-
PDF
- Split View
-
Views
-
Cite
Cite
Claudia Pignatti Frederice, Ticiana Aparecida Alves de Mira, Helymar Costa Machado, Luiz Gustavo Oliveira Brito, Cássia R.T. Juliato, Effect of Vaginal Stretching and Photobiomodulation Therapy on Sexual Function in Women with Pelvic Floor Myofascial Pain - A Randomized Clinical Trial, The Journal of Sexual Medicine, Volume 19, Issue 1, January 2022, Pages 98–105, https://doi.org/10.1016/j.jsxm.2021.10.008
Close - Share Icon Share
ABSTRACT
Spasm or increased tonus of the pelvic floor muscles (PFM) can cause myofascial pain (MP), which may result in painful intercourse and sexual dysfunction.
The effect of vaginal stretching (VS) with photobiomodulation therapy (PBMT) is compared to VS with sham PBMT in overall sexual function, rate and severity of painful intercourse at baseline and after treatment in women with pelvic floor MP.
A double-blind randomized clinical trial of 103 women with MP: 1 group received 10 sessions of VS with PBMT (4 Joules of near-infrared light-808 nm at 3 points), and the other group received VS with sham PBMT.
Impact of treatment was measured by the number of women experiencing painful intercourse, Pain severity was measured by Visual Analog Scale and sexual function was assessed by the FSFI questionnaire. Variables were assessed at baseline and after ten sessions in the intervention groups.
After treatment, the number of women experiencing painful intercourse was significantly lower in both the VS with PBMT group (90.2–55%, P = .001), and VS with sham PBMT group (86.6–46.2%, P < .001). There was a significant reduction in pain measure by Visual Analog Scale (P < .001, [VS with PBMT group: P = .002; VS with sham PBMT group: P < .001]). There was a significant decrease in the number of participants with sexual dysfunction (FSFI score ≤26.55) after the treatment in the VS with PBMT group (92.2–74.5%, P = .003) and in the VS with sham PBMT group (90.4–76.9%, P = .035). Both groups showed improvement in the FSFI pain domain after treatment (P < .001, [VS with PBMT group: P = .038; VS with sham PBMT group: P = .005]). Only the VS with sham PBMT group had a significant increase in FSFI desire and total score (P < .001) after treatment.
We found that VS associated or not with PBMT may be effective in reducing complaints of painful intercourse, alleviating pain severity, and reducing the number of women with pelvic floor MP suffering from sexual dysfunction.
Strengths of this study are the randomized design and use of validated questionnaires. Limitation of the study is the lack of a long follow-up period and the lack of a usual care comparison group hampers generalizability of the results.
VS only and VS with PBMT have short-term efficacy in reducing painful intercourse and reducing a number of women with sexual dysfunction.
INTRODUCTION
Pelvic floor muscle (PFM) dysfunction is frequently associated with sexual dysfunction in women.1 Muscle changes related to hypertonic muscles, for example, myofascial dysfunction, spasm, PFM overactivity, are mainly associated with genitopelvic pain/penetration disorders, for example, dyspareunia, vaginismus, generalized vulvodynia and provoked vestibulodynia.1,2 There is a diversity of options for management of pain conditions. Physiotherapy is a treatment modality that uses different techniques: biofeedback, myofascial release, manual therapy, massage therapy, intravaginal stretching, laser, electrostimulation, local desensitization, behavioral and lifestyle changes. Medical treatment with botulinum toxin, anesthetics, steroids injections or diazepam suppository can also be adopted.3–5 Painful disorders compromise other domains of sexual function, such as desire, lubrication and orgasm2. Sexual complaints may result in personal distress or interpersonal difficulties.6
Myofascial Pain (MP) is characterized by the presence of a trigger point in a taut muscle band, in which pain is elicited by muscle compression.7 There is currently no standardization for pelvic floor MP (PFMP) assessment and painful digital vaginal palpation is the most widely used diagnostic method.8 It is a non-standardized method, resulting in subjective assessment.9 PFMP has been identified in 85% of women with some PFM disorder. Interest in the repercussions of this painful disorder has increased due to the high functional demands made by PFM muscles.10
PFM exercises and manual techniques are common therapeutic options for the conservative treatment of MP that have shown good results.6,11,12 The aim of vaginal stretching (VS), myofascial release, proprioceptive neuromuscular facilitation, and massage therapy is to increase flexibility, release muscle tension and trigger points in PFM.6,11,12 Photobiomodulation therapy (PBMT) is another therapeutic possibility that has already been studied for MP in muscles other than the PFM. It was previously studied for treatment of vestibulodynia (PBMT). PBMT uses laser devices or LEDs (Light-Emitting Diodes) without thermal effects.13 Light absorption in biological tissue can promote analgesia, caused by delay or nerve conduction block of stimuli in central and peripheral nerve fibers, increasing the production of endogenous opioid neurotransmitters, and also local blood circulation.14,15 Few studies have evaluated the effect of VS on PF disorders. Furthermore, there are no specific studies that assess the effect of PBMT on PFMP and sexual function. Our hypothesis is that VS combined with PBMT in PFM would further decrease the complaint of painful intercourse and lead to an improved sexual function in women with MP. The aim of this study was to compare the effect of vaginal stretching (VS) with photobiomodulation therapy (PBMT) and VS with sham PBMT on overall sexual function, rate, and severity of pain during intercourse in women with PFMP, at baseline and following treatment.
METHODS
Trial Design
This is a double-blind, parallel, randomized clinical trial, conducted at the Department of Obstetrics and Gynecology School of Medical Sciences, University of Campinas, Campinas, SP, Brazil, from December 2018 to September 2020. The study was approved by the local institutional ethics committee of the State University of Campinas (CAAE: 92766318.4.0000.5404) and was registered in the REBEC (Registro Brasileiro de Ensaios Clínicos; Brazilian Registry of Clinical Trials) under N. RBR-2TDCQ4. All subjects gave their written informed consent before study entry. The study followed the Consort reporting guidelines.16
Participants
We included women over 18 years of age with MP. On unidigital palpation of the PFM, MP was diagnosed by the presence of any level of pain elicited by increasing pressure in the opposite direction to muscle contraction.17 We excluded women reporting signs and symptoms of active urinary tract infection, pelvic inflammatory disease, and history of gynecological cancer, pelvic radiotherapy or brachytherapy, pregnant women, use of analgesic medications, narcotics, and muscle relaxants.
Procedures
Women were randomized (1:1) to a vaginal stretching (VS) with PBMT group or a VS with sham PBMT group. The VS with PBMT group underwent vaginal stretching and low-level laser treatment. The VS with sham PBMT group underwent vaginal stretching with sham low-level laser treatment. Treatment consisted of 10 sessions (twice a week). Follow-up was conducted in all women 1 week after the last treatment session.
VS With PBMT Group
The VS with PBMT group underwent passive vaginal stretching of the pelvic floor muscle, with 40 seconds of sustained digital pressure applied in the opposite direction to muscle contraction (posterior - inferior) in each of the 3 muscle points treated (at 4, 6 and 8-o’clock positions on the analogue vaginal clock), followed by the application of near infrared light at the same 3 points. The PBMT device used was a low-level laser device (Model Therapy EC, DMC, São Carlos, Brazil, produced in 2018). Two GaAlAs Fiber Optic Emitters (Figure 1) were used, which have a thin metallic tip of 7.5 cm in length and 3mm in diameter, emitting red (660nm) and near infrared light (NIR) (808nm), 100 mW power. The tip was protected with an unlubricated condom which was inserted into the vaginal canal 4–5 cm deep, a site approximated by the puborectalis and pubovisceral muscle bundles, located at the 4, 6 and 8-o’clock positions. NIR light was used with 4 joules of energy applied per point, which requires 40 seconds of perpendicular positioning in contact with the vaginal mucosa at each treated point. The irradiance level at the target area was 3.571mW/cm2, the dose per point was 143J/cm2, total energy per session was 12J, and at the spot area was 0.028 cm2.
VS With Sham PBMT Group
The VS with sham PBMT group underwent the same vaginal stretching protocol, followed by vaginal introduction of the laser device which was switched off (sham). No light was emitted and the device was simply positioned into the vaginal canal for 40 seconds each at the same 3 points. Every 10 seconds the researcher pressed a beep on the equipment to simulate application.
Outcomes
Primary outcome was overall sexual function after treatment of PFMP evaluated by FSFI. Participants completed the self-reported FSFI questionnaire,18 validated in Portuguese,19,20 FSFI questionnaire assessed sexual function in the last 4 weeks. The 19 items of the FSFI is categorized into 6 domains of female sexual function: desire, arousal, lubrication, orgasm, satisfaction, and pain (during vaginal penetration). Each item uses a 5-point Likert scale ranging 0 (or 1) -5 with higher scores indicating greater levels of sexual functioning on the respective item. The FSFI total score is the sum of the 6 domain/subscale and the total scale range of 2–36, with higher scores indicating greater overall sexual function.18 In the FSFI total score that measures overall sexual function, a cut-off score of 26.55 or below may determine women that may have sexual dysfunction.21 Secondary outcome was to assess the rate and severity of pain during intercourse by the following question: “Do you have a complaint of persistent or recurrent pain or discomfort associated with attempted or complete vaginal penetration?”6 For women with complaints of painful intercourse, pain intensity was measured by Visual Analog Scale (VAS) pain score (ranging from 0–10; 0 = no pain; 10 = extreme pain).
Randomization
The randomization sequence list was generated by a computer program (Uniform probability distribution function from Data Procedure - software SAS version 9.4), using a permuted block size of 10. Information on the treatment to be used was kept inside a sealed opaque envelope, identified by a number. Random allocation sequence was organized by a single researcher who was responsible for concealing allocation and was not involved in patient recruitment. This researcher assigned participants to the intervention group and applied the treatment. Another physiotherapist was blinded to the intervention group and performed the initial and post-treatment evaluation. The patients were blinded to the treatment group.
Statistical Section
A method to compare the means between 2 groups was used to calculate sample size. We considered the mean and standard deviation of the pre and post FSFI total score, according to Zoorob et al.4 Type 1 error rate or alpha significance level was 5% (alpha = 0.05) (or 95% confidence interval) and sampling power was 80%. According to the results, the minimum sample was 42 women. We added 30% of loss to follow- up, totaling 56 women (28 per group).
Intention-to-treat analysis (ITT) was carried out with the statistical approach Last Observation Carried Forward (LOCF). To compare the presence or absence of painful intercourse and sexual dysfunction (FSFI total score ≤26.55) between 2 groups, the Chi-square or Fisher’s exact tests were used (for expected values lower than 5). To compare painful intercourse and sexual dysfunction (categorical variables) before and after treatment, the McNemar test (2 categories) and Bowker Symmetry test (3 or more categories) for related samples were used. To compare pain during intercourse by VAS pain score and FSFI domain score between both groups, the Mann-Whitney test (2 groups) was used, due to the lack of normal distribution of the variables. Analysis of variance for repeated measures (ANOVA for repeated measures) with the variables transformed into ranks due to absence of normal distribution was used to compare painful intercourse scores and FSFI domains (numerical variables) between both groups (the VS with PBMT group in comparison to the VS with sham PBMT group) and between time periods (before and after intervention) and estimation of group vs time interaction effect. Analysis adjusted to menopausal status was conducted by multiple logistic regression analysis and analysis of covariance for repeated measures (ANCOVA for repeated measures) with variables transformed into ranks due to the lack of normal distribution. The significance level was 5%.
RESULTS
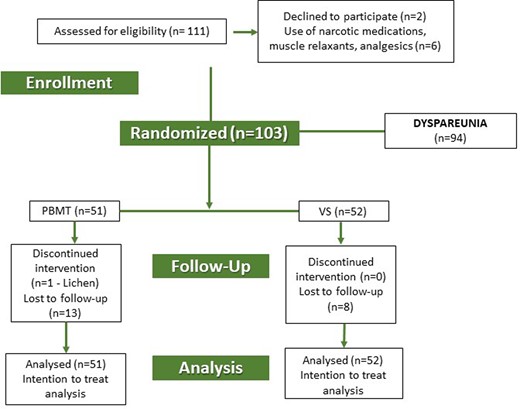
Of the 103 women included in the study, 51 were randomized to the VS with PBMT group and 52 to the VS with sham PBMT group. The participant flow chart is shown in Figure 2. A total of 37 (VS with PBMT group) and 44 women (VS with sham PBMT group) completed 10 treatment sessions. The sociodemographic characteristics of the participants are shown in Table 1 .
Sociodemographic and clinical characteristics of women with myofascial dysfunction in the pelvic floor muscles, according to vaginal stretching with photobiomodulation and vaginal stretching with sham photobiomodulation groups
| Characteristics . | VS with PBMT (n = 51) . | VS with sham PBMT (n = 52) . | P value . |
|---|---|---|---|
| Age (y) (mean ± SD) | 40 ± 15.0 | 45 ± 13.9 | .08* |
| Race White (n/%) | 38 / 74.5 | 35 / 67.3 | .42† |
| Education > 8 y (n/%) | 42 / 82.3 | 45 / 86.5 | .55† |
| Partnered (n/%) | 30 / 58.8 | 35 / 67.3 | .37† |
| Parity (mean ± SD) | 1.86 ± 1.9 | 1.62 ± 1.6 | .61* |
| Menopause (n/%) | 14 / 27.5 | 26 / 50.0 | .019† |
| Contraceptive method (n = 63) (n/%) | |||
| Hormonal | 22 / 59.5 | 13 / 50.0 | .75† |
| Non-hormonal | 7 / 18.9 | 6 / 23.1 | |
| None | 8 / 21.6 | 7 / 26.9 | |
| Hormone Therapy (n = 40) (n/%) | |||
| None | 11 / 78.6 | 19 / 73.1 | .87‡ |
| Topic | 2 / 14.3 | 3 / 15.4 | |
| Systemic | 1 / 7.1 | 4 / 11.5 |
| Characteristics . | VS with PBMT (n = 51) . | VS with sham PBMT (n = 52) . | P value . |
|---|---|---|---|
| Age (y) (mean ± SD) | 40 ± 15.0 | 45 ± 13.9 | .08* |
| Race White (n/%) | 38 / 74.5 | 35 / 67.3 | .42† |
| Education > 8 y (n/%) | 42 / 82.3 | 45 / 86.5 | .55† |
| Partnered (n/%) | 30 / 58.8 | 35 / 67.3 | .37† |
| Parity (mean ± SD) | 1.86 ± 1.9 | 1.62 ± 1.6 | .61* |
| Menopause (n/%) | 14 / 27.5 | 26 / 50.0 | .019† |
| Contraceptive method (n = 63) (n/%) | |||
| Hormonal | 22 / 59.5 | 13 / 50.0 | .75† |
| Non-hormonal | 7 / 18.9 | 6 / 23.1 | |
| None | 8 / 21.6 | 7 / 26.9 | |
| Hormone Therapy (n = 40) (n/%) | |||
| None | 11 / 78.6 | 19 / 73.1 | .87‡ |
| Topic | 2 / 14.3 | 3 / 15.4 | |
| Systemic | 1 / 7.1 | 4 / 11.5 |
Mann-Whitney test.
Chi-square test.
Fisher’s exact test.
SD = standard deviation.
Sociodemographic and clinical characteristics of women with myofascial dysfunction in the pelvic floor muscles, according to vaginal stretching with photobiomodulation and vaginal stretching with sham photobiomodulation groups
| Characteristics . | VS with PBMT (n = 51) . | VS with sham PBMT (n = 52) . | P value . |
|---|---|---|---|
| Age (y) (mean ± SD) | 40 ± 15.0 | 45 ± 13.9 | .08* |
| Race White (n/%) | 38 / 74.5 | 35 / 67.3 | .42† |
| Education > 8 y (n/%) | 42 / 82.3 | 45 / 86.5 | .55† |
| Partnered (n/%) | 30 / 58.8 | 35 / 67.3 | .37† |
| Parity (mean ± SD) | 1.86 ± 1.9 | 1.62 ± 1.6 | .61* |
| Menopause (n/%) | 14 / 27.5 | 26 / 50.0 | .019† |
| Contraceptive method (n = 63) (n/%) | |||
| Hormonal | 22 / 59.5 | 13 / 50.0 | .75† |
| Non-hormonal | 7 / 18.9 | 6 / 23.1 | |
| None | 8 / 21.6 | 7 / 26.9 | |
| Hormone Therapy (n = 40) (n/%) | |||
| None | 11 / 78.6 | 19 / 73.1 | .87‡ |
| Topic | 2 / 14.3 | 3 / 15.4 | |
| Systemic | 1 / 7.1 | 4 / 11.5 |
| Characteristics . | VS with PBMT (n = 51) . | VS with sham PBMT (n = 52) . | P value . |
|---|---|---|---|
| Age (y) (mean ± SD) | 40 ± 15.0 | 45 ± 13.9 | .08* |
| Race White (n/%) | 38 / 74.5 | 35 / 67.3 | .42† |
| Education > 8 y (n/%) | 42 / 82.3 | 45 / 86.5 | .55† |
| Partnered (n/%) | 30 / 58.8 | 35 / 67.3 | .37† |
| Parity (mean ± SD) | 1.86 ± 1.9 | 1.62 ± 1.6 | .61* |
| Menopause (n/%) | 14 / 27.5 | 26 / 50.0 | .019† |
| Contraceptive method (n = 63) (n/%) | |||
| Hormonal | 22 / 59.5 | 13 / 50.0 | .75† |
| Non-hormonal | 7 / 18.9 | 6 / 23.1 | |
| None | 8 / 21.6 | 7 / 26.9 | |
| Hormone Therapy (n = 40) (n/%) | |||
| None | 11 / 78.6 | 19 / 73.1 | .87‡ |
| Topic | 2 / 14.3 | 3 / 15.4 | |
| Systemic | 1 / 7.1 | 4 / 11.5 |
Mann-Whitney test.
Chi-square test.
Fisher’s exact test.
SD = standard deviation.
The mean age of the participants was 43 ± 14.5 years. The majority of these women were married or partnered (63%), with no difference between groups, and were mostly white, without any difference between groups (P = .42). Most participants allocated to the VS with PBMT group were not in the menopause (73%; P = .019).
Of the 103 women, 91 (88.4%) had painful intercourse: 46/51 (90.2%) and 45/52 (86.6 %) reported pain during intercourse in the VS with PBTM group and in the VS with sham PBMT group, respectively, without any difference between groups (P = .75). After treating both groups, a significant reduction was observed in the number of women who complained of painful intercourse, with no difference between treatment groups (P = .83) (Table 2).
Distribution of women with myofascial dysfunction according to presence of painful intercourse and sexual dysfunction and type of treatment and adjusted for menopausal status
| Characteristics . | Total (n = 103) . | VS with PBMT (n = 51) . | P1 . | VS with sham PBMT (n = 52) . | P1 . | P2 . | P3 . | ||
|---|---|---|---|---|---|---|---|---|---|
| . | n (%) . | Before n (%) . | After n (%) . | . | Before n (%) . | After n (%) . | . | . | . |
| Sexual dysfunction* Yes No | 94 (91.3) | 47 (92.2) | 38 (74.5) | P = .003§ | 47 (90.4) | 40 (76.9) | P = .035§ | P = .56‡ | P = .90‡ |
| 9 (8.8) | 4 (7.8) | 13 (25.5) | 5 (9.6) | 12 (23.1) | |||||
| Painful intercourse Yes No No sexual activity | 91 (88.4) | 46 (90.2) | 28 (55.0) | P = .001† | 45 (86.6) | 24 (46.2) | P < .001† | P = 0.75‡ | P = 0.83‡ |
| 3 (2.9) 9 (8.7) | 1 (2.0) 4 (7.8) | 21 (41.2) 2 (3.8) | 2 (3.8) 5 (9.6) | 24 (46.2) 4 (7.6) | |||||
| Characteristics . | Total (n = 103) . | VS with PBMT (n = 51) . | P1 . | VS with sham PBMT (n = 52) . | P1 . | P2 . | P3 . | ||
|---|---|---|---|---|---|---|---|---|---|
| . | n (%) . | Before n (%) . | After n (%) . | . | Before n (%) . | After n (%) . | . | . | . |
| Sexual dysfunction* Yes No | 94 (91.3) | 47 (92.2) | 38 (74.5) | P = .003§ | 47 (90.4) | 40 (76.9) | P = .035§ | P = .56‡ | P = .90‡ |
| 9 (8.8) | 4 (7.8) | 13 (25.5) | 5 (9.6) | 12 (23.1) | |||||
| Painful intercourse Yes No No sexual activity | 91 (88.4) | 46 (90.2) | 28 (55.0) | P = .001† | 45 (86.6) | 24 (46.2) | P < .001† | P = 0.75‡ | P = 0.83‡ |
| 3 (2.9) 9 (8.7) | 1 (2.0) 4 (7.8) | 21 (41.2) 2 (3.8) | 2 (3.8) 5 (9.6) | 24 (46.2) 4 (7.6) | |||||
Sexual Dysfunction FSFI ≤26.55.
Symmetry Test.
Multiple logistic regression analysis adjusted for menopausal status.
McNemar Test.
P1 – Intra-group comparison before vs after; P2 – inter-group comparison before treatment; P3 – inter-group comparison after treatment.
Distribution of women with myofascial dysfunction according to presence of painful intercourse and sexual dysfunction and type of treatment and adjusted for menopausal status
| Characteristics . | Total (n = 103) . | VS with PBMT (n = 51) . | P1 . | VS with sham PBMT (n = 52) . | P1 . | P2 . | P3 . | ||
|---|---|---|---|---|---|---|---|---|---|
| . | n (%) . | Before n (%) . | After n (%) . | . | Before n (%) . | After n (%) . | . | . | . |
| Sexual dysfunction* Yes No | 94 (91.3) | 47 (92.2) | 38 (74.5) | P = .003§ | 47 (90.4) | 40 (76.9) | P = .035§ | P = .56‡ | P = .90‡ |
| 9 (8.8) | 4 (7.8) | 13 (25.5) | 5 (9.6) | 12 (23.1) | |||||
| Painful intercourse Yes No No sexual activity | 91 (88.4) | 46 (90.2) | 28 (55.0) | P = .001† | 45 (86.6) | 24 (46.2) | P < .001† | P = 0.75‡ | P = 0.83‡ |
| 3 (2.9) 9 (8.7) | 1 (2.0) 4 (7.8) | 21 (41.2) 2 (3.8) | 2 (3.8) 5 (9.6) | 24 (46.2) 4 (7.6) | |||||
| Characteristics . | Total (n = 103) . | VS with PBMT (n = 51) . | P1 . | VS with sham PBMT (n = 52) . | P1 . | P2 . | P3 . | ||
|---|---|---|---|---|---|---|---|---|---|
| . | n (%) . | Before n (%) . | After n (%) . | . | Before n (%) . | After n (%) . | . | . | . |
| Sexual dysfunction* Yes No | 94 (91.3) | 47 (92.2) | 38 (74.5) | P = .003§ | 47 (90.4) | 40 (76.9) | P = .035§ | P = .56‡ | P = .90‡ |
| 9 (8.8) | 4 (7.8) | 13 (25.5) | 5 (9.6) | 12 (23.1) | |||||
| Painful intercourse Yes No No sexual activity | 91 (88.4) | 46 (90.2) | 28 (55.0) | P = .001† | 45 (86.6) | 24 (46.2) | P < .001† | P = 0.75‡ | P = 0.83‡ |
| 3 (2.9) 9 (8.7) | 1 (2.0) 4 (7.8) | 21 (41.2) 2 (3.8) | 2 (3.8) 5 (9.6) | 24 (46.2) 4 (7.6) | |||||
Sexual Dysfunction FSFI ≤26.55.
Symmetry Test.
Multiple logistic regression analysis adjusted for menopausal status.
McNemar Test.
P1 – Intra-group comparison before vs after; P2 – inter-group comparison before treatment; P3 – inter-group comparison after treatment.
Pain reported during intercourse was measured by the VAS. Before treatment, the average level of pain reported was 7.3, with no difference between groups (P = .97). A significant decrease in pain intensity during intercourse was observed in the VS with PBMT group (7.2 ± 2.2 to 6.0 ± 2.4) and in the VS with sham PBMT group (7.4 ± 2.0 to 5.8 ± 2.5) (P = .002 and P < .001, respectively) with no difference between them (P = .87) after treatment (Table 3).
Painful intercourse scores and FSFI scores in the women with myofascial dysfunction according to vaginal stretching with photobiomodulation or vaginal stretching with sham photobiomodulation groups and adjusted for menopausal status
| Characteristics . | Total (n = 103) . | (n = 51) . | VS with sham PBMT (n = 52) . | P group . | P time . | P interaction . | ||
|---|---|---|---|---|---|---|---|---|
| Before . | After . | Before . | After . | |||||
| . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | . | . | . |
| FSFI Desire | 2.7 ± 1.2 | 2.9 ± 1.2 | 3.2 ± 1.2 | 2.5 ± 1.2 | 3.1 ± 1.4 | P = .91 | P < .001† | P = .10 |
| FSFI Arousal | 2.7 ± 1.7 | 2.8 ± 1.6 | 3.1 ± 1.7 | 2.7 ± 1.8 | 2.9 ± 1.9 | P = .67 | P = .054 | P = .58 |
| FSFI Lubrication | 3.0 ± 1.9 | 3.1 ± 1.9 | 3.4 ± 1.9 | 2.9 ± 1.9 | 2.9 ± 2.1 | P = .98 | P = .15 | P = .41 |
| FSFI Orgasm | 2.9 ± 2.0 | 3.0 ± 2.0 | 2.9 ± 2.1 | 2.7 ± 2.0 | 2.8 ± 2.3 | P = .92 | P = .86 | P = .56 |
| FSFI Satisfaction | 3.3 ± 1.6 | 3.5 ± 1.4 | 3.7 ± 1.7 | 3.0 ± 1.8 | 3.4 ± 1.8 | P = .53 | P = .11 | P = .56 |
| FSFI Pain | 1.8 ± 1.4 | 1.7 ± 1.3 | 2.3 ± 2.0 | 1.8 ± 1.6 | 2.6 ± 2.2 | P = .30 | P = .002‡ | P = .29 |
| FSFI total | 16.4 ± 8.1 | 17.1 ± 7.7 | 18.6 ± 8.8 | 15.6 ± 8.6 | 17.7 ± 9.8 | P = .98 | P = .009§ | P = .65 |
| Painful intercourse (VAS) (n = 91) | 7.3 ± 2.0 | 7.2 ± 2.2 | 6.0 ± 2.4 | 7.4 ± 2.0 | 5.8 ± 2.5 | P = .97 | P < .001* | P = .87 |
| Characteristics . | Total (n = 103) . | (n = 51) . | VS with sham PBMT (n = 52) . | P group . | P time . | P interaction . | ||
|---|---|---|---|---|---|---|---|---|
| Before . | After . | Before . | After . | |||||
| . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | . | . | . |
| FSFI Desire | 2.7 ± 1.2 | 2.9 ± 1.2 | 3.2 ± 1.2 | 2.5 ± 1.2 | 3.1 ± 1.4 | P = .91 | P < .001† | P = .10 |
| FSFI Arousal | 2.7 ± 1.7 | 2.8 ± 1.6 | 3.1 ± 1.7 | 2.7 ± 1.8 | 2.9 ± 1.9 | P = .67 | P = .054 | P = .58 |
| FSFI Lubrication | 3.0 ± 1.9 | 3.1 ± 1.9 | 3.4 ± 1.9 | 2.9 ± 1.9 | 2.9 ± 2.1 | P = .98 | P = .15 | P = .41 |
| FSFI Orgasm | 2.9 ± 2.0 | 3.0 ± 2.0 | 2.9 ± 2.1 | 2.7 ± 2.0 | 2.8 ± 2.3 | P = .92 | P = .86 | P = .56 |
| FSFI Satisfaction | 3.3 ± 1.6 | 3.5 ± 1.4 | 3.7 ± 1.7 | 3.0 ± 1.8 | 3.4 ± 1.8 | P = .53 | P = .11 | P = .56 |
| FSFI Pain | 1.8 ± 1.4 | 1.7 ± 1.3 | 2.3 ± 2.0 | 1.8 ± 1.6 | 2.6 ± 2.2 | P = .30 | P = .002‡ | P = .29 |
| FSFI total | 16.4 ± 8.1 | 17.1 ± 7.7 | 18.6 ± 8.8 | 15.6 ± 8.6 | 17.7 ± 9.8 | P = .98 | P = .009§ | P = .65 |
| Painful intercourse (VAS) (n = 91) | 7.3 ± 2.0 | 7.2 ± 2.2 | 6.0 ± 2.4 | 7.4 ± 2.0 | 5.8 ± 2.5 | P = .97 | P < .001* | P = .87 |
Significant differences between times (contrast profile test): VS with PBMT group (P = .002; Before vs After); VS with sham PBMT group (P < .001; Before vs After).
Significant differences between times (contrast profile test): VS with PBMT group (P = .128; Before vs After); VS with sham PBMT group (P < .001; Before vs After).
Significant differences between times (contrast profile test): VS with PBMT group (P = .038; Before vs After); VS with sham PBMT group (P = .005; Before vs After).
Significant differences between times (contrast profile test): VS with PBMT group (P = .108; Before vs After); VS with sham PBMT group (P = .024; Before vs After).
FSFI = Female Sexual function Index; SD = standard deviation; VAS = visual analogic scale.
Analysis of covariance for repeated measures (ANCOVA for repeated measures) on rank transformed variables; PGroup: Group effect or between groups comparison; PTime: Time effect or within groups comparison; PInteraction: Group vs Time interaction effect.
Painful intercourse scores and FSFI scores in the women with myofascial dysfunction according to vaginal stretching with photobiomodulation or vaginal stretching with sham photobiomodulation groups and adjusted for menopausal status
| Characteristics . | Total (n = 103) . | (n = 51) . | VS with sham PBMT (n = 52) . | P group . | P time . | P interaction . | ||
|---|---|---|---|---|---|---|---|---|
| Before . | After . | Before . | After . | |||||
| . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | . | . | . |
| FSFI Desire | 2.7 ± 1.2 | 2.9 ± 1.2 | 3.2 ± 1.2 | 2.5 ± 1.2 | 3.1 ± 1.4 | P = .91 | P < .001† | P = .10 |
| FSFI Arousal | 2.7 ± 1.7 | 2.8 ± 1.6 | 3.1 ± 1.7 | 2.7 ± 1.8 | 2.9 ± 1.9 | P = .67 | P = .054 | P = .58 |
| FSFI Lubrication | 3.0 ± 1.9 | 3.1 ± 1.9 | 3.4 ± 1.9 | 2.9 ± 1.9 | 2.9 ± 2.1 | P = .98 | P = .15 | P = .41 |
| FSFI Orgasm | 2.9 ± 2.0 | 3.0 ± 2.0 | 2.9 ± 2.1 | 2.7 ± 2.0 | 2.8 ± 2.3 | P = .92 | P = .86 | P = .56 |
| FSFI Satisfaction | 3.3 ± 1.6 | 3.5 ± 1.4 | 3.7 ± 1.7 | 3.0 ± 1.8 | 3.4 ± 1.8 | P = .53 | P = .11 | P = .56 |
| FSFI Pain | 1.8 ± 1.4 | 1.7 ± 1.3 | 2.3 ± 2.0 | 1.8 ± 1.6 | 2.6 ± 2.2 | P = .30 | P = .002‡ | P = .29 |
| FSFI total | 16.4 ± 8.1 | 17.1 ± 7.7 | 18.6 ± 8.8 | 15.6 ± 8.6 | 17.7 ± 9.8 | P = .98 | P = .009§ | P = .65 |
| Painful intercourse (VAS) (n = 91) | 7.3 ± 2.0 | 7.2 ± 2.2 | 6.0 ± 2.4 | 7.4 ± 2.0 | 5.8 ± 2.5 | P = .97 | P < .001* | P = .87 |
| Characteristics . | Total (n = 103) . | (n = 51) . | VS with sham PBMT (n = 52) . | P group . | P time . | P interaction . | ||
|---|---|---|---|---|---|---|---|---|
| Before . | After . | Before . | After . | |||||
| . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | (Mean ± SD) . | . | . | . |
| FSFI Desire | 2.7 ± 1.2 | 2.9 ± 1.2 | 3.2 ± 1.2 | 2.5 ± 1.2 | 3.1 ± 1.4 | P = .91 | P < .001† | P = .10 |
| FSFI Arousal | 2.7 ± 1.7 | 2.8 ± 1.6 | 3.1 ± 1.7 | 2.7 ± 1.8 | 2.9 ± 1.9 | P = .67 | P = .054 | P = .58 |
| FSFI Lubrication | 3.0 ± 1.9 | 3.1 ± 1.9 | 3.4 ± 1.9 | 2.9 ± 1.9 | 2.9 ± 2.1 | P = .98 | P = .15 | P = .41 |
| FSFI Orgasm | 2.9 ± 2.0 | 3.0 ± 2.0 | 2.9 ± 2.1 | 2.7 ± 2.0 | 2.8 ± 2.3 | P = .92 | P = .86 | P = .56 |
| FSFI Satisfaction | 3.3 ± 1.6 | 3.5 ± 1.4 | 3.7 ± 1.7 | 3.0 ± 1.8 | 3.4 ± 1.8 | P = .53 | P = .11 | P = .56 |
| FSFI Pain | 1.8 ± 1.4 | 1.7 ± 1.3 | 2.3 ± 2.0 | 1.8 ± 1.6 | 2.6 ± 2.2 | P = .30 | P = .002‡ | P = .29 |
| FSFI total | 16.4 ± 8.1 | 17.1 ± 7.7 | 18.6 ± 8.8 | 15.6 ± 8.6 | 17.7 ± 9.8 | P = .98 | P = .009§ | P = .65 |
| Painful intercourse (VAS) (n = 91) | 7.3 ± 2.0 | 7.2 ± 2.2 | 6.0 ± 2.4 | 7.4 ± 2.0 | 5.8 ± 2.5 | P = .97 | P < .001* | P = .87 |
Significant differences between times (contrast profile test): VS with PBMT group (P = .002; Before vs After); VS with sham PBMT group (P < .001; Before vs After).
Significant differences between times (contrast profile test): VS with PBMT group (P = .128; Before vs After); VS with sham PBMT group (P < .001; Before vs After).
Significant differences between times (contrast profile test): VS with PBMT group (P = .038; Before vs After); VS with sham PBMT group (P = .005; Before vs After).
Significant differences between times (contrast profile test): VS with PBMT group (P = .108; Before vs After); VS with sham PBMT group (P = .024; Before vs After).
FSFI = Female Sexual function Index; SD = standard deviation; VAS = visual analogic scale.
Analysis of covariance for repeated measures (ANCOVA for repeated measures) on rank transformed variables; PGroup: Group effect or between groups comparison; PTime: Time effect or within groups comparison; PInteraction: Group vs Time interaction effect.
Before treatment, most participants (94/103, 91.3%) had sexual dysfunction assessed by the categorized FSFI total score questionnaire. After treatment in both groups, there was a significant reduction in sexual dysfunction and an increase in overall sexual function. In the VS with PBMT group, 47 (92.2 %) and 38 (74.5 %) women had sexual dysfunction before and after treatment, respectively (P = .003). Furthermore, in the VS with sham PBMT group, 47 (90.4%) and 40 (76.9%) women had sexual dysfunction before and after treatment (P = .035), without any difference between groups (P = .56 before, P = .90 after) (Table 2).
Table 3 shows total FSFI and its domains. After treatment, there was significant improvement in overall sexual function scores only in the VS with sham PBMT group (15.6–17.7, P = .024). Regarding sexual function domains, before treatment there was no difference between the VS with PBMT group and the VS with sham PBMT group. After treatment, there was a significant improvement in sexual desire (2.5–3.1, P < .001) only in the VS with sham PBMT group. The intensity of painful intercourse decreased significantly, as reflected by a significant reduction in FSFI pain domain scores after treatment in both groups (P < .001, [VS with PBMT group: P = .038; VS with sham PBMT group: P = .005]).
DISCUSSION
Our findings showed that women with MP have high rates of painful intercourse and sexual dysfunction. Vaginal stretching may have efficacy in reducing the rates of women with painful intercourse and sexual dysfunction, in addition to improving the severity of painful intercourse. However, the combination of PBMT and VS did not show any additional benefit. Furthermore, both groups showed reduction in pain with intercourse assessed by the FSFI and women treated only with VS had an increase in sexual desire and overall sexual function.
MP is associated with 1 or more pelvic floor muscles changes, such as the inability to relax when necessary and increased muscle activity2. The PFM are slightly stretched and widened to allow vaginal penetration.22 Therefore, excessively taut pelvic muscles can hamper vaginal penetration, as occurs in women with vaginismus, leading to painful intercourse.1,23,24 In the current study, 90% of women with MP had painful intercourse. Nevertheless, in this study it was demonstrated that treatment of muscle tightness, using passive vaginal stretching with or without PMBT, may have efficacy at lowering the number of women with this complaint and decreasing pain severity scores.
There is a paucity of studies in the literature on PFMP treatment. However, our study is in agreement with articles indicating the effectiveness of VS in MP treatment.25–27 Since MP may feature central sensitization,11,28 we hypothesized that the use of PBMT, in combination with VS, would provide greater pain relief during intercourse. However, this was not observed in the current study, which agrees with the findings of another study using PBMT to reduce vulvar vestibular pain in women with provoked vestibulodynia.13 One reason for this finding could be the PBMT dosage. Since this is an innovative method, the dosage required to benefit the pelvic muscles has still not been well-established.
In agreement with other studies1,4 this study revealed a high prevalence of sexual dysfunction in PFMP dysfunction. After both treatments, the number of women with sexual dysfunction decreased significantly. A similar and significant reduction in FSFI pain score was observed in the VS with PBMT group and in the VS with sham PBMT group. It was shown that PBMT did not exert any additional effect on pain reduction. The use of VS was concordant with other studies that used stretching techniques for treatment, such as the modified Thiele massage or compression maneuver.4,26,29
Regardless of the results from other FSFI pain domains, only the VS with sham PBMT group had a significant improvement in the desire domain and total FSFI score. Sexual desire is one of the subjective stages of female sexual function. Reasons that motivate a woman to engage in sexual behavior include emotional closeness to her partner and her own sense of well-being.30 In the current study, pain alleviation during intercourse may have decreased the feeling of anxiety or guilt about sexual infrequency, which can contribute to increased sexual desire. In another study,4 the authors used stretching and compression maneuvers for treatment, finding no increase in the FSFI desire score after 4 sessions per week. Despite the similarity of techniques, those results do not corroborate our study.
In our study we found no difference in the result of the other FSFI domains, such as arousal, lubrication, orgasm, and satisfaction after both types of treatment. 1 study26 evaluated the effect of an intravaginal massage technique in women who had painful intercourse associated with tenderness of the PFM. Those authors observed improvement in all FSFI domains after 4 weeks of treatment, which differs from this study.
One of the strengths of our study is that it is a randomized, double-blind study. To the best of our knowledge, it is the first study to use a combination of VS and PBMT for MP in PFM. In addition, validated techniques were used for data analysis: VAS and a specific validated instrument for sexual function. The study also has limitations. Our study design did not include a usual care control group which may have hampered the determination of efficacy. Also, we did not have an PBMT group only which prevents us from examining the efficacy of this therapy. This was a double-blind study where 1 researcher, in charge of the initial and final assessments, did not know which interventions the participants were receiving, while the participants did not know to which treatment group they have been assigned. However, the other researcher who was responsible for applying the treatments, could not be blinded to the interventions, which was also a study limitation. In addition, loss to follow-up and a short follow-up period occurred, and the duration of effects could not be established. The diagnostic method chosen for MP was painful vaginal palpation. Despite its widespread use, it is a subjective and non-standardized method. New studies with different PBMT dosimetry parameters, such as higher energy per point, or even different wavelengths of light must be carried out to evaluate the effect of this therapy on PFMP.
CONCLUSION
High rates of painful intercourse and sexual dysfunction occurred in women with PFMP. VS only and VS with PBMT may have short-term efficacy in reducing painful intercourse, decreasing the severity of this symptom and reducing the number of women with sexual dysfunction assessed by a validated questionnaire.
STATEMENT OF AUTHORSHIP
Claudia Pignatti Frederice Teixeira: Writing - Original Draft, Formal Analysis, Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Project Administration; Ticiana Aparecida Alves de Mira: Methodology, Writing - Review & Editing; Helymar da Costa Machado: statistical analysis, Writing - Review & Editing; Luiz Gustavo de Oliveira Brito: Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing; Cassia Raquel Teatin Juliato: Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing.
Funding
None.
REFERENCES
Author notes
Conflict of Interest: The authors report no conflicts of interest.



