-
PDF
- Split View
-
Views
-
Cite
Cite
Michael F Loncharich, David F Desena, Angelique N Collamer, Jess D Edison, Comparing Rheumatology Consultation Patterns Across Telehealth Platforms and Face-to-Face Clinic in the Military Health System, Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e1456–e1461, https://doi.org/10.1093/milmed/usab531
Close - Share Icon Share
ABSTRACT
To compare patterns of rheumatology consultations and outcomes across four different platforms in the Military Health System (MHS): face-to-face, synchronous telehealth, and two asynchronous telehealth platforms.
We conducted a retrospective review comparing face-to-face rheumatology consults during 2019 with teleconsultations from three virtual systems in the MHS: an asynchronous email-based system from May 2006 to Feb 2018, a web-based platform from 2014 to 2018, and synchronous telehealth consults from March 2020 to March 2021. Consults were reviewed for diagnosis, and if medical evacuation was required for consults originating OCONUS or if face-to-face follow-up was required for synchronous teleconsults. Diagnoses of interest included inflammatory arthritis, noninflammatory arthritis, crystalline arthritis, myositis, lupus, vasculitis, fibromyalgia, antibody positivity without diagnosis, symptoms without specified diagnosis, and a composite of other rheumatic diseases.
Leading diagnoses across platforms were inflammatory arthritis, noninflammatory arthritis, and a composite of other diagnoses. Consultation modality influenced the type of cases seen. Inflammatory arthritis accounted for significantly more consults in the synchronous telehealth (38.4%) and email-based (40.9%) models than in the web-based (23.7%) and face-to-face (32.0%) models. The composite of other diagnoses was the leading diagnosis for the asynchronous web-based model (32.9%), which was significantly more than the synchronous telehealth and face-to-face consults. Synchronous models saw significantly more cases of crystalline arthritis, vasculitis, and fibromyalgia.
Email-based consultations resulted in medical evacuation in 25 cases and prevented evacuation in 5. Web-based consultations prompted medical evacuation in 100 cases. In the synchronous model, face-to-face follow-up was recommended in 142 (15%) cases.
Modality of consultation influences the type of cases seen. Both synchronous and asynchronous telerheumatology models were able to answer the consult question without referral for face-to-face evaluation in 79.9-85.0% of consults, suggesting teleconsultation is a viable method to increase access to high-quality rheumatology care.
INTRODUCTION
Rheumatic diseases are often diagnostically challenging not only due to rarity, but also because symptoms can develop in a nonlinear fashion before the diagnosis is clear. Practice in the Military Health System (MHS) can add additional challenges including more frequent transitions of care and practice in austere environments during military deployments.
Transitions of care are not uncommon in the military; up to 23% of patients in the MHS undergo at least five household relocations to new duty stations and up to 35% experience six or more transitions of care when also accounting for clinician turnover.1 Discontinuity of care within the MHS has been associated with reduced access to specialty care and reduced patient satisfaction,2 which has been shown to correlate with quality of care.3 Telehealth has been utilized in the MHS since 1988 to increase access to care, particularly to those stationed in remote environments.
Restricted access to care is not limited to the MHS. Focusing on rheumatology, by 2025 there will be 0.5-1.0 rheumatologists per 100,000 people resulting in an estimated shortage of 3,269 rheumatologists by 2025 and increasing to a shortage of 4,133 by 2030.4 In the military, there are currently 14 Army rheumatologists and 11 Air Force rheumatologists with 3 Navy rheumatologists practicing in internist billets and 4 civilian rheumatologists resulting in 0.29 rheumatologists per 100,000 MHS beneficiaries5,6; however, access to care is increased by deferring beneficiaries to the civilian network. Projections based on training slots for new fellows and active duty service obligations predict this to drop to 22 rheumatologists in the MHS, or 0.22 per 100,000 beneficiaries by 2025.5,6 A physician shortage during a time of increasing demand is a pattern commonly seen among other subspecialties and primary care, especially in rural areas.7,8
Primary care physicians have reported hesitancy to treat rheumatic disease without rheumatologist oversight. A survey of physician medical directors revealed that community health center physicians would not initiate medications to treat rheumatoid arthritis (RA) or systemic lupus erythematosus (SLE), and only half would refill RA or SLE medications.9 This is particularly problematic for rheumatology patients when 19 million U.S. citizens would need to travel more than 50 miles for their nearest rheumatologist, and nearly 2.5 million would need to travel more than 100 miles.10 Catchment areas within the MHS are typically defined by a 40-mile radius.
The coronavirus disease 2019 (COVID-19) pandemic prompted an unprecedented expansion of telehealth utilization. In response, the American College of Rheumatology released a position statement advocating to broaden telehealth utilization to increase access to care. Further, they proposed continued use of telehealth to mitigate the Rheumatology workforce shortage into the post-pandemic phase.11 The Defense Health Agency (DHA), which oversees the MHS, approved several additional telehealth (TH) delivery methods. In addition to using Adobe Connect for TH video services, the following systems were also approved: Cisco Connect, Apple FaceTime, Google Duo, and Microsoft Skype.12 The DHA also approved audio only telemedicine, which has allowed those with no internet connection and less tech-savvy patients to access TH services.13
Multiple telehealth modalities have been implemented to mitigate these challenges. Here, we review telerheumatology consults from pre-pandemic asynchronous models, a current synchronous model used during the pandemic, and pre-pandemic face-to-face consultations to quantitatively compare consult patterns and how often teleconsultations can be managed entirely remotely across telehealth modalities.
METHODS
We conducted a retrospective review of the primary diagnoses made from rheumatology telehealth consults from three systems: 159 consults from an asynchronous email-based system from May 2006 to Feb 2018, 498 consults from a web-based platform from 2014 to 2018, and 1,118 synchronous telehealth consults in one academic medical center from March 2020 to March 2021. These were compared to 4,419 face-to-face rheumatology consults in 2019. Both initial consultations and follow-up consultations were included in all models. Additionally, we recorded if the consult was managed entirely via telehealth or required either face-to-face follow-up in the synchronous telehealth model or medical evacuation from asynchronous consults OCONUS.
The asynchronous email-based platform was based on the Army Knowledge Online email system. All branches of the military utilized this teleconsultation model in the treatment of active duty service members, affiliated contractors, noncombatants, and detainees. This system was primarily utilized by forward deployed physicians who emailed an on-call rheumatologist at a military hospital in the continental United States. The consulting rheumatologist did not directly interact with the patient. Standard response from time of consultation to reply was within 24 hours.
The web-based platform studied was the Pacific Asynchronous Telehealth and the Health Experts onLine Portal (PATH/HELP) system. This model requires internet connection to access a secure website with a unique username and log in. The PATH/HELP model covers active duty service members, veterans, and their dependents in the Western Pacific, Pacific Northwest, U.S. Eastern Seaboard, and Europe. Similar to the email-based model, the consulting rheumatologist is based at a military tertiary care center and does not have direct patient interaction. Median response time in the period studied is 11.5 hours.
The synchronous telerheumatology platform studied was the telerheumatology service at Walter Reed National Military Medical Center (WRNMMC), which receives consults from the national capital area. The synchronous face-to-face model was the in-person rheumatology consult service at WRNMMC. Data from both of these models excluded inpatient consults.
Across all platforms, data were collected by reviewing the primary diagnostic codes for the encounter. Diagnoses were entered into one of the following categories: inflammatory arthritis, noninflammatory arthritis, crystalline arthritis, myositis, lupus, vasculitis, fibromyalgia, antibody positivity without diagnosis, symptoms without specified diagnosis, and a composite of other rheumatic diseases. This composite was created due to data tracking constraints and rarity of some diseases. Diagnoses in the composite included, but was not limited to, hypermobility, uveitis, unspecified overlap syndromes, rhabdomyolysis, and antisynthetase syndrome. For statistical analysis, we also included a category to account for patient encounters in which a diagnosis was not found.
Statistical analysis with chi-square test and post-hoc analysis with Bonferroni correction was performed to assess if the proportion of each diagnosis significantly differed across the platforms studied.
The authors’ local Institutional Review Board reviewed and approved this study, and informed consent was deemed not required for this retrospective analysis: WRNMMC-EDO-2020-0633.
RESULTS
Outcomes
In the asynchronous, email-based telehealth platform, 25 cases resulted in medical evacuation and 129 (81.1%) were treated locally after teleconsultation followed by return to duty. In the remaining five cases, medical evacuation from the deployed or austere setting was prevented based on teleconsultation. In the asynchronous web platform, 100 cases resulted in medical evacuation and 398 (79.9%) were managed solely via telehealth. In the synchronous telehealth model, 950 cases (85.0%) were managed solely via telehealth, whereas 168 cases (15.0%) were referred for face-to-face follow-up (Fig. 1).
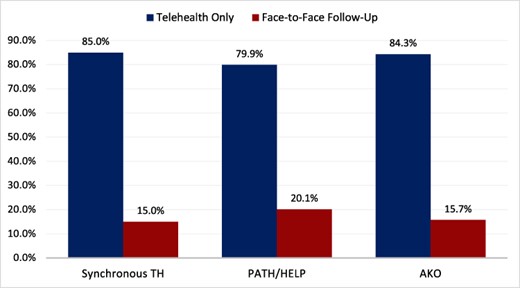
Teleconsultation follow-up.Percent of consults from each telehealth modality that required face-to-face follow-up versus those managed solely via telemedicine.Abbreviations: AKO—Army Knowledge Online, PATH/HELP—Pacific Asynchronous Telehealth and the Health Experts onLine Portal, TH—telehealth.
Diagnoses
Chi-square analysis was performed to determine if the proportion of diagnoses studied varied across consultation platforms. A significant difference in distribution of diagnoses across platforms was found: χ2(30) = 564.02, P < .001, Φ = 0.302. Table I lists diagnoses seen in each consultation modality. Supplementary Table S1 lists the full results of chi-square analysis and post hoc testing.
| Diagnosis . | Face-to-face count (percent) . | Synchronous TH count (percent) . | PATH/HELP count (percent) . | AKO count (percent) . |
|---|---|---|---|---|
| Inflammatory arthritis | 1416 (32.0) | 429 (38.4) | 118 (23.7) | 65 (40.9) |
| Noninflammatory arthritis | 997 (22.6) | 137 (12.3) | 118 (23.7) | 24 (15.1) |
| Myositis | 141 (3.2) | 11 (1.0) | 0 (0) | 1 (0.6) |
| Other diagnosis | 638 (14.4) | 153 (13.7) | 164 (32.9) | 44 (27.7) |
| Lupus | 240 (5.4) | 96 (8.6) | 31 (6.2) | 7 (4.4) |
| Crystalline arthritis | 319 (7.2) | 68 (6.1) | 0 (0) | 0 (0) |
| Vasculitis | 102 (2.3) | 34 (3.0) | 0 (0) | 0 (0) |
| Antibody positivity | 121 (2.7) | 61 (5.5) | 11 (2.2) | 14 (8.8) |
| Fibromyalgia | 295 (6.7) | 65 (5.8) | 0 (0) | 0 (0) |
| Symptoms, no diagnosis | 83 (1.9) | 44 (3.9) | 5 (1.0) | 4 (2.5) |
| Not listed | 67 (1.5) | 20 (1.8) | 51 (10.2) | 0 (0) |
| Diagnosis . | Face-to-face count (percent) . | Synchronous TH count (percent) . | PATH/HELP count (percent) . | AKO count (percent) . |
|---|---|---|---|---|
| Inflammatory arthritis | 1416 (32.0) | 429 (38.4) | 118 (23.7) | 65 (40.9) |
| Noninflammatory arthritis | 997 (22.6) | 137 (12.3) | 118 (23.7) | 24 (15.1) |
| Myositis | 141 (3.2) | 11 (1.0) | 0 (0) | 1 (0.6) |
| Other diagnosis | 638 (14.4) | 153 (13.7) | 164 (32.9) | 44 (27.7) |
| Lupus | 240 (5.4) | 96 (8.6) | 31 (6.2) | 7 (4.4) |
| Crystalline arthritis | 319 (7.2) | 68 (6.1) | 0 (0) | 0 (0) |
| Vasculitis | 102 (2.3) | 34 (3.0) | 0 (0) | 0 (0) |
| Antibody positivity | 121 (2.7) | 61 (5.5) | 11 (2.2) | 14 (8.8) |
| Fibromyalgia | 295 (6.7) | 65 (5.8) | 0 (0) | 0 (0) |
| Symptoms, no diagnosis | 83 (1.9) | 44 (3.9) | 5 (1.0) | 4 (2.5) |
| Not listed | 67 (1.5) | 20 (1.8) | 51 (10.2) | 0 (0) |
Raw count and percentage of each diagnosis for each of the consultation platforms in this study.
Abbreviations: AKO—Army Knowledge Online, PATH/HELP—Pacific Asynchronous Telehealth and the Health Experts onLine Portal, TH—telehealth.
| Diagnosis . | Face-to-face count (percent) . | Synchronous TH count (percent) . | PATH/HELP count (percent) . | AKO count (percent) . |
|---|---|---|---|---|
| Inflammatory arthritis | 1416 (32.0) | 429 (38.4) | 118 (23.7) | 65 (40.9) |
| Noninflammatory arthritis | 997 (22.6) | 137 (12.3) | 118 (23.7) | 24 (15.1) |
| Myositis | 141 (3.2) | 11 (1.0) | 0 (0) | 1 (0.6) |
| Other diagnosis | 638 (14.4) | 153 (13.7) | 164 (32.9) | 44 (27.7) |
| Lupus | 240 (5.4) | 96 (8.6) | 31 (6.2) | 7 (4.4) |
| Crystalline arthritis | 319 (7.2) | 68 (6.1) | 0 (0) | 0 (0) |
| Vasculitis | 102 (2.3) | 34 (3.0) | 0 (0) | 0 (0) |
| Antibody positivity | 121 (2.7) | 61 (5.5) | 11 (2.2) | 14 (8.8) |
| Fibromyalgia | 295 (6.7) | 65 (5.8) | 0 (0) | 0 (0) |
| Symptoms, no diagnosis | 83 (1.9) | 44 (3.9) | 5 (1.0) | 4 (2.5) |
| Not listed | 67 (1.5) | 20 (1.8) | 51 (10.2) | 0 (0) |
| Diagnosis . | Face-to-face count (percent) . | Synchronous TH count (percent) . | PATH/HELP count (percent) . | AKO count (percent) . |
|---|---|---|---|---|
| Inflammatory arthritis | 1416 (32.0) | 429 (38.4) | 118 (23.7) | 65 (40.9) |
| Noninflammatory arthritis | 997 (22.6) | 137 (12.3) | 118 (23.7) | 24 (15.1) |
| Myositis | 141 (3.2) | 11 (1.0) | 0 (0) | 1 (0.6) |
| Other diagnosis | 638 (14.4) | 153 (13.7) | 164 (32.9) | 44 (27.7) |
| Lupus | 240 (5.4) | 96 (8.6) | 31 (6.2) | 7 (4.4) |
| Crystalline arthritis | 319 (7.2) | 68 (6.1) | 0 (0) | 0 (0) |
| Vasculitis | 102 (2.3) | 34 (3.0) | 0 (0) | 0 (0) |
| Antibody positivity | 121 (2.7) | 61 (5.5) | 11 (2.2) | 14 (8.8) |
| Fibromyalgia | 295 (6.7) | 65 (5.8) | 0 (0) | 0 (0) |
| Symptoms, no diagnosis | 83 (1.9) | 44 (3.9) | 5 (1.0) | 4 (2.5) |
| Not listed | 67 (1.5) | 20 (1.8) | 51 (10.2) | 0 (0) |
Raw count and percentage of each diagnosis for each of the consultation platforms in this study.
Abbreviations: AKO—Army Knowledge Online, PATH/HELP—Pacific Asynchronous Telehealth and the Health Experts onLine Portal, TH—telehealth.
Inflammatory arthritis, noninflammatory arthritis, and the composite of other diagnoses were the leading diagnoses across telehealth platforms (Fig. 2). Inflammatory arthritis accounted for 40.9% of consults in the email-based model, 38.4% in the synchronous telehealth model, 32.0% of face-to-face consults, and 23.7% of consults in the web-platform model. Post hoc testing showed that this was proportionately lowest in the web-platform teleconsultation model (P < .001) and significantly higher in the synchronous telehealth model compared to the face-to-face model (P < .001).
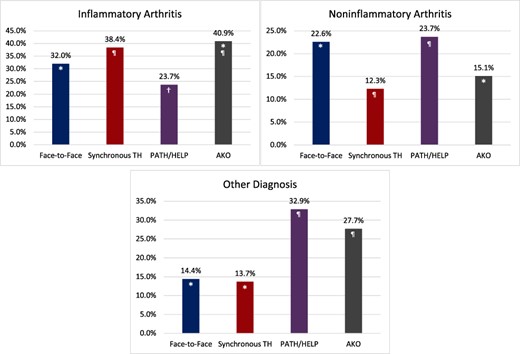
Leading diagnoses across platforms.Leading diagnoses across consultation platforms. Chi-square testing analyzed if each diagnosis differed across consultation platforms. Matching symbols indicate no statistically significant difference of a diagnosis across platforms, and differing symbols indicate statistically significant differences.Abbreviations: AKO—Army Knowledge Online, PATH/HELP—Pacific Asynchronous Telehealth and the Health Experts onLine Portal, TH—telehealth.
Noninflammatory arthritis accounted for 23.7% of consults in the web-platform model, 22.6% of face-to-face consults, 15.1% of email-based consults, and 12.3% of synchronous telehealth consults. Post hoc testing showed proportionately fewer teleconsults for noninflammatory arthritis in the synchronous telehealth model than in the face-to-face or web-based model (P < .001).
Comparing synchronous and asynchronous platforms (Fig. 3), the composite of other diagnoses was proportionately higher in the asynchronous models accounting for 32.9% of web-platform consults, 27.7% of email-based consults, 14.4% of face-to-face consults, and 13.7% of synchronous telehealth consults. In contrast, the asynchronous telerheumatology platforms received proportionately fewer consults for crystalline arthritis, fibromyalgia, or vasculitis, whereas these diagnoses accounted for 6.1%, 5.8%, and 3.0% of consults in the synchronous telehealth model and 7.2%, 6.7%, and 2.3% of consults in the face-to-face model, respectively.
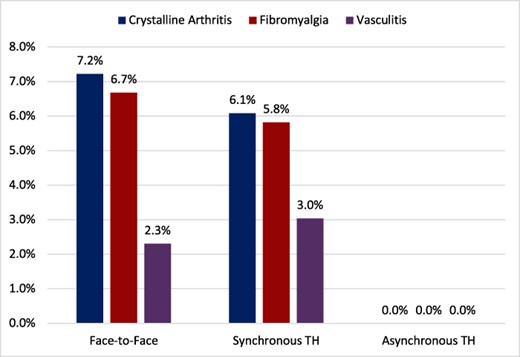
Comparison of synchronous versus asynchronous consultations.There were significantly more consults for crystalline arthritis, fibromyalgia, and vasculitis in the synchronous consultation platforms and no consults for these on AKO or PATH/HELP.Abbreviations: AKO—Army Knowledge Online, PATH/HELP—Pacific Asynchronous Telehealth and the Health Experts onLine Portal, TH—telehealth.
The distribution of other investigated diagnoses is detailed in Table I and shown graphically in Figure 1.
DISCUSSION
Referral patterns were similar across telehealth modalities, but there were some differences. In the asynchronous models, there were more referrals for the composite of other diagnoses and fewer referrals for crystalline arthropathies and fibromyalgia, suggesting a qualitative difference in referral patterns in different telehealth mediums.
We suspect a large part of this difference is due to divergent utilizations. The asynchronous modalities reviewed here are primarily used by physicians OCONUS within the MHS, which selects for a healthier patient population (mainly deployed military service members). In comparison, the synchronous model primarily receives consultations in a tertiary care center in a major metropolitan area with a patient population consisting of active duty military, their families, and retired service members and their beneficiaries. Additionally, lack of direct patient contact in the asynchronous models likely influences both cases that are referred and the consultant’s diagnosis.
Rates of face-to-face follow-up required were comparable across modalities, and a large majority of cases were successfully managed solely with telehealth. Currently, rheumatology consults account for 0.6% of tele-consults in the MHS.14 A recent review of telehealth in a tertiary military medical center in Europe has shown the potential to capture thousands of additional encounters that would have otherwise required transfer or purchased care resulting in an estimated savings of $1.3 million in 2017 alone.15 Cost savings from teleconsultations are not unique to military healthcare. A review of telerheumatology including 20 studies found that while only 6 reported on cost-efficacy, all 6 showed telerheumatology to be cost-effective.16 However, the authors note the rigor of cost-analysis was lacking in these studies.
Resource availability and disparate user interfaces likely contribute to the differences observed in this study. The asynchronous models require access to email or a potentially cumbersome encrypted web-based platform in environments potentially as austere as a field hospital. Commonly cited reasons for physician reluctance to broader adoption of telehealth include platform complexity,17 unfamiliarity with new methods,18 and challenging user interface.19
Our study has several limitations. Due to data tracking constraints and rarity of some diseases, some diagnoses were clustered into the composite of other diagnoses rather than listed individually. The older, asynchronous telehealth platforms collated diagnoses in broad groups, whereas individual diagnostic codes were available from the synchronous platforms. For consistency across platforms, we used the same diagnostic categories in all models. Similarly, some diagnostic codes were missing from each investigated consultation modality. The date range investigated from each platform varied, which adds the confounding factor of the influence of the COVID-19 pandemic. Finally, this study was based on the use of primary diagnostic codes, and potentially relevant secondary diagnostic codes were excluded.
As demonstrated by the majority of teleconsults not requiring face-to-face follow-up across all platforms, telehealth appears to be a viable option to increase access to care for rheumatology patients across a variety of consultation platforms. Concordant with the ACR telemedicine position statement, use and acceptance of telerheumatology are increasing. Defining appropriate patients, follow-up intervals, and modality of telehealth platforms are important topics for further study. Clear description of liability responsibilities and reimbursement patterns with demonstrable ease-of-use will be necessary to minimize rheumatologist resistance to adopt telehealth as an enduring solution to mitigate the growing workforce shortage.
ACKNOWLEDGMENTS
The authors would like to thank LTC Charlie T Nguyen and Ms. Anna Castillo-Lora for their aid in securing data from the PATH/HELP teleconsultation platform and LTC Autumn Richards for her help securing NCC teleconsultation data.
SUPPLEMENTARY MATERIAL
SUPPLEMENTARY MATERIAL is available at Military Medicine online.
FUNDING
None declared.
CONFLICT OF INTEREST STATEMENT
The authors report no conflict of interest including consulting fees, paid expert testimony, employment, grants, honoraria, patents, royalties, stocks, or any other relationships or ethical considerations that may involve the subject matter of the manuscript and compromise its integrity. No financial support or other benefits from commercial sources were obtained for work involving this manuscript.
REFERENCES
Author notes
High Value Practice Academic Alliance, poster, virtual conference, 10/9/21. American College of Rheumatology national meeting, poster, virtual conference, 11/6/21.
The views expressed in this manuscript are those of the authors and do not reflect the official policy of the Department of Army/Navy/Air Force/Space Force, Department of Defense, or U.S. Government.



