-
PDF
- Split View
-
Views
-
Cite
Cite
Ibrahim Jubber, Zoe Rogers, James WF Catto, Sarah Bottomley, Adam Glaser, Amy Downing, Kate Absolom, Sexual Activity, Function and Dysfunction After a Diagnosis of Bladder Cancer, The Journal of Sexual Medicine, Volume 19, Issue 9, September 2022, Pages 1431–1441, https://doi.org/10.1016/j.jsxm.2022.06.016
Close - Share Icon Share
ABSTRACT
Sexual dysfunction is common in those affected by cancer and local and radical treatments for Bladder Cancer (BC) can affect sexual function directly.
To evaluate sexual function following a bladder cancer (BC) diagnosis.
Self-reported sexual function was collected 10 years after a diagnosis of BC as part of a cross-sectional patient reported outcome measure (PROM) survey exploring life after BC diagnosis and treatment.
Participants completed a combined EORTC QLQ-BLM30 and QLQ-NMIBC24 questionnaire, including questions on sexual activity, intimacy, erectile/ejaculatory function and vaginal dryness.
A total of 1796 participants returned a completed survey out of 3279 eligible participants (55%). Of the participants who returned a completed survey, a total of 1530 (85%) participants answered sexual function questions. The median (IQR) age was 75 (70–81). Participants were predominantly men (78%) and married/in civil partnerships (66%). In total, 31% were sexually active. Vaginal dryness was common (66%) in women. Erectile and ejaculatory dysfunction (80% and 58% respectively) were common in men. Compared to TURBT +/- intravesical treatments, those who had radical treatment were less likely to be sexually active (adjusted OR 0.56, 95% CI: 0.44–0.72, P<0.001) and had worse mean scores for intimacy problems (29.1 [radical treatment] vs 12.1, P<0.001), male sexual problems (72.2 [radical treatment] vs 45.7, P<0.001) and overall sexual function (17.1 [radical treatment] vs 20.3, P=0.01).
These findings highlight the magnitude of sexual dysfunction in the BC patient cohort and can help inform patients during the pre-op counselling process and shared decision making prior to BC treatments.
This study provides the largest in-depth analysis of sexual activity and function after BC diagnosis and treatment, to date. Limitations include the lack of data on participants’ sexual function prior to BC treatment and the heterogeneity with respect to time passed since last BC treatment.
Sexual dysfunction in BC patients is common and rates appear higher following radical treatments compared to endoscopic. It is important to elicit these problems in clinics to enable counselling and treatment.
INTRODUCTION
Sexual dysfunction in those affected by cancer is common and may arise from anatomical disruption, side-effects from medication, emotional consequences of the diagnosis and treatment, or a combination of these.1,2 Bladder cancer (BC) is the ninth most commonest and one of the most prevalent cancers worldwide.3 Treatments vary between local bladder-sparing approaches and radical cystectomy (RC) or radiotherapy (RT). Local and radical treatments may affect sexual function directly. Endoscopic resection uses electrocautery that may temporarily disrupt erectile function and libido.4 Intravesical treatments (such as Bacillus Calmette-Guerin [BCG] and chemotherapy) may cause infections or local inflammation leading to painful ejaculation, erectile difficulties and concern about contamination.5,6 Both RC and RT lead to erectile and ejaculation dysfunction in men, and vaginal dryness, vaginal shortening and dyspareunia in women.7 Cystectomy often requires an ileal conduit diversion and this may impact upon body image.8 These predictable changes may be discussed too briefly at the time of consent, leading to distress.9
We recently published a large cross-sectional survey of health-related quality of life (HRQOL) in participants 1–10 years after a diagnosis of BC.10 HRQOL was found to be significantly worse than for colorectal or prostate cancer patients. With regards to sexual problems, we found these were more commonly reported by younger men and those who received radical treatment. To date, most reports of sexual function in BC have been modest in size, focussed on either NMI or invasive disease, or have compared surgical approaches (e.g. ileal conduit vs neobladder).11 Whilst small reports have identified areas of potential concern, there is an urgent need to comprehensively understand the sexual consequences of BC diagnosis and treatment, thereby helping in the counselling of individuals and development of therapeutic strategies.12 Here we evaluate and explore in detail, the sexual function components from our previously published survey.10
METHODS
Study Design and Setting
Sexual function information was collected as part of a cross-sectional patient reported outcome measure (PROM) survey exploring life after BC diagnosis and treatment. The full methods and wider results are published elsewhere.10,13 In brief, eligible participants aged ≥18 years, between 1–10 years after a diagnosis of BC (NMI or invasive) between January 2007 and December 2016 and diagnosed in the National Health Service (NHS) hospitals in Yorkshire and Humber, North Derbyshire or South Tees regions were invited to participate. Participants could either complete a paper questionnaire that was mailed to their home address, complete an online questionnaire, or complete the questionnaire over the telephone.
Questionnaire Content
With the appropriate permissions from the EORTC, components of the EORTC QLQ-BLM30 and QLQ-NMIBC24 questionnaires were combined to assess treatment and cancer-specific HRQOL.
The combined EORTC QLQ-BLM30 and QLQ-NMIBC24 questionnaires included the following sexual function scales/items answered on a 4-point scale (‘not at all’ to ‘very much’) with reference to the last 4 weeks
- -
Sexual function (2 items, covering sexual activity [“To what extent were you sexually active?”] and interest [“To what extent were you interested in sex?”])
- -
Male sexual problems (2 items, covering erectile [“Did you have difficulty in gaining or maintaining an erection?”] and ejaculation issues [“Did you have ejaculation problems?”])
- -
If sexually active in the last 4 weeks:
- -
Female sexual problems (1 item, on vaginal dryness [“Did you have a dry vagina or other problems during intercourse?”])
- -
Sexual intimacy (1 item, about comfort with sexual intimacy [“Have you felt uncomfortable about being sexually intimate?”])
- -
Risk of contaminating partner (1 item, worry about treatment contamination [“Have you worried that you may contaminate your partner during sexual contact with the bladder treatment you have been receiving?”])
- -
Sexual enjoyment (1 item [“To what extent was sex enjoyable for you?”]).
Higher scores reflect better function for the sexual function and sexual enjoyment domains. In contrast, higher scores for the following domains: male sexual problems, female sexual problems, sexual intimacy and risk of contaminating partner, reflect worsening function. The survey captured self-reported information on participant socio-demographics, level of physical activity (GODIN scale),14 treatment received for BC (TURBT +/- intravesical treatments, RC or RT) and the presence of long term conditions (LTCs). The LTCs captured were heart conditions, angina, stroke, hypertension, diabetes, arthritis, asthma/chronic chest problems, gastrointestinal problems (stomach, bowel or gall bladder problems), kidney diseases, Alzheimer’s/Dementia, Epilepsy, Neurological problems and liver or pancreas problems. The income domain of the Index of Multiple Deprivation (IMD) was used to measure socioeconomic deprivation. The IMD was allocated using postcode of residence at diagnosis and grouped into quintiles, with IMD category 1 being the most socially deprived.15
Statistical Analysis
Age was grouped into <65, 65–74, 75–84, and ≥85 years. The number of LTCs were grouped into none, one, two, three or ≥4. In addition, we looked at sexual activity in patients with specific LTCs.
EORTC Questionnaire responses were linearly transformed to a 0-100 scale as previously described.16 Mean (and standard deviation [SD]) scores were calculated for: sexual function, male sexual problems, sexual intimacy problems, risk of contaminating partner worry, sexual enjoyment and female sexual problems. For the purposes of analysis, treatment group was separated into two groups. TURBT was grouped together with adjuvant intravesical treatments and RC and radical RT were grouped together as radical treatment due to the small number of patients undergoing RT. Categorical outcomes were analysed using a chi-square test and continuous variables were analysed using a T test for parametric data and a Mann-Whitney U test for non-parametric data. Logistic regression was used to assess the relationship between sexual activity and treatment group controlling for confounding variables. With regards to missing data and individual questions in the survey that weren’t answered, data was analysed if there were still questions answered that were stand-alone and not dependent on others. However, we did not include answers to sexual questions where there was a dependency on being sexually active in the last 4 weeks. For these questions participants were instructed to answer only if sexually active in the last 4 weeks. Where participants had not followed the instructions and reported not being sexually active in the last 4 weeks, and still answered the questions that depended on being sexually active, their answers were excluded from the analysis. Statistical Analysis was performed using STATA (Version 16.1 for Windows).
RESULTS
Participants
As previously reported,10 1,796 of 3,279 eligible participants returned a completed survey (55%). Of these, 1,530 (85% of those who returned a completed survey) answered questions on sexual activity and were used as the denominator in this sub-study. In total, 1492 participants completed paper questionnaires, 29 participants completed online questionnaires and 9 participants completed telephone questionnaires.
Most participants were men (78%), married or in a civil partnership (66%), insufficiently active using the GODIN exercise scale (53%) and were current (9%) or ex-smokers (60%) (Table 1). A further breakdown of demographics stratified by sex and individual treatments are in supplementary tables 1 and 2 respectively.
| . | All treatments . | TURBT+/- MMC/BCG . | Radical Cystectomy or Radical RT +/- other . | P value . | |||
|---|---|---|---|---|---|---|---|
| . | (N=1,530) . | (N=731)a . | (N=737)a . | ||||
| Characteristic . | No. or Median . | % or IQR . | No. or Median . | % or IQR . | No. or Median . | % or IQR . | |
| Sex | |||||||
| Male | 1,199 | 78 | 597 | 52 | 558 | 48 | |
| Female | 331 | 22 | 134 | 43 | 179 | 57 | 0.005 |
| Age at diagnosis, years | 69 | 63–75 | 69.0 | 63–76 | 69 | 63–75 | 0.19 |
| Age at survey, years | 75 | 70–81 | 76.0 | 70–82 | 75 | 70–80 | 0.003 |
| No. of other LTCs | |||||||
| None | 364 | 24 | 163 | 47 | 187 | 53 | |
| 1 | 466 | 30 | 222 | 50 | 226 | 50 | |
| 2 | 320 | 21 | 145 | 48 | 159 | 52 | |
| 3 | 205 | 13 | 106 | 53 | 95 | 47 | |
| ≥4 | 175 | 11 | 95 | 58 | 70 | 42 | 0.15 |
| IMD | |||||||
| 1 (least deprived) | 345 | 23 | 169 | 52 | 157 | 48 | |
| 2 | 388 | 25 | 174 | 47 | 196 | 53 | |
| 3 | 323 | 21 | 155 | 49 | 162 | 51 | |
| 4 | 240 | 16 | 117 | 52 | 109 | 48 | |
| 5 (most deprived) | 234 | 15 | 116 | 51 | 113 | 49 | 0.70 |
| Employment status | |||||||
| Employed | 176 | 12 | 76 | 44 | 97 | 56 | |
| Unemployed | 28 | 2 | 11 | 41 | 16 | 59 | |
| Retired | 1,277 | 83 | 615 | 50 | 605 | 50 | 0.19 |
| Other | 13 | 1 | 7 | 54 | 6 | 46 | |
| Not known | 36 | 2 | 22 | 63 | 13 | 37 | |
| Relationship status | |||||||
| Married/Civil partnership | 1,012 | 66 | 477 | 49 | 503 | 51 | |
| Separated/Divorced | 135 | 9 | 56 | 43 | 75 | 57 | |
| Widowed/Surviving Partner | 255 | 17 | 136 | 57 | 101 | 43 | |
| Single | 51 | 3 | 25 | 53 | 22 | 47 | 0.03 |
| Other | 21 | 1 | 12 | 60 | 8 | 40 | |
| Not known | 56 | 4 | 25 | 47 | 28 | 53 | |
| Smoking | |||||||
| Never smoker | 405 | 26 | 194 | 50 | 194 | 50 | |
| Ex-smoker | 914 | 60 | 438 | 50 | 441 | 50 | |
| Current smoker | 143 | 9 | 72 | 52 | 66 | 48 | 0.88 |
| Not known | 68 | 4 | 27 | 43 | 36 | 57 | |
| GODIN Exercise | |||||||
| Insufficiently active | 809 | 53 | 380 | 49 | 401 | 51 | |
| Moderately active | 109 | 7 | 50 | 48 | 55 | 52 | |
| Active | 242 | 16 | 129 | 55 | 105 | 45 | 0.20 |
| Not known | 370 | 24 | 172 | 49 | 176 | 51 | |
| Carer | |||||||
| No | 1,132 | 74 | 538 | 50 | 547 | 50 | |
| Yes | 297 | 19 | 149 | 52 | 138 | 48 | 0.48 |
| Not known | 101 | 7 | 44 | 46 | 52 | 54 | |
| Ethnicity | |||||||
| White | 1,455 | 95 | 696 | 50 | 700 | 50 | |
| Non white | 16 | 1 | 10 | 63 | 6 | 38 | 0.45 |
| Not known | 59 | 4 | 25 | 45 | 31 | 55 | |
| . | All treatments . | TURBT+/- MMC/BCG . | Radical Cystectomy or Radical RT +/- other . | P value . | |||
|---|---|---|---|---|---|---|---|
| . | (N=1,530) . | (N=731)a . | (N=737)a . | ||||
| Characteristic . | No. or Median . | % or IQR . | No. or Median . | % or IQR . | No. or Median . | % or IQR . | |
| Sex | |||||||
| Male | 1,199 | 78 | 597 | 52 | 558 | 48 | |
| Female | 331 | 22 | 134 | 43 | 179 | 57 | 0.005 |
| Age at diagnosis, years | 69 | 63–75 | 69.0 | 63–76 | 69 | 63–75 | 0.19 |
| Age at survey, years | 75 | 70–81 | 76.0 | 70–82 | 75 | 70–80 | 0.003 |
| No. of other LTCs | |||||||
| None | 364 | 24 | 163 | 47 | 187 | 53 | |
| 1 | 466 | 30 | 222 | 50 | 226 | 50 | |
| 2 | 320 | 21 | 145 | 48 | 159 | 52 | |
| 3 | 205 | 13 | 106 | 53 | 95 | 47 | |
| ≥4 | 175 | 11 | 95 | 58 | 70 | 42 | 0.15 |
| IMD | |||||||
| 1 (least deprived) | 345 | 23 | 169 | 52 | 157 | 48 | |
| 2 | 388 | 25 | 174 | 47 | 196 | 53 | |
| 3 | 323 | 21 | 155 | 49 | 162 | 51 | |
| 4 | 240 | 16 | 117 | 52 | 109 | 48 | |
| 5 (most deprived) | 234 | 15 | 116 | 51 | 113 | 49 | 0.70 |
| Employment status | |||||||
| Employed | 176 | 12 | 76 | 44 | 97 | 56 | |
| Unemployed | 28 | 2 | 11 | 41 | 16 | 59 | |
| Retired | 1,277 | 83 | 615 | 50 | 605 | 50 | 0.19 |
| Other | 13 | 1 | 7 | 54 | 6 | 46 | |
| Not known | 36 | 2 | 22 | 63 | 13 | 37 | |
| Relationship status | |||||||
| Married/Civil partnership | 1,012 | 66 | 477 | 49 | 503 | 51 | |
| Separated/Divorced | 135 | 9 | 56 | 43 | 75 | 57 | |
| Widowed/Surviving Partner | 255 | 17 | 136 | 57 | 101 | 43 | |
| Single | 51 | 3 | 25 | 53 | 22 | 47 | 0.03 |
| Other | 21 | 1 | 12 | 60 | 8 | 40 | |
| Not known | 56 | 4 | 25 | 47 | 28 | 53 | |
| Smoking | |||||||
| Never smoker | 405 | 26 | 194 | 50 | 194 | 50 | |
| Ex-smoker | 914 | 60 | 438 | 50 | 441 | 50 | |
| Current smoker | 143 | 9 | 72 | 52 | 66 | 48 | 0.88 |
| Not known | 68 | 4 | 27 | 43 | 36 | 57 | |
| GODIN Exercise | |||||||
| Insufficiently active | 809 | 53 | 380 | 49 | 401 | 51 | |
| Moderately active | 109 | 7 | 50 | 48 | 55 | 52 | |
| Active | 242 | 16 | 129 | 55 | 105 | 45 | 0.20 |
| Not known | 370 | 24 | 172 | 49 | 176 | 51 | |
| Carer | |||||||
| No | 1,132 | 74 | 538 | 50 | 547 | 50 | |
| Yes | 297 | 19 | 149 | 52 | 138 | 48 | 0.48 |
| Not known | 101 | 7 | 44 | 46 | 52 | 54 | |
| Ethnicity | |||||||
| White | 1,455 | 95 | 696 | 50 | 700 | 50 | |
| Non white | 16 | 1 | 10 | 63 | 6 | 38 | 0.45 |
| Not known | 59 | 4 | 25 | 45 | 31 | 55 | |
BCG = Bacillus Calmette-Guerin; GODIN = Godin Leisure-Time Exercise Questionnaire; IMD=Index of Multiple Deprivation; LTCs= Long Term Conditions; MMC = Intravesical Mitomycin C; TURBT = Transurethral Resection of a Bladder Tumour
N=62 out of N=1530 with Treatment Other/Not known excluded from analysis
| . | All treatments . | TURBT+/- MMC/BCG . | Radical Cystectomy or Radical RT +/- other . | P value . | |||
|---|---|---|---|---|---|---|---|
| . | (N=1,530) . | (N=731)a . | (N=737)a . | ||||
| Characteristic . | No. or Median . | % or IQR . | No. or Median . | % or IQR . | No. or Median . | % or IQR . | |
| Sex | |||||||
| Male | 1,199 | 78 | 597 | 52 | 558 | 48 | |
| Female | 331 | 22 | 134 | 43 | 179 | 57 | 0.005 |
| Age at diagnosis, years | 69 | 63–75 | 69.0 | 63–76 | 69 | 63–75 | 0.19 |
| Age at survey, years | 75 | 70–81 | 76.0 | 70–82 | 75 | 70–80 | 0.003 |
| No. of other LTCs | |||||||
| None | 364 | 24 | 163 | 47 | 187 | 53 | |
| 1 | 466 | 30 | 222 | 50 | 226 | 50 | |
| 2 | 320 | 21 | 145 | 48 | 159 | 52 | |
| 3 | 205 | 13 | 106 | 53 | 95 | 47 | |
| ≥4 | 175 | 11 | 95 | 58 | 70 | 42 | 0.15 |
| IMD | |||||||
| 1 (least deprived) | 345 | 23 | 169 | 52 | 157 | 48 | |
| 2 | 388 | 25 | 174 | 47 | 196 | 53 | |
| 3 | 323 | 21 | 155 | 49 | 162 | 51 | |
| 4 | 240 | 16 | 117 | 52 | 109 | 48 | |
| 5 (most deprived) | 234 | 15 | 116 | 51 | 113 | 49 | 0.70 |
| Employment status | |||||||
| Employed | 176 | 12 | 76 | 44 | 97 | 56 | |
| Unemployed | 28 | 2 | 11 | 41 | 16 | 59 | |
| Retired | 1,277 | 83 | 615 | 50 | 605 | 50 | 0.19 |
| Other | 13 | 1 | 7 | 54 | 6 | 46 | |
| Not known | 36 | 2 | 22 | 63 | 13 | 37 | |
| Relationship status | |||||||
| Married/Civil partnership | 1,012 | 66 | 477 | 49 | 503 | 51 | |
| Separated/Divorced | 135 | 9 | 56 | 43 | 75 | 57 | |
| Widowed/Surviving Partner | 255 | 17 | 136 | 57 | 101 | 43 | |
| Single | 51 | 3 | 25 | 53 | 22 | 47 | 0.03 |
| Other | 21 | 1 | 12 | 60 | 8 | 40 | |
| Not known | 56 | 4 | 25 | 47 | 28 | 53 | |
| Smoking | |||||||
| Never smoker | 405 | 26 | 194 | 50 | 194 | 50 | |
| Ex-smoker | 914 | 60 | 438 | 50 | 441 | 50 | |
| Current smoker | 143 | 9 | 72 | 52 | 66 | 48 | 0.88 |
| Not known | 68 | 4 | 27 | 43 | 36 | 57 | |
| GODIN Exercise | |||||||
| Insufficiently active | 809 | 53 | 380 | 49 | 401 | 51 | |
| Moderately active | 109 | 7 | 50 | 48 | 55 | 52 | |
| Active | 242 | 16 | 129 | 55 | 105 | 45 | 0.20 |
| Not known | 370 | 24 | 172 | 49 | 176 | 51 | |
| Carer | |||||||
| No | 1,132 | 74 | 538 | 50 | 547 | 50 | |
| Yes | 297 | 19 | 149 | 52 | 138 | 48 | 0.48 |
| Not known | 101 | 7 | 44 | 46 | 52 | 54 | |
| Ethnicity | |||||||
| White | 1,455 | 95 | 696 | 50 | 700 | 50 | |
| Non white | 16 | 1 | 10 | 63 | 6 | 38 | 0.45 |
| Not known | 59 | 4 | 25 | 45 | 31 | 55 | |
| . | All treatments . | TURBT+/- MMC/BCG . | Radical Cystectomy or Radical RT +/- other . | P value . | |||
|---|---|---|---|---|---|---|---|
| . | (N=1,530) . | (N=731)a . | (N=737)a . | ||||
| Characteristic . | No. or Median . | % or IQR . | No. or Median . | % or IQR . | No. or Median . | % or IQR . | |
| Sex | |||||||
| Male | 1,199 | 78 | 597 | 52 | 558 | 48 | |
| Female | 331 | 22 | 134 | 43 | 179 | 57 | 0.005 |
| Age at diagnosis, years | 69 | 63–75 | 69.0 | 63–76 | 69 | 63–75 | 0.19 |
| Age at survey, years | 75 | 70–81 | 76.0 | 70–82 | 75 | 70–80 | 0.003 |
| No. of other LTCs | |||||||
| None | 364 | 24 | 163 | 47 | 187 | 53 | |
| 1 | 466 | 30 | 222 | 50 | 226 | 50 | |
| 2 | 320 | 21 | 145 | 48 | 159 | 52 | |
| 3 | 205 | 13 | 106 | 53 | 95 | 47 | |
| ≥4 | 175 | 11 | 95 | 58 | 70 | 42 | 0.15 |
| IMD | |||||||
| 1 (least deprived) | 345 | 23 | 169 | 52 | 157 | 48 | |
| 2 | 388 | 25 | 174 | 47 | 196 | 53 | |
| 3 | 323 | 21 | 155 | 49 | 162 | 51 | |
| 4 | 240 | 16 | 117 | 52 | 109 | 48 | |
| 5 (most deprived) | 234 | 15 | 116 | 51 | 113 | 49 | 0.70 |
| Employment status | |||||||
| Employed | 176 | 12 | 76 | 44 | 97 | 56 | |
| Unemployed | 28 | 2 | 11 | 41 | 16 | 59 | |
| Retired | 1,277 | 83 | 615 | 50 | 605 | 50 | 0.19 |
| Other | 13 | 1 | 7 | 54 | 6 | 46 | |
| Not known | 36 | 2 | 22 | 63 | 13 | 37 | |
| Relationship status | |||||||
| Married/Civil partnership | 1,012 | 66 | 477 | 49 | 503 | 51 | |
| Separated/Divorced | 135 | 9 | 56 | 43 | 75 | 57 | |
| Widowed/Surviving Partner | 255 | 17 | 136 | 57 | 101 | 43 | |
| Single | 51 | 3 | 25 | 53 | 22 | 47 | 0.03 |
| Other | 21 | 1 | 12 | 60 | 8 | 40 | |
| Not known | 56 | 4 | 25 | 47 | 28 | 53 | |
| Smoking | |||||||
| Never smoker | 405 | 26 | 194 | 50 | 194 | 50 | |
| Ex-smoker | 914 | 60 | 438 | 50 | 441 | 50 | |
| Current smoker | 143 | 9 | 72 | 52 | 66 | 48 | 0.88 |
| Not known | 68 | 4 | 27 | 43 | 36 | 57 | |
| GODIN Exercise | |||||||
| Insufficiently active | 809 | 53 | 380 | 49 | 401 | 51 | |
| Moderately active | 109 | 7 | 50 | 48 | 55 | 52 | |
| Active | 242 | 16 | 129 | 55 | 105 | 45 | 0.20 |
| Not known | 370 | 24 | 172 | 49 | 176 | 51 | |
| Carer | |||||||
| No | 1,132 | 74 | 538 | 50 | 547 | 50 | |
| Yes | 297 | 19 | 149 | 52 | 138 | 48 | 0.48 |
| Not known | 101 | 7 | 44 | 46 | 52 | 54 | |
| Ethnicity | |||||||
| White | 1,455 | 95 | 696 | 50 | 700 | 50 | |
| Non white | 16 | 1 | 10 | 63 | 6 | 38 | 0.45 |
| Not known | 59 | 4 | 25 | 45 | 31 | 55 | |
BCG = Bacillus Calmette-Guerin; GODIN = Godin Leisure-Time Exercise Questionnaire; IMD=Index of Multiple Deprivation; LTCs= Long Term Conditions; MMC = Intravesical Mitomycin C; TURBT = Transurethral Resection of a Bladder Tumour
N=62 out of N=1530 with Treatment Other/Not known excluded from analysis
Response Rates
The highest response rate was for the question on sexual interest (100%). The lowest response rates were for questions on sexual enjoyment (78% of those who reported being sexually active), risk of contaminating partner worry (78% of the sexually active), and female sexual problems (78% of the sexually active) (Supplementary Table 3).
Sexual item response rates varied most by relationship status (Supplementary Table 3). Participants who were not in a relationship (but reported being sexually active) had lower response rates for questions on sexual intimacy (69% [no relationship] vs 83% [in a relationship]), risk of contaminating partner (65% vs 82%), sexual enjoyment (66% vs 82%) and female sexual problems (64% vs 81%) compared to those in a relationship.
Sexual Activity by Participant Demographics
In total, 31% of participants reported being sexually active in the last 4 weeks (Table 2). Rates of sexual activity varied with sex, age and LTCs. In particular, fewer women were sexually active compared to men (‘A little’, ‘Quite a bit’ or ‘Very much’: 19% [females] vs 34% [males], P<0.001), and the proportion of participants <65 years who were sexually active was double that of the 75–84 age group (50% vs 25% respectively, P<0.001, Table 2). Participants with 4+ LTCs were much less likely to belong to the sexually active group than participants with no LTCs (17% vs 38%, P<0.001). There were no significant differences in sexual activity with respect to carer roles or smoking status (Table 2). Participants with cardiovascular conditions or diabetes were less likely to be sexually active than participants without LTCs (% Sexually active: 23% for heart conditions, 17% for angina, 26% for strokes, 27% for hypertension only, 27% for diabetes vs 38% for no LTCs (Table 3).
| . | Total . | Sexually Active . | Not Sexually Active . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | (N=1,530) . | (N=471) . | (N=1,059) . | . | . | . | . | |||
| Characteristic . | No. . | % . | No. . | %a . | No. . | %a . | Unadjusted ORs . | 95 % CI . | p value . | |
| Sex | ||||||||||
| Male | 1199 | 78 | 407 | 34 | 792 | 66 | 1.00 | |||
| Female | 331 | 22 | 64 | 19 | 267 | 81 | 0.47 | 0.35 | 0.63 | <0.001 |
| Age, years | ||||||||||
| <65 | 179 | 12 | 90 | 50 | 89 | 50 | 3.06 | 2.17 | 4.32 | <0.001 |
| 65-74 | 522 | 34 | 198 | 38 | 324 | 62 | 1.85 | 1.43 | 2.38 | <0.001 |
| 75-84 | 616 | 40 | 153 | 25 | 463 | 75 | 1.00 | |||
| ≥85 | 213 | 14 | 30 | 14 | 183 | 86 | 0.50 | 0.32 | 0.76 | 0.001 |
| No. long-term conditions | ||||||||||
| None | 364 | 24 | 137 | 38 | 227 | 62 | 1.00 | |||
| 1 | 466 | 30 | 168 | 36 | 298 | 64 | 0.93 | 0.70 | 1.24 | 0.64 |
| 2 | 320 | 21 | 96 | 30 | 224 | 70 | 0.71 | 0.52 | 0.98 | 0.04 |
| 3 | 205 | 13 | 40 | 20 | 165 | 80 | 0.40 | 0.27 | 0.60 | <0.001 |
| 4+ | 175 | 11 | 30 | 17 | 145 | 83 | 0.34 | 0.22 | 0.54 | <0.001 |
| Relationship status | ||||||||||
| Married/Civil partnership | 1012 | 66 | 350 | 35 | 662 | 65 | 1.00 | |||
| Separated/Divorced | 135 | 9 | 40 | 30 | 95 | 70 | 0.80 | 0.54 | 1.18 | 0.25 |
| Widowed/Surviving Partner | 255 | 17 | 44 | 17 | 211 | 83 | 0.39 | 0.28 | 0.56 | <0.001 |
| Single | 51 | 3 | 14 | 27 | 37 | 73 | 0.72 | 0.38 | 1.34 | 0.30 |
| Other / Not known | 77 | 5 | 23 | 30 | 54 | 70 | n/a | n/a | n/a | |
| Index of Multiple Deprivation | ||||||||||
| 1, 2 or 3 (least deprived) | 1056 | 69 | 339 | 32 | 717 | 68 | 1.00 | |||
| 4 or 5 (most deprived) | 474 | 31 | 132 | 28 | 342 | 72 | 0.82 | 0.64 | 1.04 | 0.10 |
| Ethnicity | ||||||||||
| White | 1455 | 95 | 446 | 31 | 1009 | 69 | 1.00 | |||
| Non-white | 16 | 1 | 10 | 63 | 6 | 38 | 3.77 | 1.36 | 10.44 | 0.01 |
| Not known | 59 | 4 | 15 | 25 | 44 | 75 | n/a | n/a | n/a | |
| Carer | ||||||||||
| No | 1132 | 74 | 353 | 31 | 779 | 69 | 1.00 | |||
| Yes | 297 | 19 | 94 | 32 | 203 | 68 | 1.02 | 0.78 | 1.35 | 0.88 |
| Not known | 101 | 7 | 24 | 24 | 77 | 76 | n/a | n/a | n/a | |
| Smoking | ||||||||||
| Never smoker | 405 | 27 | 118 | 29 | 287 | 71 | 0.93 | 0.72 | 1.20 | 0.56 |
| Ex-smoker | 914 | 60 | 281 | 31 | 633 | 69 | 1.00 | |||
| Current smoker | 143 | 9 | 49 | 34 | 94 | 66 | 1.17 | 0.81 | 1.70 | 0.40 |
| Not known | 68 | 5 | 23 | 34 | 45 | 66 | n/a | n/a | n/a | |
| Treatment | ||||||||||
| TURBT ± BCG/MMC | 731 | 48 | 260 | 36 | 471 | 64 | 1.00 | |||
| RC or Radical RT ± other | 737 | 48 | 194 | 26 | 543 | 74 | 0.65 | 0.52 | 0.81 | <0.001 |
| Other / Not known | 62 | 4 | 17 | 27 | 45 | 73 | n/a | n/a | n/a | |
| . | Total . | Sexually Active . | Not Sexually Active . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | (N=1,530) . | (N=471) . | (N=1,059) . | . | . | . | . | |||
| Characteristic . | No. . | % . | No. . | %a . | No. . | %a . | Unadjusted ORs . | 95 % CI . | p value . | |
| Sex | ||||||||||
| Male | 1199 | 78 | 407 | 34 | 792 | 66 | 1.00 | |||
| Female | 331 | 22 | 64 | 19 | 267 | 81 | 0.47 | 0.35 | 0.63 | <0.001 |
| Age, years | ||||||||||
| <65 | 179 | 12 | 90 | 50 | 89 | 50 | 3.06 | 2.17 | 4.32 | <0.001 |
| 65-74 | 522 | 34 | 198 | 38 | 324 | 62 | 1.85 | 1.43 | 2.38 | <0.001 |
| 75-84 | 616 | 40 | 153 | 25 | 463 | 75 | 1.00 | |||
| ≥85 | 213 | 14 | 30 | 14 | 183 | 86 | 0.50 | 0.32 | 0.76 | 0.001 |
| No. long-term conditions | ||||||||||
| None | 364 | 24 | 137 | 38 | 227 | 62 | 1.00 | |||
| 1 | 466 | 30 | 168 | 36 | 298 | 64 | 0.93 | 0.70 | 1.24 | 0.64 |
| 2 | 320 | 21 | 96 | 30 | 224 | 70 | 0.71 | 0.52 | 0.98 | 0.04 |
| 3 | 205 | 13 | 40 | 20 | 165 | 80 | 0.40 | 0.27 | 0.60 | <0.001 |
| 4+ | 175 | 11 | 30 | 17 | 145 | 83 | 0.34 | 0.22 | 0.54 | <0.001 |
| Relationship status | ||||||||||
| Married/Civil partnership | 1012 | 66 | 350 | 35 | 662 | 65 | 1.00 | |||
| Separated/Divorced | 135 | 9 | 40 | 30 | 95 | 70 | 0.80 | 0.54 | 1.18 | 0.25 |
| Widowed/Surviving Partner | 255 | 17 | 44 | 17 | 211 | 83 | 0.39 | 0.28 | 0.56 | <0.001 |
| Single | 51 | 3 | 14 | 27 | 37 | 73 | 0.72 | 0.38 | 1.34 | 0.30 |
| Other / Not known | 77 | 5 | 23 | 30 | 54 | 70 | n/a | n/a | n/a | |
| Index of Multiple Deprivation | ||||||||||
| 1, 2 or 3 (least deprived) | 1056 | 69 | 339 | 32 | 717 | 68 | 1.00 | |||
| 4 or 5 (most deprived) | 474 | 31 | 132 | 28 | 342 | 72 | 0.82 | 0.64 | 1.04 | 0.10 |
| Ethnicity | ||||||||||
| White | 1455 | 95 | 446 | 31 | 1009 | 69 | 1.00 | |||
| Non-white | 16 | 1 | 10 | 63 | 6 | 38 | 3.77 | 1.36 | 10.44 | 0.01 |
| Not known | 59 | 4 | 15 | 25 | 44 | 75 | n/a | n/a | n/a | |
| Carer | ||||||||||
| No | 1132 | 74 | 353 | 31 | 779 | 69 | 1.00 | |||
| Yes | 297 | 19 | 94 | 32 | 203 | 68 | 1.02 | 0.78 | 1.35 | 0.88 |
| Not known | 101 | 7 | 24 | 24 | 77 | 76 | n/a | n/a | n/a | |
| Smoking | ||||||||||
| Never smoker | 405 | 27 | 118 | 29 | 287 | 71 | 0.93 | 0.72 | 1.20 | 0.56 |
| Ex-smoker | 914 | 60 | 281 | 31 | 633 | 69 | 1.00 | |||
| Current smoker | 143 | 9 | 49 | 34 | 94 | 66 | 1.17 | 0.81 | 1.70 | 0.40 |
| Not known | 68 | 5 | 23 | 34 | 45 | 66 | n/a | n/a | n/a | |
| Treatment | ||||||||||
| TURBT ± BCG/MMC | 731 | 48 | 260 | 36 | 471 | 64 | 1.00 | |||
| RC or Radical RT ± other | 737 | 48 | 194 | 26 | 543 | 74 | 0.65 | 0.52 | 0.81 | <0.001 |
| Other / Not known | 62 | 4 | 17 | 27 | 45 | 73 | n/a | n/a | n/a | |
BCG = Bacillus Calmette-Guerin; MMC = Intravesical Mitomycin C; RC = Radical Cystectomy; RT = Radiotherapy; TURBT = Transurethral Resection of a Bladder Tumour
Row percentages used to show distribution of sexual activity by patient characteristic, rather than by outcome
| . | Total . | Sexually Active . | Not Sexually Active . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | (N=1,530) . | (N=471) . | (N=1,059) . | . | . | . | . | |||
| Characteristic . | No. . | % . | No. . | %a . | No. . | %a . | Unadjusted ORs . | 95 % CI . | p value . | |
| Sex | ||||||||||
| Male | 1199 | 78 | 407 | 34 | 792 | 66 | 1.00 | |||
| Female | 331 | 22 | 64 | 19 | 267 | 81 | 0.47 | 0.35 | 0.63 | <0.001 |
| Age, years | ||||||||||
| <65 | 179 | 12 | 90 | 50 | 89 | 50 | 3.06 | 2.17 | 4.32 | <0.001 |
| 65-74 | 522 | 34 | 198 | 38 | 324 | 62 | 1.85 | 1.43 | 2.38 | <0.001 |
| 75-84 | 616 | 40 | 153 | 25 | 463 | 75 | 1.00 | |||
| ≥85 | 213 | 14 | 30 | 14 | 183 | 86 | 0.50 | 0.32 | 0.76 | 0.001 |
| No. long-term conditions | ||||||||||
| None | 364 | 24 | 137 | 38 | 227 | 62 | 1.00 | |||
| 1 | 466 | 30 | 168 | 36 | 298 | 64 | 0.93 | 0.70 | 1.24 | 0.64 |
| 2 | 320 | 21 | 96 | 30 | 224 | 70 | 0.71 | 0.52 | 0.98 | 0.04 |
| 3 | 205 | 13 | 40 | 20 | 165 | 80 | 0.40 | 0.27 | 0.60 | <0.001 |
| 4+ | 175 | 11 | 30 | 17 | 145 | 83 | 0.34 | 0.22 | 0.54 | <0.001 |
| Relationship status | ||||||||||
| Married/Civil partnership | 1012 | 66 | 350 | 35 | 662 | 65 | 1.00 | |||
| Separated/Divorced | 135 | 9 | 40 | 30 | 95 | 70 | 0.80 | 0.54 | 1.18 | 0.25 |
| Widowed/Surviving Partner | 255 | 17 | 44 | 17 | 211 | 83 | 0.39 | 0.28 | 0.56 | <0.001 |
| Single | 51 | 3 | 14 | 27 | 37 | 73 | 0.72 | 0.38 | 1.34 | 0.30 |
| Other / Not known | 77 | 5 | 23 | 30 | 54 | 70 | n/a | n/a | n/a | |
| Index of Multiple Deprivation | ||||||||||
| 1, 2 or 3 (least deprived) | 1056 | 69 | 339 | 32 | 717 | 68 | 1.00 | |||
| 4 or 5 (most deprived) | 474 | 31 | 132 | 28 | 342 | 72 | 0.82 | 0.64 | 1.04 | 0.10 |
| Ethnicity | ||||||||||
| White | 1455 | 95 | 446 | 31 | 1009 | 69 | 1.00 | |||
| Non-white | 16 | 1 | 10 | 63 | 6 | 38 | 3.77 | 1.36 | 10.44 | 0.01 |
| Not known | 59 | 4 | 15 | 25 | 44 | 75 | n/a | n/a | n/a | |
| Carer | ||||||||||
| No | 1132 | 74 | 353 | 31 | 779 | 69 | 1.00 | |||
| Yes | 297 | 19 | 94 | 32 | 203 | 68 | 1.02 | 0.78 | 1.35 | 0.88 |
| Not known | 101 | 7 | 24 | 24 | 77 | 76 | n/a | n/a | n/a | |
| Smoking | ||||||||||
| Never smoker | 405 | 27 | 118 | 29 | 287 | 71 | 0.93 | 0.72 | 1.20 | 0.56 |
| Ex-smoker | 914 | 60 | 281 | 31 | 633 | 69 | 1.00 | |||
| Current smoker | 143 | 9 | 49 | 34 | 94 | 66 | 1.17 | 0.81 | 1.70 | 0.40 |
| Not known | 68 | 5 | 23 | 34 | 45 | 66 | n/a | n/a | n/a | |
| Treatment | ||||||||||
| TURBT ± BCG/MMC | 731 | 48 | 260 | 36 | 471 | 64 | 1.00 | |||
| RC or Radical RT ± other | 737 | 48 | 194 | 26 | 543 | 74 | 0.65 | 0.52 | 0.81 | <0.001 |
| Other / Not known | 62 | 4 | 17 | 27 | 45 | 73 | n/a | n/a | n/a | |
| . | Total . | Sexually Active . | Not Sexually Active . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | (N=1,530) . | (N=471) . | (N=1,059) . | . | . | . | . | |||
| Characteristic . | No. . | % . | No. . | %a . | No. . | %a . | Unadjusted ORs . | 95 % CI . | p value . | |
| Sex | ||||||||||
| Male | 1199 | 78 | 407 | 34 | 792 | 66 | 1.00 | |||
| Female | 331 | 22 | 64 | 19 | 267 | 81 | 0.47 | 0.35 | 0.63 | <0.001 |
| Age, years | ||||||||||
| <65 | 179 | 12 | 90 | 50 | 89 | 50 | 3.06 | 2.17 | 4.32 | <0.001 |
| 65-74 | 522 | 34 | 198 | 38 | 324 | 62 | 1.85 | 1.43 | 2.38 | <0.001 |
| 75-84 | 616 | 40 | 153 | 25 | 463 | 75 | 1.00 | |||
| ≥85 | 213 | 14 | 30 | 14 | 183 | 86 | 0.50 | 0.32 | 0.76 | 0.001 |
| No. long-term conditions | ||||||||||
| None | 364 | 24 | 137 | 38 | 227 | 62 | 1.00 | |||
| 1 | 466 | 30 | 168 | 36 | 298 | 64 | 0.93 | 0.70 | 1.24 | 0.64 |
| 2 | 320 | 21 | 96 | 30 | 224 | 70 | 0.71 | 0.52 | 0.98 | 0.04 |
| 3 | 205 | 13 | 40 | 20 | 165 | 80 | 0.40 | 0.27 | 0.60 | <0.001 |
| 4+ | 175 | 11 | 30 | 17 | 145 | 83 | 0.34 | 0.22 | 0.54 | <0.001 |
| Relationship status | ||||||||||
| Married/Civil partnership | 1012 | 66 | 350 | 35 | 662 | 65 | 1.00 | |||
| Separated/Divorced | 135 | 9 | 40 | 30 | 95 | 70 | 0.80 | 0.54 | 1.18 | 0.25 |
| Widowed/Surviving Partner | 255 | 17 | 44 | 17 | 211 | 83 | 0.39 | 0.28 | 0.56 | <0.001 |
| Single | 51 | 3 | 14 | 27 | 37 | 73 | 0.72 | 0.38 | 1.34 | 0.30 |
| Other / Not known | 77 | 5 | 23 | 30 | 54 | 70 | n/a | n/a | n/a | |
| Index of Multiple Deprivation | ||||||||||
| 1, 2 or 3 (least deprived) | 1056 | 69 | 339 | 32 | 717 | 68 | 1.00 | |||
| 4 or 5 (most deprived) | 474 | 31 | 132 | 28 | 342 | 72 | 0.82 | 0.64 | 1.04 | 0.10 |
| Ethnicity | ||||||||||
| White | 1455 | 95 | 446 | 31 | 1009 | 69 | 1.00 | |||
| Non-white | 16 | 1 | 10 | 63 | 6 | 38 | 3.77 | 1.36 | 10.44 | 0.01 |
| Not known | 59 | 4 | 15 | 25 | 44 | 75 | n/a | n/a | n/a | |
| Carer | ||||||||||
| No | 1132 | 74 | 353 | 31 | 779 | 69 | 1.00 | |||
| Yes | 297 | 19 | 94 | 32 | 203 | 68 | 1.02 | 0.78 | 1.35 | 0.88 |
| Not known | 101 | 7 | 24 | 24 | 77 | 76 | n/a | n/a | n/a | |
| Smoking | ||||||||||
| Never smoker | 405 | 27 | 118 | 29 | 287 | 71 | 0.93 | 0.72 | 1.20 | 0.56 |
| Ex-smoker | 914 | 60 | 281 | 31 | 633 | 69 | 1.00 | |||
| Current smoker | 143 | 9 | 49 | 34 | 94 | 66 | 1.17 | 0.81 | 1.70 | 0.40 |
| Not known | 68 | 5 | 23 | 34 | 45 | 66 | n/a | n/a | n/a | |
| Treatment | ||||||||||
| TURBT ± BCG/MMC | 731 | 48 | 260 | 36 | 471 | 64 | 1.00 | |||
| RC or Radical RT ± other | 737 | 48 | 194 | 26 | 543 | 74 | 0.65 | 0.52 | 0.81 | <0.001 |
| Other / Not known | 62 | 4 | 17 | 27 | 45 | 73 | n/a | n/a | n/a | |
BCG = Bacillus Calmette-Guerin; MMC = Intravesical Mitomycin C; RC = Radical Cystectomy; RT = Radiotherapy; TURBT = Transurethral Resection of a Bladder Tumour
Row percentages used to show distribution of sexual activity by patient characteristic, rather than by outcome
| Long Term Condition . | Sexually Active . | Not sexually Active . | ||
|---|---|---|---|---|
| . | % . | 95% CI . | % . | 95% CI . |
| Heart condition | 23 | 19–28 | 77 | 72–81 |
| Angina | 17 | 11–24 | 83 | 76–89 |
| Stroke | 26 | 17–36 | 74 | 64–83 |
| Hypertension | 27 | 23–30 | 73 | 70–77 |
| Diabetes | 27 | 22–33 | 73 | 67–78 |
| Arthritis | 22 | 18–26 | 78 | 74–82 |
| Asthma/chronic chest problem | 26 | 21–33 | 74 | 67–79 |
| Stomach, bowel, or gallbladder problem | 25 | 20–31 | 75 | 69–80 |
| Kidney disease | 20 | 14–28 | 80 | 72–86 |
| Alzheimer’s/dementia | 13 | 4–31 | 88 | 69–96 |
| Epilepsy | 16 | 6–38 | 84 | 62–94 |
| Neurological problem | 27 | 17–40 | 73 | 60–83 |
| Liver or Pancreas problem | 13 | 5–28 | 88 | 72–95 |
| None | 38 | 33–43 | 62 | 57–67 |
| Long Term Condition . | Sexually Active . | Not sexually Active . | ||
|---|---|---|---|---|
| . | % . | 95% CI . | % . | 95% CI . |
| Heart condition | 23 | 19–28 | 77 | 72–81 |
| Angina | 17 | 11–24 | 83 | 76–89 |
| Stroke | 26 | 17–36 | 74 | 64–83 |
| Hypertension | 27 | 23–30 | 73 | 70–77 |
| Diabetes | 27 | 22–33 | 73 | 67–78 |
| Arthritis | 22 | 18–26 | 78 | 74–82 |
| Asthma/chronic chest problem | 26 | 21–33 | 74 | 67–79 |
| Stomach, bowel, or gallbladder problem | 25 | 20–31 | 75 | 69–80 |
| Kidney disease | 20 | 14–28 | 80 | 72–86 |
| Alzheimer’s/dementia | 13 | 4–31 | 88 | 69–96 |
| Epilepsy | 16 | 6–38 | 84 | 62–94 |
| Neurological problem | 27 | 17–40 | 73 | 60–83 |
| Liver or Pancreas problem | 13 | 5–28 | 88 | 72–95 |
| None | 38 | 33–43 | 62 | 57–67 |
*Frequencies not shown due to potential for identification.
| Long Term Condition . | Sexually Active . | Not sexually Active . | ||
|---|---|---|---|---|
| . | % . | 95% CI . | % . | 95% CI . |
| Heart condition | 23 | 19–28 | 77 | 72–81 |
| Angina | 17 | 11–24 | 83 | 76–89 |
| Stroke | 26 | 17–36 | 74 | 64–83 |
| Hypertension | 27 | 23–30 | 73 | 70–77 |
| Diabetes | 27 | 22–33 | 73 | 67–78 |
| Arthritis | 22 | 18–26 | 78 | 74–82 |
| Asthma/chronic chest problem | 26 | 21–33 | 74 | 67–79 |
| Stomach, bowel, or gallbladder problem | 25 | 20–31 | 75 | 69–80 |
| Kidney disease | 20 | 14–28 | 80 | 72–86 |
| Alzheimer’s/dementia | 13 | 4–31 | 88 | 69–96 |
| Epilepsy | 16 | 6–38 | 84 | 62–94 |
| Neurological problem | 27 | 17–40 | 73 | 60–83 |
| Liver or Pancreas problem | 13 | 5–28 | 88 | 72–95 |
| None | 38 | 33–43 | 62 | 57–67 |
| Long Term Condition . | Sexually Active . | Not sexually Active . | ||
|---|---|---|---|---|
| . | % . | 95% CI . | % . | 95% CI . |
| Heart condition | 23 | 19–28 | 77 | 72–81 |
| Angina | 17 | 11–24 | 83 | 76–89 |
| Stroke | 26 | 17–36 | 74 | 64–83 |
| Hypertension | 27 | 23–30 | 73 | 70–77 |
| Diabetes | 27 | 22–33 | 73 | 67–78 |
| Arthritis | 22 | 18–26 | 78 | 74–82 |
| Asthma/chronic chest problem | 26 | 21–33 | 74 | 67–79 |
| Stomach, bowel, or gallbladder problem | 25 | 20–31 | 75 | 69–80 |
| Kidney disease | 20 | 14–28 | 80 | 72–86 |
| Alzheimer’s/dementia | 13 | 4–31 | 88 | 69–96 |
| Epilepsy | 16 | 6–38 | 84 | 62–94 |
| Neurological problem | 27 | 17–40 | 73 | 60–83 |
| Liver or Pancreas problem | 13 | 5–28 | 88 | 72–95 |
| None | 38 | 33–43 | 62 | 57–67 |
*Frequencies not shown due to potential for identification.
Sexual Function by Sex
The EORTC sexual questionnaire used in this study only included one female-specific sexual function item about vaginal dryness/problems with intercourse. Over a third (36%) of sexually active women reported problems with vaginal dryness/problems with intercourse (answering ‘quite a bit or ‘very much’ (Figure 1). Over two thirds (67%) of men reported erectile difficulty (answering ‘quite a bit or ‘very much’) and half of men (50%) reported ejaculation problems (answering ‘quite a bit or ‘very much’) (Figure 1).
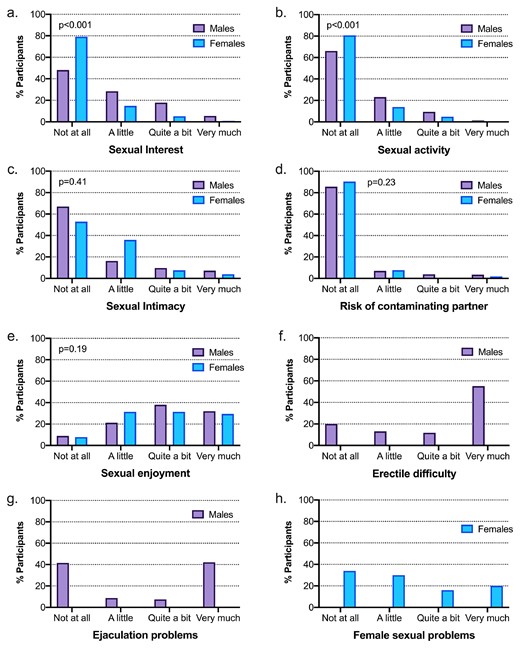
Rates of sexual interest were higher in men than women (23% vs 6% respectively reporting ‘Quite a bit’ or ‘Very much’, P<0.001, Figure 1). Similarly, more males were sexually active compared to females (answering ‘A little’, ‘Quite a bit’ or ‘Very much’: 34% [males] vs 19% [females], P<0.001, Figure 1).
Mean sexual function scores were higher in men compared to women (21.2 [males] vs 8.9 [females], P<0.001, Figure 2 a and Supplementary Table 4). No statistically significant differences were seen for intimacy problems, fear of contaminating partner or sexual enjoyment.
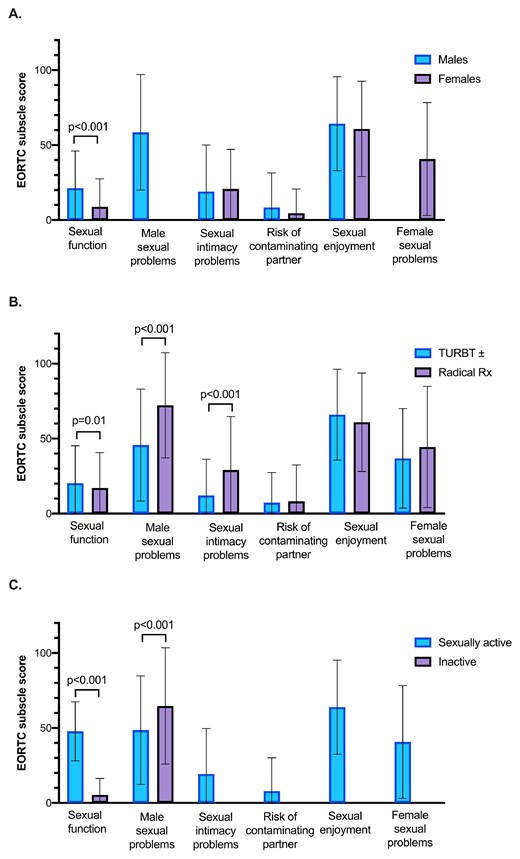
Sexual Scores (Mean and Standard Deviation) For Each Subscale Stratified by (A) Sex, (B) Treatment Received and (C) Sexual Activity. For each, a higher score either represents better function, more enjoyment or more problems.
Sexual Activity and Function by Treatment Received
Participants who received radical treatment (RC or RT+/- systemic treatments) were less likely to be sexually active compared to those who underwent local treatment (TURBT+/- intravesical agents) (26% vs 36% respectively, Unadjusted OR 0.65 [95% CI 0.52–0.81], [<0.001) (Table 2). This difference persisted after adjustment for age, sex, LTCs, relationship status and IMD (adjusted OR 0.56, 95% CI: 0.44 -0.72, P<0.001) and might reflect lack of interest and/or poorer sexual function.
However, there was no significant difference in sexual interest between those receiving radical treatment compared to TURBT (‘Quite a bit’ or ‘Very much’: 19% [radical treatment] vs 21% [TURBT], P=0.35) (Figure 3). A larger proportion of men who had received radical treatment reported more severe erectile dysfunction (‘Quite a bit’ or ‘Very much’: 81% [radical] vs 54% [TURBT], P>0.001), ejaculatory problems (‘Quite a bit’ or ‘Very much’: 65% [radical] vs 36% [TURBT], P<0.001) and intimacy problems (‘Quite a bit’ or ‘Very much’: 26% [radical] vs 10% [TURBT], P<0.001) compared to TURBT+/- adjuvant treatments (Figure 3).
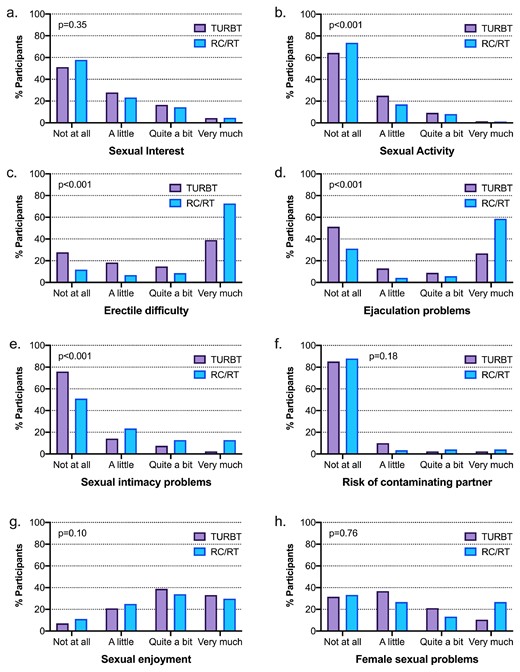
Responses to Each Individual Question Stratified by Treatment Received.
There was no significant difference between the treatments in females who reported vaginal dryness/problems with intercourse (‘Quite a bit’ or ‘Very much’: 40% [radical treatment] vs 32% [TURBT], p=0.76), though limited by few participants (Figure 3). Participants who had received radical treatment had worse mean scores for sexual function (17.1 [radical treatment] vs 20.3, P=0.01), male sexual problems (72.2 [radical treatment] vs 45.7, P<0.001) and intimacy problems (29.1 [radical treatment] vs 12.1, P<0.001) than those who had received TURBT+/- adjuvant treatments (Figure 2b and Supplementary Table 5). There were no statistically significant differences in concerns over contaminating partner and sexual enjoyment scores.
Sexual Function by Sexual Activity
There were marked differences in the rate of sexual interest between sexually active and inactive participants (Supplementary Figure 1). For example, 48% of sexually active participants were ‘Quite a bit’ or ‘Very much’ interested in sex, compared to 7% of inactive participants (P<0.001). Males who were not sexually active were more likely to report erectile dysfunction (‘Quite a bit’ or ‘very much’: 76% [not active] vs 52% [active]) and ejaculatory problems (‘Quite a bit’ or ‘very much’: 56% [not active] vs 40% [active]) (both P<0.001). Males who were sexually active had lower scores for male sexual problems compared to inactive respondents (48.6 [active] vs 64.7 [not active], P<0.001, Figure 2c and Supplementary Table 6).
DISCUSSION
This study provides the largest in-depth analysis of sexual activity and function after BC diagnosis and treatment, to date. We present a large multi-centre study showing data from a population that has traditionally been difficult to reach. Additionally, it is one of very few studies evaluating sexual function in patients with NMIBC. There are several key findings: Firstly, a significant proportion of sexually active men and female participants reported sexual problems. Secondly, we found that compared to men, women reported less sexual interest, were less sexually active and had overall worse sexual function. Finally, individuals who have undergone radical treatments for BC were less likely to be sexually active and this was independent of age, sex, LTCs, relationship status and IMD, and reported worse sexual intimacy problems and (male) sexual problems compared to those undergoing TURBT.
High rates of male and female sexual problems were reported in both TURBT and radical treatment groups. Erectile and ejaculatory dysfunction were even higher in the radical group. These findings are supported by studies demonstrating the impact of radical treatment on specific male and female sexual function parameters.7,17 In addition, our finding of worse overall sexual function with radical treatment compared to non-radical treatments in BC confirm a previous smaller series.18 The impact of cystoscopic treatment on sexual function outcomes has been reported to a lesser degree. A study of 117 NMIBC patients demonstrated vaginal dryness in 63% of sexually active females, as well as erectile dysfunction and ejaculation problems in 60% and 43% of sexually active males respectively.6 This data provides a useful insight for the clinician into the magnitude of sexual dysfunction in the BC patient cohort.
We found that compared to men, women were less sexually active, had less sexual interest and had overall worse sexual function. This finding supports previous work in 117 NMIBC patients that found fewer women were sexually active compared to men (percentage sexually active: 44% vs 69% [men]) and fewer women had interest in sex compared to men (percentage with interest in sex: 68% vs 87% [men]).6 It is imperative that clinicians are aware of the prevalence of male and female sexual dysfunction, effectively counsel patients pre-treatment, and proactively ask about their symptoms post treatment.
The likelihood of participants being sexually active, reduced with increasing age and a greater number of self-reported LTCs. With regards to LTCs, participants with cardiovascular conditions or diabetes were less likely to be sexually active than participants without LTCs. This is supported by studies demonstrating a link between age, co-morbidities such as hypertension and diabetes and erectile dysfunction19,20 as well as female sexual dysfunction.21 Furthermore, younger age (less than 65 years) has been shown to be associated with better erectile function following RC.22 These findings are exploratory but highlight the potential effects of specific conditions on sexual activity in BC patients. The findings have direct clinical relevance to the pre-op counselling process and shared decision making prior to BC treatments.
Limitations
Firstly, the sexual activity and sexual function questions were included as part of a wider set of quality of life measures. Therefore, the breadth and content of the sexual items in the questionnaires were not as comprehensive as other available measures and limits some of the conclusions that can be drawn. Secondly, there were slightly lower response rates for some of the questions on sexual function compared to other measures which can represent a bias. However, out of the participants who answered questions on sexual activity, all the sexual function questions had at least a 78% response rate. The overall response rate to the sexual activity question, out of the participants who returned a completed survey, was 85% which is higher than has been reported in another recent quality of life questionnaire based study.1
Thirdly, as we did not have data on participants’ sexual activity or sexual function prior to BC treatment, it is not possible to ascertain whether differences in sexual function and sexual activity between treatment groups are due to the treatment itself or pre-morbid states. In addition, participants were between 1–10 years beyond their BC diagnosis and therefore non-treatment related factors may play a confounding role with respect to sexual dysfunction. There is also heterogeneity with respect to time passed since last treatment for BC and this may have influenced the results. Finally, due to the small numbers of patients who underwent RT in our cohort, we merged RC and RT into one category representing radical treatments. However, we did note that there were no differences in sexual activity rates between the two groups.
CONCLUSIONS
Sexual dysfunction is very common in patients with a diagnosis of BC and not confined to those with MIBC. However, compared to endoscopic treatments, radical treatments for BC are associated with worse sexual function. Both men and women report significant problems with sexual function. It is essential that clinical teams recognise the potential for sexual dysfunction at all stages of the BC care pathway. The results from this study should be used to support evidence-based counselling prior to BC treatments and pro-active enquiry and support following treatments.
STATEMENT OF AUTHORSHIP
Conceptualization, JC and AG; Methodology, JC, AG, AD and KA; Investigation, JC, AG, AD, ZR and KA; Writing – Original Draft, IJ, JC, AG, AD, ZR and KA; Writing – Review & Editing, IJ, JC, AG, AD, ZR and KA; Funding Acquisition, JC and AG; Resources, SB, ZR.; Supervision, JC, AG, KA and AD.
Funding
The study was funded by Yorkshire Cancer Research (Study S385: The Yorkshire Cancer Research Bladder Cancer Patient Reported Outcomes Survey). The funder had no role in the design, analysis or collection of the data; in writing the manuscript; or in the decision to submit the manuscript for publication. JWFC is funded by an NIHR Research Professorship.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jsxm.2022.06.016.
Acknowledgment
We gratefully acknowledge the support of participants and local principal investigators and thank Penny Wright and Sam Mason for their contributions to the design and delivery of Life And Bladder Cancer research. We acknowledge the support of the User, Clinical and Scientific Advisory Group: Linda Sharpe (Chair), Jo Cresswell, Louise Goodwin, Mohini Varughese, Sally Appleyard, Ananya Choudhury, Rik Bryan, Duncan Nekeman, Andrew Winterbottom (deceased), Caroline Raw, Sophie Jose, Charlotte Eversfield, Hannah Roberts, Ashok Nikapota and Sunjay Jain. Colleagues at Quality Health supported survey distribution and results collation. This work uses data provided by patients and collected by the NHS as part of their care and support. This work is dedicated to patients who died before its completion, and in particular Andrew Winterbottom from Fight Bladder Cancer UK and Stanley Wilson.
REFERENCES
Author notes
Conflict of Interest: JWFC has received reimbursement for consultancy from Astra Zeneca, Roche and Janssen, speaker fees from BMS, MSD, Nucleix and Roche, and honoraria for membership of advisory boards from Astra Zeneca, Ferring, Roche and Janssen. The remaining authors declare no potential conflicts of interest.



