (n = 8 or 22.2% female) completed the study. Fifteen participants had the designation of CLSs, 19 were combat medics, one participant had other designations (e.g., Ophthalmic Tech), and one participant had no medical training. Participants’ designated experience ranged from 2 days to 17.5 years. For experience, nine (25%) of the trainees had less than 1 month of experience, 10 (27.8%) of the trainees had less than 2 years of experience, 15 (41.7%) of the trainees had more than 2 years of experience, and two (5.6%) did not report their experience. The age range was 18-41 years old, with 27 (75.0%) of participants between 18 and 29 years and nine (25%) were between 30 and 41 years.
Design
The overall purpose of this study was to analyze potential performance gaps between patient gender using male and female-retrofitted simulators in a military medical training scenario. To accomplish this, the experiment was a mixed factorial with patient simulator gender as the within-subjects variable and patient simulator order as the between-subjects variable. This resulted in a 2 (Female Simulator, Male Simulator) × 2 (Female First, Male First) design, with participants randomly assigned to each condition.
Procedure
Participants were first provided an information sheet covering the basic details of the study and provided a reminder that participation was voluntary and confidential, with no consequences for choosing to withdraw or participate. The research staff provided a verbal review of the information sheet details and obtained verbal consent from those individuals who elected to participate. To analyze potential performance gaps between patient gender, each participant conducted the following procedures on male and female-retrofitted simulators: massive hemorrhage control via tourniquet application, treatment of entrance and exit GSWs/penetrating wounds via chest seal application, and pneumothorax (collapsed lung) via needle chest decompression (NCD). In addition to previous familiarity with MARCH, researchers briefed participants before participation that these procedures were of some importance during the simulation both by staff and instructor. Researchers fitted participants with a GarminTM video camera mounted to a combat helmet to record and time procedures. Researchers and medical simulation training center instructors briefed participants that they would be consecutively treating two patients with the same injuries and should quickly render care by performing hemorrhage control, addressing a GSW, and performing an NCD using an aid bag of necessary supplies. Half of the participants performed procedures on the male simulator first, and half of the participants performed procedures on the female-retrofitted simulator first. Following the completion of treatment for both patients, the participants received instructor feedback on their performance, performed a short debrief interview with research staff, and answered a short list of survey questions.
The study team and medical simulation training center staff created two separate participant testing lanes with two SimMan® 3G patient simulators in each lane. Gender modifications to one simulator in each lane included replacing the torso skin with the female Gender Retrofit Kit produced by SIMETRI, a wig, and makeup. Uniform clothing between the simulators was nearly identical apart from a nude sports bra underneath the standard undershirt of the female patient.
Materials and Measures
Four trained coders rated video footage of the tactical field care scenario using a scoring metric created based on the TCCC MARCH guidelines. Three procedures (i.e., tourniquet, chest seal [chest seal 1/entrance GSW and chest seal 2/exit GSW], and NCD) were of primary focus for this analysis and were of key importance. For each procedure, coders used a binary coding system to indicate correctness of the procedure according to TCCC standards (yes/no) and correctness of the order according to MARCH (yes/no). To ensure interrater reliability (IRR), all four coders completed the process for coding participant procedure order and correctness for a small subset of the participants. Following demonstration of IRR, two team members coded half of the participant recordings, and the other two members coded the remaining participant recordings.
Total procedures completed correctly
The team calculated a sum of correct procedures for each participant for both the male and female-retrofitted patients. The computed value represents the total number of procedures completed. Procedures, each with a value of 1, assessed in accordance with TCCC standards included: tourniquet application to the amputated leg, chest seal treatment of the GSW on the chest, chest seal treatment of the GSW on the back, and NCD, for a maximum score of 4. It is important to note that this score, aimed at measuring general correct treatment application, is independent of whether the participants completed the procedures in the correct order according to MARCH.
Correct order
A correct order value was generated for each patient, i.e., male and retrofitted female, of each participant. This value is a binary value, in which the participant either attempted (i.e., independent of correctness of performance) each of the three key procedures in the correct order, as specified through MARCH, or failed to do so. According to MARCH, the correct order for completing the three key procedures is tourniquet application (M—massive hemorrhage), GSW treatment using chest seals (R—respiration), and NCD (R—respiration). This portion of the analysis primarily focuses on whether the participant followed the correct procedure order according to MARCH, not whether the participants performed the procedures correctly. If participants first applied the tourniquet on the injured left leg, identified and applied one or both chest seals, and then attempted to perform the NCD, this was considered a correct order (coded “yes”) and any other combination of procedures was considered an incorrect order (coded “no”).
RESULTS
Interrater Reliability
The four raters jointly coded two trainees performing two simulations each (male and female patients) for a potential maximum of four treatments per simulation. Each rater coded each task step with a label for the task type and time-stamped when they observed the task begin and end. When the coders used the same label and approximate start and end time range (3-second time deviation), then the coders agreed on that task step. Otherwise, the coders disagreed and labeled the nominal coding as a disagreement. Given multiple raters, the analysis used the IRR statistic, Fleiss’ kappa,33 Fleiss’ |$\kappa = $| 0.626, z = 5.36, p < .001, indicating a good level of agreement. The team reviewed any remaining disagreements in ratings and resolved to determine a final rating.
Descriptive Statistics
Trainee experience was not statistically different in the two treatment conditions (i.e., female first vs. male first), p = .189, nor was trainee gender, p = .691. Table I shows the frequency and percentages of participant characteristics for trainee experience and trainee gender in both participant groups.
Frequencies and Percentages of Trainee Characteristics by Treatment Condition
| Trainee characteristic . | Female first group, n (%) . | Male first group, n (%) . |
|---|---|---|
| Gender | ||
| Female | 3 (16.6) | 5 (27.0) |
| Male | 15 (83.3) | 13 (72.2) |
| Experience level | ||
| Less than 1 month | 5 (27.0) | 4 (22.2) |
| Less than 2 years | 3 (16.6) | 7 (38.9) |
| More than 2 years | 8 (44.4) | 7 (38.9) |
| Did not share experience | 2 (11.1) | 0 (0.0) |
| Trainee characteristic . | Female first group, n (%) . | Male first group, n (%) . |
|---|---|---|
| Gender | ||
| Female | 3 (16.6) | 5 (27.0) |
| Male | 15 (83.3) | 13 (72.2) |
| Experience level | ||
| Less than 1 month | 5 (27.0) | 4 (22.2) |
| Less than 2 years | 3 (16.6) | 7 (38.9) |
| More than 2 years | 8 (44.4) | 7 (38.9) |
| Did not share experience | 2 (11.1) | 0 (0.0) |
Percentages are presented in parentheses. Female first group, n = 18; male first group, n = 18.
Frequencies and Percentages of Trainee Characteristics by Treatment Condition
| Trainee characteristic . | Female first group, n (%) . | Male first group, n (%) . |
|---|---|---|
| Gender | ||
| Female | 3 (16.6) | 5 (27.0) |
| Male | 15 (83.3) | 13 (72.2) |
| Experience level | ||
| Less than 1 month | 5 (27.0) | 4 (22.2) |
| Less than 2 years | 3 (16.6) | 7 (38.9) |
| More than 2 years | 8 (44.4) | 7 (38.9) |
| Did not share experience | 2 (11.1) | 0 (0.0) |
| Trainee characteristic . | Female first group, n (%) . | Male first group, n (%) . |
|---|---|---|
| Gender | ||
| Female | 3 (16.6) | 5 (27.0) |
| Male | 15 (83.3) | 13 (72.2) |
| Experience level | ||
| Less than 1 month | 5 (27.0) | 4 (22.2) |
| Less than 2 years | 3 (16.6) | 7 (38.9) |
| More than 2 years | 8 (44.4) | 7 (38.9) |
| Did not share experience | 2 (11.1) | 0 (0.0) |
Percentages are presented in parentheses. Female first group, n = 18; male first group, n = 18.
The analysis computed means and standard deviations of total procedures for simulator gender, simulator order, and trainee experience. Overall, for the total number of procedures completed, there was a significant difference for simulator gender, with a fewer number of procedures being performed on the female simulator, t(71) = −25.217, p < .001, d = 0.20. Additionally, the average number of total procedures completed was lower for the female simulator when trainees treated the female simulator first, and by trainees with the least experience (i.e., less than 1 month), see Table II.
Means and Standard Deviations of Total Procedures for Simulator Gender, Simulator Order, and Trainee Experience
| Variable . | M . | SD . |
|---|---|---|
| Simulator gender | ||
| Female | 3.22 | 0.93 |
| Male | 3.39 | 0.77 |
| Simulator order | ||
| Female first | 3.11 | 0.71 |
| Male first | 3.50 | 0.94 |
| Trainee experience | ||
| <1 month | 3.00 | 0.69 |
| <2 years | 3.15 | 1.04 |
| >2 years | 3.67 | 0.66 |
| Variable . | M . | SD . |
|---|---|---|
| Simulator gender | ||
| Female | 3.22 | 0.93 |
| Male | 3.39 | 0.77 |
| Simulator order | ||
| Female first | 3.11 | 0.71 |
| Male first | 3.50 | 0.94 |
| Trainee experience | ||
| <1 month | 3.00 | 0.69 |
| <2 years | 3.15 | 1.04 |
| >2 years | 3.67 | 0.66 |
Total procedures have a maximum score of 4 (tourniquet, chest seal 1, chest seal 2, and needle chest decompression). The means presented here are weighted averages because of unequal sample sizes per condition.
Means and Standard Deviations of Total Procedures for Simulator Gender, Simulator Order, and Trainee Experience
| Variable . | M . | SD . |
|---|---|---|
| Simulator gender | ||
| Female | 3.22 | 0.93 |
| Male | 3.39 | 0.77 |
| Simulator order | ||
| Female first | 3.11 | 0.71 |
| Male first | 3.50 | 0.94 |
| Trainee experience | ||
| <1 month | 3.00 | 0.69 |
| <2 years | 3.15 | 1.04 |
| >2 years | 3.67 | 0.66 |
| Variable . | M . | SD . |
|---|---|---|
| Simulator gender | ||
| Female | 3.22 | 0.93 |
| Male | 3.39 | 0.77 |
| Simulator order | ||
| Female first | 3.11 | 0.71 |
| Male first | 3.50 | 0.94 |
| Trainee experience | ||
| <1 month | 3.00 | 0.69 |
| <2 years | 3.15 | 1.04 |
| >2 years | 3.67 | 0.66 |
Total procedures have a maximum score of 4 (tourniquet, chest seal 1, chest seal 2, and needle chest decompression). The means presented here are weighted averages because of unequal sample sizes per condition.
Total Procedures Completed
The constructed initial model examined the effects of simulator gender, simulator order, and trainee experience on the total number of procedures completed. We computed a type II ANOVA after removal of one significant outlier (Bonferroni p = .0059). There was a significant main effect of simulator order on the total number of procedures completed, F(1,62) = 8.485, p < .01, |$\eta _p^2$| = 0.12. Pairwise comparisons showed that there was a significant difference between getting the male or female simulator first (estimated marginal mean = 0.507, SE = 0.174, p < .01) on the total number of procedures completed. This suggests that trainees who treated the male simulator first completed more procedures on both patients compared to trainees who treated the female patient first, see Figure 2.
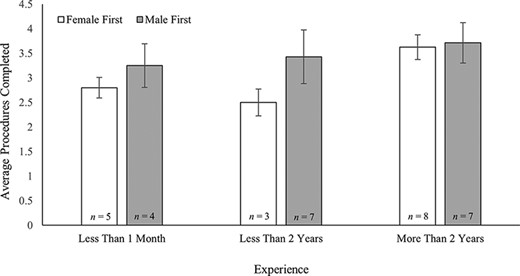
A graph of trainee experience level and simulator order on the average total number of procedures completed.
There was also a significant effect of trainee experience on the total number of procedures completed, F(2, 62) = 9.373, p < .001, |$\eta _p^2$| = 0.23. Pairwise comparisons showed that experience of 2 years or less significantly differed from experience of more than 2 years with a mean difference of −0.735 (SE = 0.206), p < .01. Additionally, experience of less than 1 month was significantly different from experience of more than 2 years on the total number of procedures completed, with a mean difference of −0.756 (SE = 0.208), p < .01. This suggests that those with more experience were significantly more likely to perform more total procedures compared to those with less experience, see Figure 2. Finally, there were no significant three- or two-way interaction effects between simulator order, patient gender, and trainee experience.
Correct Order
We conducted a binary logistic regression with patient simulator order, patient gender, and trainee experience on whether participants performed the three primed procedures (i.e., tourniquet, chest seal 1 and/or chest seal 2, and NCD) in the correct procedure order (yes/no). The model was significant, χ2 = 15.822, p < .01, explaining 28% of the variance in the correct procedure order (Nagelkerke R2). Those who received the female patient first were less likely to perform the procedure order correctly, B = −1.172 (SE = 0.574), p< .05 (odds ratio [OR] = 0.31, 95% CI, 0.101-0.954). Trainees with more experience were significantly more likely to perform the procedures in the correct order, B = 1.147 (SE = 0.360), p = .001 (OR = 3.150, 95% CI 1.555-6.373). An additional analysis considering the interaction between simulator order and trainee experience on the correct procedure order found no effect, χ2 = 4.311, p= .366, explaining 9% of the variance in the correct procedure order (Nagelkerke R2).
Completion of NCD Procedure
The NCD procedure is infrequently attempted in trauma patients and has a high failure rate because of factors such as inadequate ratios of chest wall thickness and catheter length and the general difficulty of diagnosing a tension pneumothorax in a prehospital setting.34 As such, it may be particularly prone to failure by novices, particularly where a female patient is concerned. A binomial logistic regression examined the effects of simulator order and trainee experience (i.e., less than 1 month, 2 years or less, and greater than 2 years) on performing the NCD procedure. There was a significant effect of simulator order on performing the NCD procedure. Those who had the female first were significantly less likely to perform the NCD, B = −1.813 (SE = 0.651), p < .01. The odds of performing the NCD correctly when treating the male simulator first was 2.477 (95% CI, 1.35-4.93) times the odds of treating a female simulator first. Participants completed the NCD procedure 80.6% (n = 29) of the time when participants had the male simulator first. However, participants completed the NCD procedure 50.0% (n = 18) of the time when they had the female simulator first.
There was also a significant effect of experience on performing the NCD procedure, with experience levels greater than 2 years significantly more likely to perform the NCD procedure, B = 2.366 (SE = 0.771), p < .01. Tukey’s multiple comparisons showed that those with more than 2 years of experience significantly differed from those with less than 1 month of experience on completing the NCD, estimate = 2.366 (SE = 0.771), p < .001. Completion rates for the NCD procedure were 38.9% (n = 7) for novice trainees (i.e., less than 1 month), 65.0% (n = 13) for trainees with 2 years of experience, and 83.3% (n = 25) for trainees with more than 2 years of experience.
Debrief Interview
After performing the procedure, participants broadly supported (n = 35, 97.2%) specific training for female patients. Questions were not explicitly asked about the frequency of their encounters with female patient simulators. However, a significant number (n = 12, 33.3%) of participants volunteered that they had no experience training with female patients and expressed that the experience would be helpful.
CONCLUSIONS
The present study tested treatment performance on patient simulators, considering effects of patient gender and order on procedures performed, particularly critical chest and airway interventions such as NCD, and considering the order of treatment tasks. The study results reflect a need to enhance the training for soldiers and combat medics to learn how to provide treatment on the battlefield and the need to provide better treatment for chest and airway injuries, particularly when casualties involve female soldiers. The hypothesis was that novice performers would be prone to have poorer performance in both the number of tasks performed and the order in which they performed because of heightened mental demand and stress in treating a female patient simulator. The study indicated partial support for this hypothesis.
Across both conditions, trainees averaged significantly fewer total procedures on female simulators compared to male simulators. Furthermore, when asked to treat a female patient first, trainees not only tended to average fewer total procedures on both simulators but were also significantly less likely to perform the procedures of interest in the correct order (i.e., follow the MARCH algorithm). Furthermore, participants who received the female patient simulator first were less likely to adequately perform the relatively more complex NCD task. Unsurprisingly, novice trainees were less likely to perform as well as more experienced trainees. However, there was no significant interaction between patient order and trainee experience, demonstrating that both inexperienced and more experienced trainees tended to perform more poorly (e.g., fewer procedures performed, procedures performed out of order, and NCD procedure completion) when treating the female patient simulator first compared to the male patient simulator. This finding suggests that for the presently assessed levels of experience, the novelty and stress involved in treating a female patient for chest and airway injuries were sufficient to disrupt recall of the correct response (e.g., order) to a learned situation.
Significance and Implications
Women have now been in active duty combat roles for more than 7 years. As such, it is important that training standards carefully consider inclusive design and allow for the opportunity to practice treating both female and male patients. This is especially important in consideration of chest and airway injuries, which may be especially susceptible to disruptions in performance.24–30
The findings from the current work suggest that treating a female patient first may lead to undertreatment of both patients. Gender biases in medical decision-making generally result in underdiagnosis of the neglected gender.35 Because trainees were treating patient simulators in quick succession, trainees may be relying on their recent memory to treat the second patient based on how they treated the first patient, which may have worked to their advantage when they treated the male patient first, but not when they treated the female patient first.
Furthermore, the observed differences in treating sensitive areas of the body (e.g., near female breasts) suggest providing greater opportunities for trainees to practice often missed or incorrectly performed procedures. Instituting focused continuous educational programs on perishable skills is a mitigating strategy that could potentially improve success rates of infrequently performed interventions, such as chest procedures.1 The current work suggests that the treatment of a female patient remains a novel experience for many trainees, such that trainees are less likely to fully treat a female patient and are less likely to treat female soldiers for the most life-threatening injuries. In fact, the initial presentation of the female patient simulator appeared to affect experienced trainees, suggesting that removing the experience of novelty and stress requires more extensive exposure and alternative training. Also, the inclusion of both combat medic trainees and CLS trainees in this study captures an important consideration of battlefield medicine: All soldiers should be trained in self-aid/buddy-aid to perform basic medical care in the field to save life or limb and since female soldiers have been authorized to serve in combat since 2015, this care must include them. The immediate and effective treatment of female battlefield casualties is critical and falls to both medical and nonmedical military occupational specialty codes alike.
Limitations
The present study has a relatively small sample size, which limits the ability to confidently extrapolate the findings and may lead to variable or biased results. Replication of this study with a comparative or larger sample is necessary. Furthermore, the wide range of trainee experience reported here may fail to capture some study effects, and future studies should test more constrained ranges (e.g., 1-2 years of experience). The study did not request trainees’ experience treating female soldiers, which limits confidence in the proposed hypothesis being correct, so future studies should examine the extent to which experience is predictive of performance. However, follow-up interviews indicated that many trainees had little to no experience treating female soldiers.
Proposals for Future Studies
Future research should not only consider the addition of diverse patient simulators to practice treating chest and airway injuries and female soldiers, but also consider other factors that may contribute to differences in patient care, such as symptom expression. The observed differences in treatment of male and female patients may be greater in the real world and potentially on the battlefield, as female and male patients tend to express symptoms differently.36 Thus, there is a need to use more interactive approaches in patient simulation to provide opportunities for practice, especially for those procedures that require treatment to sensitive areas of the body.
ACKNOWLEDGMENTS
First and foremost, the authors wish to thank Jack Norfleet, PhD, and Mark Mazzeo, MS, from the Army Combat Capabilities Development Command (DEVCOM) Soldier Center for their ongoing guidance and support on this work. The authors also wish to thank members of the research team including Timothy Kowalewski, PhD, and Mandi Lye for their support for this work.
FUNDING
This work was supported by the U.S. Department of Defense via the U.S. Army Combat Capabilities Development Command Soldier Center, Award Number W912CG2120002.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data that support the findings of this study are available on request from the corresponding author.
CLINICAL TRIAL REGISTRATION
Not applicable.
INSTITUTIONAL REVIEW BOARD (HUMAN SUBJECTS)
The study was reviewed by the University of Minnesota’s Institutional Review Board (STUDY00013436) and the U.S. Army DEVCOM Soldier Center (UN-210,003), both of which determined that it was “Not Human Subjects Research” as defined by U.S. Department of Health and Human Services and FDA regulation.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC)
Not applicable.
INSTITUTIONAL CLEARANCE
Not applicable.
INDIVIDUAL AUTHOR CONTRIBUTION STATEMENT
All authors collected the data and drafted the original manuscript. C.M.C., K.R.S., and B.A.D. analyzed the data. N.L.M. designed this research. All authors reviewed and edited the manuscript. All authors read and approved the final manuscript.
REFERENCES
Author notes
The views expressed in this article are those of the authors and do not reflect the official policy or position of the U.S. Government, the DoD, or the Department of the Army.
- respiration
- code
- craniocerebral trauma
- hypothermia, natural
- hypothermia, induced
- needles
- patient simulation
- tourniquets
- wounds and injuries
- breast
- gender
- stress
- chest
- massive hemorrhage
- airway device
- airway structure
- airway procedure
- airway trauma
- simulators
- soldiers
- noncommunicable diseases
- combat medics



