-
PDF
- Split View
-
Views
-
Cite
Cite
J Weinberger, K Koontz, T Nguyen, N Kim, S Goldstein, I Goldstein, (030) QUANTITATIVE SENSORY TESTING OF THE CLITORIS, VULVA AND VESTIBULE IN MENOPAUSAL PATIENTS WITH SEXUAL DYSFUNCTION, The Journal of Sexual Medicine, Volume 22, Issue Supplement_1, April 2025, qdaf068.030, https://doi.org/10.1093/jsxmed/qdaf068.030
Close - Share Icon Share
Abstract
Individuals in menopause often complain of sexual dysfunction (low libido, reduced sensation, muted orgasm). In sexual-health related menopause concerns, hormonal pathophysiologies have been well studied, however, the effects of menopause on the integrity of the female genital sensory pathways have not been well researched. Somatic afferent pathways of the clitoris, vulva and vestibule include the dorsal and perineal nerve branches of the pudendal nerve (S2-S4). To assess the integrity of these somatic afferent pathways, genital quantitative sensory testing (QST) may be performed. QST consists of vibration perception threshold testing for large myelinated A-beta fibers and temperature perception threshold testing for small myelinated A-delta fibers (cold) and for unmyelinated c-fibers (warmth).
We wished to assess genital QST in menopausal patients with sexual dysfunction.
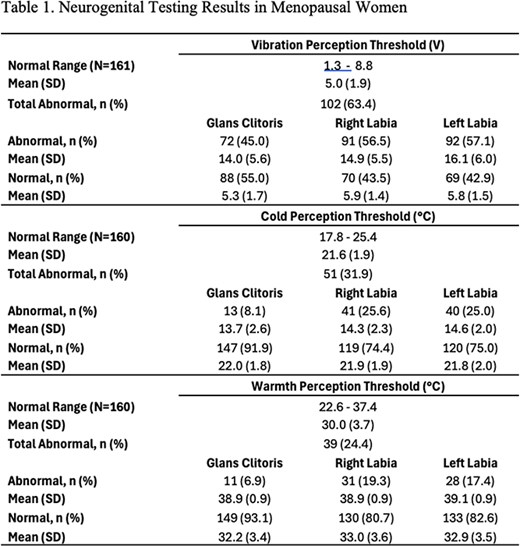
This is a chart review of menopausal patients presenting to a sexual medicine clinic for sexual dysfunction between January 2022 and October 2024. They all presented with limited or no previous menopause management by systemic and/or local sex steroid hormone treatment. Quantitative sensory testing of vibratory, cold and warm sensation was performed at the initial visit, prior to any treatment from our clinic, using a biothesiometer (Bio-Medical Instruments, Newbury, OH) to test for vibration perception threshold (VPT) measured in volts, and a thermal sensitivity tester (Sensortek, Inc., Clifton, NJ) to test for cold perception threshold (CPT) and warmth perception threshold (WPT) measured in degrees Centigrade, comparing the genital readings to a non-genital location as control. The protocol for formal CPT testing begins with exposure to a 25°C probe and requires the patient to relay their perception of a decreasing temperature as soon as she perceives it. Similarly, WPT testing begins at 25°C but the probe increases in temperature until a change in perception is identified. Abnormal QST was defined when the test value was ≥2 standard deviations from the control value.
A total of 30 charts of patients in menopause were reviewed. Sixteen individuals, mean age 59 (range 50 to 81 years), presented for GSM alone. Abnormal VPT testing was found in 63%, mean VPT value 15 V compared to 6 V for control. Abnormal CPT testing was found in 44%, mean CPT value 19°C compared to 22°C for control. Abnormal WPT testing was found in 68%, mean WPT value 35°C compared to 27°C for control. Fourteen individuals, mean age 64 (range 50 to 78 years), presented with concomitant PGAD/GPD. Abnormal VPT testing was found in 71%, mean VPT value 16 V compared to 5 V for control. Abnormal CPT testing was found in 43%, mean CPT value 20°C compared to 22°C for control. Abnormal WPT testing was found in 71%, mean WPT value 35°C compared to 28°C for control.
The prevalence of abnormal neurogenital testing in menopausal women was significant in this cohort, consistent withreports of reduced vulvar sensitivity with menopause in the literature. We conclude that genital sensory impairment is common in menopause, may contribute to menopause-related sexual dysfunction, and should be documented objectively by baseline neurogenital testing.
No.