-
PDF
- Split View
-
Views
-
Cite
Cite
F Chierigo, G Mantica, M Oszczudlowski, F X Madec, L Bialek, E J Redmond, M Waterloos, W Verla, C M Rosenbaum, M A Frankiewicz, A Cocci, J Klemm, P Neuville, J Adamowicz, F Campos-Juanatey, D Ralph, M W Vetterlein, CURRENT PRACTICES AND TREATMENT STRATEGIES FOR CLIMACTURIA: A YAU RECONSTRUCTIVE AND ESGURS SURVEY, The Journal of Sexual Medicine, Volume 22, Issue Supplement_2, May 2025, qdaf077.117, https://doi.org/10.1093/jsxmed/qdaf077.117
Close - Share Icon Share
Abstract
Climacturia is a neglected complication following radical prostatectomy (RP) that significantly impacts quality of life. Despite its prevalence, treatment approaches remain underreported. This survey evaluates European practices in managing climacturia.
A Google Form-based survey was circulated among andrology, reconstructive, and functional urology experts by the YAU Reconstructive Working Party and ESGURS. Descriptive statistics were used for analysis.
Of 59 respondents (91.5% from teaching hospitals), 75% managed male incontinence surgeries, and 68% performed penile implants. While all respondents assessed stress urinary incontinence (SUI) and erectile dysfunction (ED) after RP, only 60% routinely inquired about climacturia. The reported median (IQR) prevalence of climacturia at 3 months post-RP was 15% (5-30%) and 10% (4-15%) at 12 months.
In the absence of a standardized assessment tool, we proposed a new one focusing on urine loss volume, frequency, and patient bother, with a median (IQR) approval score of 7 (7-8) on a Likert scale.
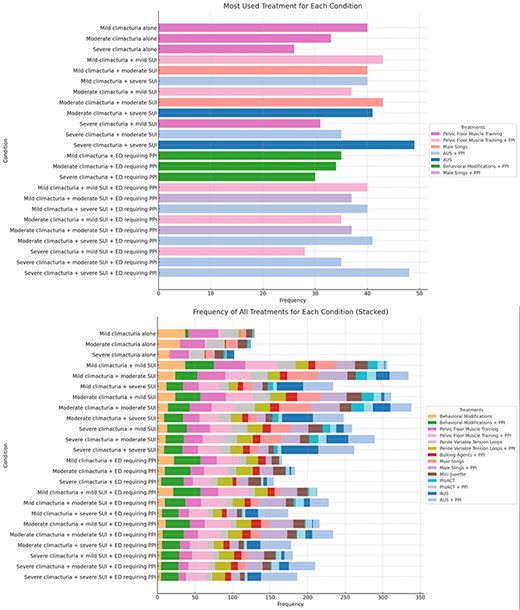
Key treatment strategies for climacturia included:
Behavioral Modifications: Commonly recommended for mild cases, focusing on lifestyle adjustments and timed voiding.
Pelvic Floor Muscle Training (PFMT): Widely used for mild-to-moderate climacturia, often with SUI or ED management.
Mini-Jupette: Suggested for moderate cases, particularly when SUI is present, providing additional urethral support during sexual activity.
Male Slings: Frequently applied for moderate climacturia with SUI, improving continence.
Artificial Urinary Sphincter (AUS): Reserved for severe climacturia or complex cases, especially with significant SUI, offering definitive control.
Combination Approaches: For climacturia with ED, combinations such as AUS with PPI were commonly used.
Treatment followed a stepwise approach, with conservative options for mild symptoms and invasive interventions for severe cases.
This survey highlights the need for standardized assessment tools and offers insights into current practices. Conservative treatments are favored for mild climacturia, while AUS is prioritized for severe cases. Further research is needed to optimize management strategies and improve outcomes.
none.