- Split View
-
Views
-
Cite
Cite
MAM Hammad, B Azad, MS Gross, D Swerdloff, J Miller, E Abou Chawareb, A Alkhayal, KA Alrabeeah, R Andrianne, AL Burnett, K Gross, G Hatzichristodoulou, A Lentz, D Osmonov, A Jones, V Modgil, P Perito, JM Hotaling, SH Park, I Pearce, H Sadeghi-Nejad, M Sempels, A Suarez-Sarmiento Jr., K Van Renterghem, JN Warner, M Ziegelmann, TC Hsieh, L Jenkins, J Jones, J Simhan, FA Yafi, on behalf of the PUMP (Prosthetic Urology Multi-institutional Partnership) collaborators, DW Barham, (149) NEW FINDINGS REGARDING PERIOPERATIVE INFLATABLE PENILE PROSTHESIS ANTIMICROBIAL PROPHYLAXIS PATTERNS FROM A LARGE MULTINATIONAL COLLABORATION, The Journal of Sexual Medicine, Volume 21, Issue Supplement_6, December 2024, qdae161.121, https://doi.org/10.1093/jsxmed/qdae161.121
Close - Share Icon Share
Abstract
Inflatable penile prosthesis (IPP) surgery is a well-established treatment for erectile dysfunction (ED). There is little information in the literature regarding the utilization of perioperative antimicrobial prophylaxis in primary and revision IPP surgeries.
We investigated the patterns of perioperative antimicrobial prophylaxis among a large multinational cohort of primary and revision IPP surgeries.
We conducted a retrospective analysis of 5400 patients (4187 primary IPP patients and 849 revision IPP patients) from our Prosthetic Urology Multi-Institutional Partnership (PUMP) institutions. Usage data for intravenous (IV), preoperative oral, and postoperative oral antimicrobials were analyzed. We specifically assessed patient profiles, antimicrobial selection, and antimicrobial duration. Multivariate statistical analyses were conducted to identify significant variations between primary and revision surgeries.
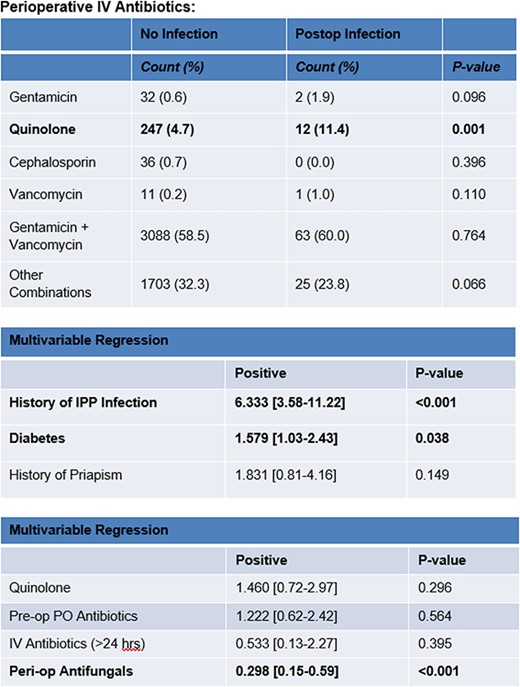
For patients undergoing primary IPP placement, 81.9% received IV antibiotics for <24 hours whereas 18.1% received IV antibiotics for >24 hours. Preoperative oral antimicrobials were used in 59.4% of patients and 99.4% received postoperative oral antimicrobials. The overall infection rate for primary implants was 2%. Notably, quinolone administration shows a higher postoperative infection rate (11.4%) compared to gentamicin (1.9%), cephalosporin (0%), and vancomycin (1.0%). Multivariable regression analysis identifies factors such as a history of infection, diabetes, and priapism as predictors for postoperative infections. Furthermore, the study finds that perioperative antifungal use is associated with a decreased risk of infection.
This study provides valuable insights into the patterns of perioperative antimicrobial prophylaxis. Duration, type, and route of antibiotics given preoperatively or postoperatively do not affect postoperative infection rates among high volume prosthetic urologists. Giving IV antibiotics for more than 24 hours does not affect postoperative infection. Perioperative antifungals are a protective factor.
Any of the authors act as a consultant, employee or shareholder of an industry for: Coloplast, Clarus Therapeutics, Antares Pharma, Acerus.