-
PDF
- Split View
-
Views
-
Cite
Cite
Ameen S Aldahar, Abdullah Zakaria Al-Dhayan, Raed N Alghamdi, Raneem Abdullah Alrouji, Ali Albargawi, Rakan Mounla Ali, Symptomatic pleural lipoma: a case report from Saudi Arabia, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf310, https://doi.org/10.1093/jscr/rjaf310
Close - Share Icon Share
Abstract
Pleural lipomas are rare, benign, slow-growing tumors composed of fat cells. This case report highlights a symptomatic pleural lipoma, adding to the limited surgical literature on this condition. A 56-year-old female presented with intermittent left pleuritic chest pain. Imaging revealed a benign left pleural lipoma without effusion or pleural thickening. The patient underwent video-assisted thoracoscopy surgery (VATS) for resection of the lipoma. Postoperative recovery was uneventful, with complete resolution of symptoms. Pleural lipomas are rare, benign, slow-growing tumors that are usually asymptomatic. Symptomatic cases should be managed with surgical resection via VATS for optimal outcomes.
Introduction
Lipomas are considered common benign tumors of the skin and subcutaneous tissue. They occur with an annual incidence of 1 per 1000 people [1]. Most lipomas are found in the subcutaneous tissue, and they can be found in various places in the human body; however, their presence throughout the thoracic pleura is extremely rare [2]. A pleural lipoma is a benign, slow-growing tumor composed of fat cells that develop on the pleura, usually found at the mediastinal, bronchial, and pulmonary levels. In addition, pleural lipomas are considered slowly developing tumor as most patients often remain asymptomatic. Pleural lipomas are typically asymptomatic and often discovered incidentally during chest radiographs or computed tomography (CT) examinations [3, 4]. CT scans are the preferred modality for diagnosing pleural lipomas, revealing well-defined nodules with homogeneous fat attenuation of approximately −50 to −150 Hounsfield units [5]. In our case, CT scan was descriptive to left small pleural lipoma and histopathology revealed lipomas which clinched the diagnosis. Although pleural lipoma is considered benign tumor and usually asymptomatic however, when it is symptomatic, it may cause compressive symptoms such as nonproductive cough, chest pain, and dyspnea if they reach adequate size that may cause compressive effect. Surgery is indicated for symptomatic ones to be completely resected via open or video-assisted thoracoscopy surgery (VATS) as it has good outcomes for diagnostic and therapeutic purposes for those with symptomatic pleural lipoma [1].
This case report has been prepared in accordance with the updated Surgical Case Report (SCARE) 2023 guidelines, ensuring the study adheres to established standards for the publication of surgical case reports. The SCARE criteria provide a comprehensive framework for reporting clinical case details and outcomes to enhance transparency and reproducibility in surgical literature [6].
Case presentation
This is a 56-year-old female referred to our clinic with on-and-off left pleuritic chest pain since 3 months. Her past medical history was significant for hypothyroidism and dyslipidaemia. Upon presentation, she was conscious, alert, oriented, with normal vital signs, not in respiratory distress. Her laboratory workup unremarkable, chest X-ray was unremarkable for any abnormality, and computed tomography scan of the chest with IV contrast (Fig. 1) showed features suggestive of benign left pleural lipoma with no effusion or pleural thickening. Preoperative tests were done, the patient underwent surgical resection via VATS by a 10-year expert consultant. The operation was done uneventfully and specimen was sent to laboratory that revealed the diagnosis of pleural lipoma (Fig. 2). Patient postoperative period was uneventful, discharged after surgery and followed up in clinic for 1 month with resolving of her symptoms completely and return to her normal life activities safely.
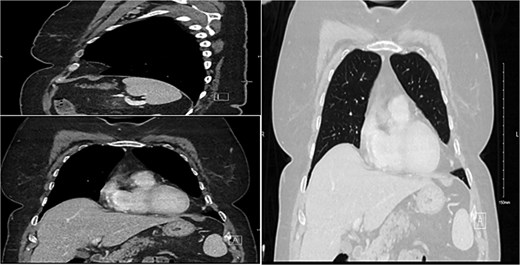
Demonstration of a pleural-based soft tissue mass consistent with lipoma.
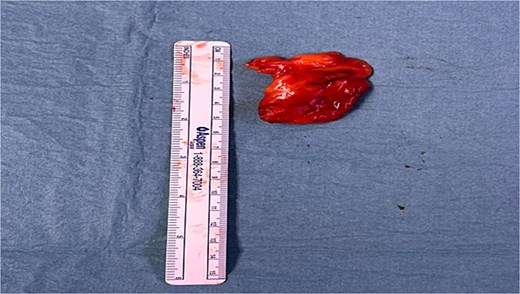
Pleural lipoma after surgical resection, sent after for pathological testing.
Discussion
Intrathoracic tumor was first described by Fothergill in 1781 [7]. Lipoma is an extremely rare benign mesenchymal slow-growing tumor that commonly originates in the deep and subcutaneous areas of the human body. Most pleural lipomas are clinically asymptomatic, but they can cause symptoms like cough, dysphagia, chest tightness, and shortness of breath [8]. Usually, they are discovered incidentally following a chest X-ray or CT scan performed for other reasons. Lipomas are classified into many types based on their origin. These include diaphragmatic, end bronchial and, in our case, pleural lipoma, which is of submesothelial parietal pleura origin with the capacity to extend into subpleural, pleural or extrapleural spaces [9]. Also it is subclassified into purely intrathoracic lipoma such as our case or dumbbell/hourglass lipomas which extend from the thoracic cavity across the anatomic thoracic inlet or intercostal space [8].
Pleural lipomas do not have a risk of malignant transformation and are typically asymptomatic [10]. However, we believe our patient presenting symptom pleuritic chest pain is due to the lipoma, as the patient intra-operatively was found to have this lipoma attached to intercostal space and adhered to the lung and pericardial fat. As a result of this attachment to the intercostal space a traction effect on the nerve might contribute to her presentation. Diagnostically, CT imaging has superiority over X-ray and ultrasound due to its accuracy in thoracic lipomas [10]. Additionally, it has a characteristic of homogeneity, obtuse-angled, fat-attenuating mass allows a definitive diagnosis of lipoma on CT [11]. However, there are case reports of lipomas containing fibrous stroma or dystrophic ring-type calcifications that make diagnosis sometimes challenging based on radiological evidence alone [12, 13]. As a result, a histopathological investigation is recommended to differentiate between similarly presenting fat-containing intrathoracic masses such as our case.
Management strategy is still debatable due to the nature of pleural lipoma that manifests a slow-growing and commonly asymptomatic benign tumor so management is dependent on age, tumor size, and symptoms. Many studies recommend, when possible, surgical excision for improved therapeutic and diagnostic outcomes [9]. This is reinforced by the good outcomes of surgical resection via VATS, with a very minimal recurrence rate of less than 5% [14]. In very rare cases, pleural lipoma can lead to serious consequences like heart failure when compress adjacent organs like the heart that also reported [15].
Conclusion
In general, pleural lipoma is considered as a rare benign, slowly growing neoplasm. Usually, patients will show no symptoms unless it is adherent to the surrounding organs or with a size sufficient to make compressive effects, including cough, dysphagia, chest tightness, and shortness of breath or traction-related symptoms as in our case. Diagnosis of pleural lipomas is via CT scan and confirmed by histopathology result. Surgical management via open or VATS for symptomatic patient remains gold standard. As pleural lipoma is reported sporadically in literature, so it is important to publish more to provide surgeons with an insight about its existence and the importance of its consideration when facing patients with intrathoracic mass. Also add to scientific literature more valuable information about this rare condition.
Conflict of interest statement
None declared.
Funding
None declared.



