-
PDF
- Split View
-
Views
-
Cite
Cite
Ai Lee, Yen-Kuang Lin, Yu-Huei Lin, Wen-Pei Chang, A longitudinal study of rotating shift type and attention performance of acute and critical care nurses with chronotype as moderator variable, Journal of Occupational Health, Volume 66, Issue 1, January-December 2024, uiae042, https://doi.org/10.1093/joccuh/uiae042
Close - Share Icon Share
Abstract
To investigate whether chronotype is a moderator variable that also interacts with shift type and whether they jointly influence the attention performance of nurses working in acute and critical care units.
We adopted a longitudinal research design focusing on nurses working rotating shifts in the emergency room and intensive care units at a medical center. A total of 40 complete samples were obtained. Data analysis was conducted using the generalized estimating equations in SAS 9.4.
The mean (SD) age of the participants was 26.35 (2.12) years. After controlling for age, gender, and sleep duration, an interaction effect was discovered between a specific chronotype and shift type; that is, the interaction effect between chronotype and shift type was only significant when comparing late-types working the night shift with early- and intermediate-types working the night shift (B = −18.81, P = .011). The least squares means of the mean reaction time of the interaction effects between the 2 chronotype groups and the 3 shift types found that the mean reaction time of late-types working the night shift was 11.31 ms (P = .044) slower compared with working the day shift.
The chronotype is a moderator variable between shift type and mean reaction time, such that matching the chronotype of nurses in acute and critical care units with the appropriate shift type improved their mean reaction time. It is hoped that the results of this study could serve as a reference for acute and critical care nurses when scheduling their shifts.
Key points
What is already known on this topic: Existing studies have found that the type of work shift influences the cognitive functions of nurses. However, whether shift type influences the attention performance of nurses with different chronotypes working different shifts is not clearly understood.
What this study adds: The attention of acute and critical care nurses was jointly influenced by the interaction effect between their chronotype and shift type rather than by shift type alone. Chronotype is a moderator variable between shift type and mean reaction time.
How this study might affect research, practice, or policy: Better regulation of their own circadian rhythms could lead to more focus at work and improve nursing quality.
Introduction
As patient care duties in hospitals are nonstop, especially those in acute and critical care units, nurses must work shifts in order to provide patients with round-the-clock, year-round care.1 However, when the shifts that nurses work are not aligned with their circadian rhythms, their unmet sleep needs can result in fatigue, distraction, memory loss, decreased job satisfaction, and increased risk of disease.2 Existing studies have indicated that rotating shifts are associated with the individual cognitive dysfunction of shift workers, such as loss of attention or increased reaction time (RT).3,4 Emergency rooms (ERs) and intensive care units (ICUs) are both acute and critical care units. Nurses in acute and critical care units routinely face patients in urgent condition and must be attentive to changes in patients’ conditions at all times.5 A loss in focus, even very minor, could lead to medical errors that could easily harm or cause death to patients.6
Chronotypes are defined as the behavioral differences in the body that are regulated by circadian rhythms, the most distinct of which are sleep/wake periods.7 Chronotypes are generally regarded as preferences for waking up early or late, and are divided into different types based on personal routines and sleeping hours.8 The chronotypes of different individuals can vary widely and are subject to the influence of various factors, such as gender; for example, research has shown that males generally function better at night, also known as night owls.9 Age is another factor; for instance, the majority of teenagers are night owls, whereas children and elderly individuals are more commonly morning people or early risers.10,11 Chronotype can reflect when an individual’s body functions, hormones, body temperature, cognitive abilities, and eating and sleeping patterns are active throughout the day.12 Moreover, chronotype can substantially influence work and learning performance.13
Findings from past studies regarding nurse shifts and attention have been inconsistent. Whereas some studies have indicated that rotating shift work results in drowsiness and difficulty in adjusting circadian rhythms, which decreases the level of attention and alertness in nurses,14,15 other studies have reported that the attention of nurses is not affected regardless of which shift is worked.16,17 Furthermore, studies not focusing on nurses have noted that attention performance varies throughout the day and that the interaction effect between sleep schedule and chronotype also affects attention performance.18,19 We therefore aimed to understand whether shift type influences the level of attention of acute and critical care nurses and whether chronotype jointly influences their attention performance.
Methods and measures
Research design and participants
We adopted a longitudinal research design focusing on nurses working rotating shifts in the ER and ICUs at a medical center in northern Taiwan. To provide nonstop care, acute and critical care wards must have adequate lighting 24 hours a day. At the medical center, consistent lighting day and night was ensured by fixing the lighting at 500 lx to 750 lx during all 3 shifts. Nursing work at the medical center followed a 3-shift schedule: day shift (7:30 am to 3:30 pm), evening shift (3:30 pm to 11:00 pm), and night shift (11:00 pm to 7:30 am). Although overtime was not routine in any of the shifts, nurses sometimes left work around half an hour after their scheduled shift time in order to perform handover to the nurses working the next shift. There was half an hour of rest time beginning at the midpoint of each shift: day shift (11:30 am to 12:00 am), evening shift (7:00 pm to 7:30 pm), and night shift (3:30 am to 4:00 am). Note that nurses were unable to take naps during any of the shifts. The participants comprised nurses who were aged 20 or above, worked a rotating shift schedule with 3 shifts (including the morning shift, evening shift, and night shift), understood and responded to the content of our questionnaire, cooperated in taking attention tests, understood the content and objectives of this study, and signed a paper informed consent form. Nurses who worked a fixed shift, were taking psychiatric drugs that affected attention, were diagnosed with attention deficit or sleep-related disorders, or could not work rotating shifts due to pregnancy or breastfeeding were excluded from this study. The number of study samples required was estimated using G-Power 3.1 with a significance level setting of .05, power setting of .80, medium effect size, and repeated measures analysis of variance (ANOVA) of intrinsic factors. The result determined that at least 33 samples were needed. Based on an estimated sample loss rate of approximately 20%, 42 nurses were recruited as participants.
Research ethics
Before recruiting participants, the institutional review board of the Tri-Service General Hospital reviewed our study proposal (No. A202205213). Only when we received approval did we begin to recruit participants. Before data collection, we explained the study aims and procedures to the participants in detail and answered any questions that they had. Data collection commenced when the participants gave consent and signed an informed consent form.
Data collection procedure
All of the ER and ICU nurses in this study worked a shift system with irregular and fast rotations. They changed shifts every 6 to 7 days, and there was no fixed order determining their next shift. All of the nurses filled out our questionnaire while working the evening shift. We arranged to administer the Brief Psychomotor Vigilance Test (PVT-B) to the participants during the rest time in each shift type, that is, at around 12:00 am during the day shift, 7:30 pm during the evening shift, and 4:00 am during the night shift. The purpose of this was to prevent any disturbances in the outside work environment from affecting the test results and thereby increase the validity and reliability of the test. During the PVT-B, the brightness of the PVT-B screen remained the same during all 3 shift types. The nurses who consented to participate in this study were first advised to obtain sufficient sleep, which was ideally more than 7 hours in total, the day before they took the PVT-B. They were also asked to avoid the following activities on the day before the test so that the test results would not be affected: engaging in high-intensity physical activities as well as drinking alcohol and caffeinated and/or energy drinks. On the day of the PVT-B, a checklist was used to confirm whether the participants followed these instructions to ensure the accuracy of the test results. Furthermore, based on previous research, we required that the nurses had gotten at least 2 rest days before each PVT-B in order to minimize any difficulty adapting to the new schedule after changing shift type. Two days was chosen based on findings by Chang et al,20 who discovered that when nurses working the night shift rotated to the day shift, having only 1 day of rest affected their alertness, execution function ability, and attention performance. Furthermore, to prevent the effects of working on the first day of rotating to a new shift from influencing our test results, we only conducted the PVT-B on the second day of working the same type of shift.
Research instruments
Via questionnaire surveys, we first obtained the basic information and chronotype of the participating nurses. A PVT-B device was then used to assess the attention performance of the nurses. Each instrument is described as follows.
The basic information questionnaire comprised 12 question items regarding age, gender, work experience, department of employment, educational background, marital status, drinking frequency, smoking habit, average daily sleep duration during the past 7 days, presence of preschool children at home, use of hypnotics, and use of psychiatric medication. The Munich Chronotype Questionnaire for shift workers (MCTQSHIFT) was presented by Juda et al in 2013.21 This questionnaire uses images to guide respondents through question items regarding the process of going to bed and waking up on workdays and free days in the past 2 weeks. Variables used to determine chronotype include the sleep duration on workdays (SDW) working the morning shift (M), evening shift (E), or night shift (N); sleep duration on free days (SDF); and the midpoint of sleep on workdays (MSW) and free days (MSF). The equation (number of workdays a week × SDW + number of free days a week × SDF)/7 is then used to calculate the weekly average sleep duration (ØSD). When the nurses slept less on workdays than on free days, the sleep-corrected (SC) midpoint of sleep on free days (MSFSC) was used to determine their chronotype; the equation was MSFSC = MSF – (SDF – ØSD)/2. The sleep-corrected midpoint of sleep on free days after evening shifts (MSFEsc) is the best variable for determining the chronotype of shift workers. We therefore employed MSFEsc to determine the chronotypes of the nurses in this study, which included early-types (MSFEsc ≤ 3:59), intermediate-types (MSFEsc = 4:00-4:59), and late-types (MSFEsc ≥ 5:00).21
The attention performance of the nurses was assessed using the PVT-B. Existing studies have demonstrated that the Psychomotor Vigilance Test (PVT) can objectively assess sleep deprivation, prolonged wake time during sleep, fatigue induced by circadian misalignment, and the influence of changes in circadian rhythms on vigilance during work.22 However, the conventional PVT takes 10 minutes, which is considered unfeasible in real environments. To address this issue, Basner et al23 modified the PVT to the 3-minute PVT-B. Research has shown that not only is the PVT-B a valid and credible tool for evaluating changes in attention with stable repeatable measurement, but it is also simple with adequate sensitivity.24 We performed the PVT-B using a PVT-192 Psychomotor Vigilance Task Monitor (Ambulatory Monitoring Inc., New York). The nurses were required to place the PVT-192 on their lap with the screen at 14 to 22 inches from their eyes in an environment with no noise or interruptions; they used the thumb or index finger of their dominant hand to press the designated button. The test took 3 minutes with a visual stimulus every 1 to 4 seconds. The participants had to press the designated button in response to the visual stimuli presented at random intervals. Whether they could maintain focus and attention was assessed based on their RT.22,23 The parameters included mean RT and the total number of errors. The latter was the total number of incorrect operations made by the participants, which included pressing the wrong button, pressing buttons in the absence of a stimulus, or pressing a button too fast (RT < 100 ms). A shorter mean RT and a smaller total number of errors indicate better attention.24
Statistical methods
The data for each ER and ICU nurse included 1 basic information questionnaire and 3 sets of PVT-B results. We encoded the data and analyzed them using SAS version 9.4 (SAS Institute Inc.). The descriptive statistics included frequency distribution, percentage, mean, and SD to describe the basic traits and chronotypes of the shift nurses. Only 2 nurses were intermediate-types; therefore, we combined the early- and intermediate-types into 1 group and compared it with the late-types. We first compared the age, work experience, and average sleep duration of the 2 groups using independent samples t-tests. For variables of the 2 chronotype groups, the expected values in over 20% of the cells in the contingency table were less than 5; therefore, we employed the Fisher exact test for statistical analysis. To analyze the interaction effects between chronotype and shift type, we first controlled the other moderating variables and, in consideration of the dependence between the mean RT and the total number of errors for each nurse during the 3 different shifts, employed the generalized estimating equations (GEEs) for analysis. We selected the exchangeable working correlation matrix to control for the effects of time. The factors included chronotype (the early- and intermediate-type group and the late-type group), shift type (the day shift, evening shift, and night shift), and their interaction effect (chronotype × shift type). A significant interaction effect (chronotype × shift type) means that there were significant differences in chronotype when shift type changed. We also included age, gender, and sleep duration in the model as moderating variables to control for their effects.8–11 In all of the analyses, a P value less than .05 indicated a statistical difference.
Results
Distributions of nurses in basic demographic attributes, healthy behavior, attention performance, and chronotype
A total of 42 participants were recruited for this study. During the course of this study, 1 participant became pregnant and could not continue working rotating shifts, and 1 participant resigned. Thus, we derived a total of 40 study samples. For chronotype, there were 9, 2, and 29 participants belonging to the early, intermediate, and late chronotypes, respectively. The mean age of the participants was 26.35 years, and there were markedly more females (77.5%) than males (22.5%). Their mean work experience in nursing was 52.72 months. The majority had a university or college degree (90.0%), and most were single (92.5%). In terms of healthy behavior, the drinking frequency of the largest group in alcohol drinking habits was once or less per month (45.0%), and only 1 participant had a smoking habit (2.5%). The participants were advised to obtain at least 7 hours of sleep before taking the PVT-B. The MCTQSHIFT questionnaire revealed that the average (SD) sleep duration of all of the participants on the day before an evening shift was 7.67 (1.35) hours; the average sleep duration on workdays and free days was, respectively, 7.68 (0.68) hours and 7.70 (1.37) hours. Furthermore, the basic information questionnaire indicated that the average daily sleep duration of the participants during the past 7 days was 6.96 (0.96) hours, and that they woke up 3.37 (1.78) hours before their evening shift. Note that this information was collected only during evening shifts. The 2 chronotype groups exhibited no significant differences in any demographic attribute or healthy behavior habit (Table 1).
Distributions of nurses in basic demographic attributes, healthy behavior habits, and chronotype (n = 40).
| Basic attribute . | . | Chronotype . | . | |
|---|---|---|---|---|
| All samples . | Early- and intermediate-types (n = 11) . | Late-types (n = 29) . | . | |
| n (%) or x- ± SD . | n (%) or x- ± SD . | n (%) or x- ± SD . | P . | |
| Age, y | 26.35 ± 2.12 | 26.27 ± 2.28 | 26.38 ± 2.09 | .804a |
| Gender | ||||
| Male | 9 (22.5) | 4 (36.4) | 5 (17.2) | .227b |
| Female | 31 (77.5) | 7 (63.6) | 24 (82.8) | |
| Work experience in nursing, mo | 52.72 ± 24.92 | 49.55 ± 23.8 | 53.93 ± 25.64 | .834a |
| Department of employment | ||||
| ER | 35 (87.5) | 9 (81.8) | 27 (93.1) | .603b |
| ICU | 5 (12.5) | 2 (18.2) | 2 (6.9) | |
| Educational background | ||||
| University or college | 36 (90.0) | 9 (81.8) | 27 (93.1) | .300b |
| Graduate school or higher | 4 (10.0) | 2 (18.2) | 2 (6.9) | |
| Marital status | ||||
| Single | 37 (92.5) | 11 (100) | 26 (89.7) | .548b |
| Married | 3 (7.5) | 0 (0) | 3 (10.3) | |
| Drinking frequency | ||||
| Never or less than once or twice a year | 12 (30.0) | 2 (18.2) | 10 (34.5) | .225b |
| Once or less a month | 18 (45.0) | 4 (36.4) | 14 (48.3) | |
| Twice or more a month | 10 (25.0) | 5 (45.5) | 5 (17.2) | |
| Smoking habit | ||||
| Yes | 1 (2.5) | 1 (9.1) | 0 (0) | .275b |
| No | 39 (97.5) | 10 (90.9) | 29 (100) | |
| Sleep duration, h | 6.96 ± 0.96 | 6.46 ± 1.06 | 7.16 ± 0.87 | .618a |
| Children at home | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Use of hypnotics | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Use of psychiatric medication | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Basic attribute . | . | Chronotype . | . | |
|---|---|---|---|---|
| All samples . | Early- and intermediate-types (n = 11) . | Late-types (n = 29) . | . | |
| n (%) or x- ± SD . | n (%) or x- ± SD . | n (%) or x- ± SD . | P . | |
| Age, y | 26.35 ± 2.12 | 26.27 ± 2.28 | 26.38 ± 2.09 | .804a |
| Gender | ||||
| Male | 9 (22.5) | 4 (36.4) | 5 (17.2) | .227b |
| Female | 31 (77.5) | 7 (63.6) | 24 (82.8) | |
| Work experience in nursing, mo | 52.72 ± 24.92 | 49.55 ± 23.8 | 53.93 ± 25.64 | .834a |
| Department of employment | ||||
| ER | 35 (87.5) | 9 (81.8) | 27 (93.1) | .603b |
| ICU | 5 (12.5) | 2 (18.2) | 2 (6.9) | |
| Educational background | ||||
| University or college | 36 (90.0) | 9 (81.8) | 27 (93.1) | .300b |
| Graduate school or higher | 4 (10.0) | 2 (18.2) | 2 (6.9) | |
| Marital status | ||||
| Single | 37 (92.5) | 11 (100) | 26 (89.7) | .548b |
| Married | 3 (7.5) | 0 (0) | 3 (10.3) | |
| Drinking frequency | ||||
| Never or less than once or twice a year | 12 (30.0) | 2 (18.2) | 10 (34.5) | .225b |
| Once or less a month | 18 (45.0) | 4 (36.4) | 14 (48.3) | |
| Twice or more a month | 10 (25.0) | 5 (45.5) | 5 (17.2) | |
| Smoking habit | ||||
| Yes | 1 (2.5) | 1 (9.1) | 0 (0) | .275b |
| No | 39 (97.5) | 10 (90.9) | 29 (100) | |
| Sleep duration, h | 6.96 ± 0.96 | 6.46 ± 1.06 | 7.16 ± 0.87 | .618a |
| Children at home | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Use of hypnotics | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Use of psychiatric medication | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
Abbreviations: ER, emergency room; ICU, intensive care unit; x- ± SD, mean ± SD.
Value calculated using independent samples t-test.
Value calculated using Fisher exact test.
Distributions of nurses in basic demographic attributes, healthy behavior habits, and chronotype (n = 40).
| Basic attribute . | . | Chronotype . | . | |
|---|---|---|---|---|
| All samples . | Early- and intermediate-types (n = 11) . | Late-types (n = 29) . | . | |
| n (%) or x- ± SD . | n (%) or x- ± SD . | n (%) or x- ± SD . | P . | |
| Age, y | 26.35 ± 2.12 | 26.27 ± 2.28 | 26.38 ± 2.09 | .804a |
| Gender | ||||
| Male | 9 (22.5) | 4 (36.4) | 5 (17.2) | .227b |
| Female | 31 (77.5) | 7 (63.6) | 24 (82.8) | |
| Work experience in nursing, mo | 52.72 ± 24.92 | 49.55 ± 23.8 | 53.93 ± 25.64 | .834a |
| Department of employment | ||||
| ER | 35 (87.5) | 9 (81.8) | 27 (93.1) | .603b |
| ICU | 5 (12.5) | 2 (18.2) | 2 (6.9) | |
| Educational background | ||||
| University or college | 36 (90.0) | 9 (81.8) | 27 (93.1) | .300b |
| Graduate school or higher | 4 (10.0) | 2 (18.2) | 2 (6.9) | |
| Marital status | ||||
| Single | 37 (92.5) | 11 (100) | 26 (89.7) | .548b |
| Married | 3 (7.5) | 0 (0) | 3 (10.3) | |
| Drinking frequency | ||||
| Never or less than once or twice a year | 12 (30.0) | 2 (18.2) | 10 (34.5) | .225b |
| Once or less a month | 18 (45.0) | 4 (36.4) | 14 (48.3) | |
| Twice or more a month | 10 (25.0) | 5 (45.5) | 5 (17.2) | |
| Smoking habit | ||||
| Yes | 1 (2.5) | 1 (9.1) | 0 (0) | .275b |
| No | 39 (97.5) | 10 (90.9) | 29 (100) | |
| Sleep duration, h | 6.96 ± 0.96 | 6.46 ± 1.06 | 7.16 ± 0.87 | .618a |
| Children at home | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Use of hypnotics | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Use of psychiatric medication | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Basic attribute . | . | Chronotype . | . | |
|---|---|---|---|---|
| All samples . | Early- and intermediate-types (n = 11) . | Late-types (n = 29) . | . | |
| n (%) or x- ± SD . | n (%) or x- ± SD . | n (%) or x- ± SD . | P . | |
| Age, y | 26.35 ± 2.12 | 26.27 ± 2.28 | 26.38 ± 2.09 | .804a |
| Gender | ||||
| Male | 9 (22.5) | 4 (36.4) | 5 (17.2) | .227b |
| Female | 31 (77.5) | 7 (63.6) | 24 (82.8) | |
| Work experience in nursing, mo | 52.72 ± 24.92 | 49.55 ± 23.8 | 53.93 ± 25.64 | .834a |
| Department of employment | ||||
| ER | 35 (87.5) | 9 (81.8) | 27 (93.1) | .603b |
| ICU | 5 (12.5) | 2 (18.2) | 2 (6.9) | |
| Educational background | ||||
| University or college | 36 (90.0) | 9 (81.8) | 27 (93.1) | .300b |
| Graduate school or higher | 4 (10.0) | 2 (18.2) | 2 (6.9) | |
| Marital status | ||||
| Single | 37 (92.5) | 11 (100) | 26 (89.7) | .548b |
| Married | 3 (7.5) | 0 (0) | 3 (10.3) | |
| Drinking frequency | ||||
| Never or less than once or twice a year | 12 (30.0) | 2 (18.2) | 10 (34.5) | .225b |
| Once or less a month | 18 (45.0) | 4 (36.4) | 14 (48.3) | |
| Twice or more a month | 10 (25.0) | 5 (45.5) | 5 (17.2) | |
| Smoking habit | ||||
| Yes | 1 (2.5) | 1 (9.1) | 0 (0) | .275b |
| No | 39 (97.5) | 10 (90.9) | 29 (100) | |
| Sleep duration, h | 6.96 ± 0.96 | 6.46 ± 1.06 | 7.16 ± 0.87 | .618a |
| Children at home | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Use of hypnotics | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
| Use of psychiatric medication | ||||
| Yes | 0 (0) | 0 (0) | 0 (0) | 1.00b |
| No | 40 (100) | 11 (100) | 29 (100) | |
Abbreviations: ER, emergency room; ICU, intensive care unit; x- ± SD, mean ± SD.
Value calculated using independent samples t-test.
Value calculated using Fisher exact test.
Comparison of mean RT of different chronotypes during 3 shifts
Despite Table 1 showing that the participants in the 2 chronotype groups exhibited no significant differences in any of the demographic attributes or healthy behavior variables, past studies have found that age, gender, and sleep duration exert a greater impact on attention and cognitive performance. For this reason, we still regarded the age, gender, and sleep duration of the participants as moderating variables and controlled for their effects.8–11 With early- and intermediate-types as the reference group for chronotype, and the day shift as the reference group for shift type, the results of the GEE are shown in Table 2. Among the extraneous variables, the Gk lower case beta B of age was −8.56 (P = .001) and that of sleep duration was −21.02 (P = .005). This means that as age increased, sleep duration increased and mean RT decreased. After controlling the extraneous variables, we found that the mean RT of late-types was significantly longer than that of early- and intermediate-types by 30.36 ms (P = .030). In the interaction effect between chronotype and shift type, the Gk lower case beta B of late-types working the night shift was −18.81(P = .011), thereby indicating that the interaction effect between chronotype and shift type was only significant in late-types working the night shift compared with early- and intermediate-types working the night shift. To more concretely elucidate the mean RT of different chronotypes working different shifts, we again divided the chronotypes into 2 groups, and each group exhibited significant differences in mean RT among the 3 different shifts. We then obtained and compared the least squares means (LSMs) of mean RT of the interaction effects between chronotype and shift type, with the resulting bar chart shown in Figure 1. The results indicate that when late-types were working the night shift, the LSM of their mean RT was less than that when they were working the day shift by 11.31 ms (P = .044).
GEE analysis of influence of chronotype and shift type on mean RT of nurses.
| Variable . | Mean RT . | ||
|---|---|---|---|
| B . | 95% CI . | P . | |
| Age | −8.56 | −13.56 to −3.56 | .001 |
| Gender: female (reference group: male) | −15.67 | −50.77 to 19.44 | .382 |
| Sleep duration | −21.02 | −35.79 to −6.25 | .005 |
| Chronotype: late-type (reference group: early- and intermediate-types) | 30.36 | 2.99 to 57.74 | .030 |
| Shift type (reference group: day shift) | |||
| Night shift | 7.50 | −1.90 to 16.90 | .118 |
| Evening shift | 3.87 | −3.62 to 11.36 | .311 |
| Interaction effecta | |||
| Late-type × night shift (reference group: early- and intermediate-types × night shift) | −18.81 | −33.26 to −4.36 | .011 |
| Late-type × evening shift (reference group: early- and intermediate-types × evening shift) | −8.41 | −19.13 to 2.32 | .124 |
| Late-type × day shift (reference group: early- and intermediate-types × day shift) | — | — | — |
| Variable . | Mean RT . | ||
|---|---|---|---|
| B . | 95% CI . | P . | |
| Age | −8.56 | −13.56 to −3.56 | .001 |
| Gender: female (reference group: male) | −15.67 | −50.77 to 19.44 | .382 |
| Sleep duration | −21.02 | −35.79 to −6.25 | .005 |
| Chronotype: late-type (reference group: early- and intermediate-types) | 30.36 | 2.99 to 57.74 | .030 |
| Shift type (reference group: day shift) | |||
| Night shift | 7.50 | −1.90 to 16.90 | .118 |
| Evening shift | 3.87 | −3.62 to 11.36 | .311 |
| Interaction effecta | |||
| Late-type × night shift (reference group: early- and intermediate-types × night shift) | −18.81 | −33.26 to −4.36 | .011 |
| Late-type × evening shift (reference group: early- and intermediate-types × evening shift) | −8.41 | −19.13 to 2.32 | .124 |
| Late-type × day shift (reference group: early- and intermediate-types × day shift) | — | — | — |
Abbreviations: B, unstandardized Gk lower case beta; GEE, generalized estimating equation; RT, reaction time.
Interaction effect variables were sleep pattern preference × shift type.
GEE analysis of influence of chronotype and shift type on mean RT of nurses.
| Variable . | Mean RT . | ||
|---|---|---|---|
| B . | 95% CI . | P . | |
| Age | −8.56 | −13.56 to −3.56 | .001 |
| Gender: female (reference group: male) | −15.67 | −50.77 to 19.44 | .382 |
| Sleep duration | −21.02 | −35.79 to −6.25 | .005 |
| Chronotype: late-type (reference group: early- and intermediate-types) | 30.36 | 2.99 to 57.74 | .030 |
| Shift type (reference group: day shift) | |||
| Night shift | 7.50 | −1.90 to 16.90 | .118 |
| Evening shift | 3.87 | −3.62 to 11.36 | .311 |
| Interaction effecta | |||
| Late-type × night shift (reference group: early- and intermediate-types × night shift) | −18.81 | −33.26 to −4.36 | .011 |
| Late-type × evening shift (reference group: early- and intermediate-types × evening shift) | −8.41 | −19.13 to 2.32 | .124 |
| Late-type × day shift (reference group: early- and intermediate-types × day shift) | — | — | — |
| Variable . | Mean RT . | ||
|---|---|---|---|
| B . | 95% CI . | P . | |
| Age | −8.56 | −13.56 to −3.56 | .001 |
| Gender: female (reference group: male) | −15.67 | −50.77 to 19.44 | .382 |
| Sleep duration | −21.02 | −35.79 to −6.25 | .005 |
| Chronotype: late-type (reference group: early- and intermediate-types) | 30.36 | 2.99 to 57.74 | .030 |
| Shift type (reference group: day shift) | |||
| Night shift | 7.50 | −1.90 to 16.90 | .118 |
| Evening shift | 3.87 | −3.62 to 11.36 | .311 |
| Interaction effecta | |||
| Late-type × night shift (reference group: early- and intermediate-types × night shift) | −18.81 | −33.26 to −4.36 | .011 |
| Late-type × evening shift (reference group: early- and intermediate-types × evening shift) | −8.41 | −19.13 to 2.32 | .124 |
| Late-type × day shift (reference group: early- and intermediate-types × day shift) | — | — | — |
Abbreviations: B, unstandardized Gk lower case beta; GEE, generalized estimating equation; RT, reaction time.
Interaction effect variables were sleep pattern preference × shift type.
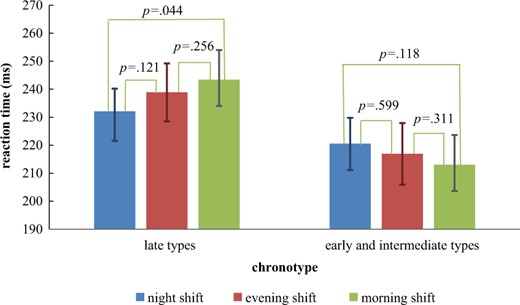
Differences between least squares means (LSMs) and SEMs of mean reaction time (RT) of interaction effects between chronotype and shift type.
Comparison of total number of errors of different chronotypes during 3 shifts
After controlling the extraneous variables, namely, age, gender, and sleep duration, we included the interaction effects of chronotype and shift type and used the early- and intermediate-types as the reference group for chronotype and the day shift as the reference group for shift type. The results for the interaction effects indicated no significant differences in the interaction effects with regard to the total number of errors, regardless of whether late-types worked the night shift or the evening shift (Table 3). To more specifically explain the total number of errors made by nurses with different chronotypes during different shifts, we again divided the chronotypes into 2 groups, both of which presented differences in the total number of errors in the 3 shift types. We then derived the LSMs of the mean RT of the interaction effects between chronotype and shift type and compared them using a bar chart, as shown in Figure 2. The results indicate no significant differences in the total number of errors, regardless of shift type or chronotype.
GEE analysis of influence of chronotype and shift type on total number of errors made by nurses.
| Variable . | Total number of errors . | ||
|---|---|---|---|
| B . | 95% CI . | P . | |
| Age | 0.11 | −0.21 to 0.42 | .498 |
| Gender: female (reference group: male) | −0.77 | −2.76 to 1.23 | .451 |
| Sleep duration | −0.82 | −1.78 to 0.13 | .092 |
| Chronotype: late-type (reference group: early- and intermediate-types) | −0.45 | −1.76 to 0.87 | .505 |
| Shift type (reference group: day shift) | |||
| Night shift | −0.07 | −0.75 to 0.61 | .836 |
| Evening shift | −0.55 | −1.16 to 0.07 | .082 |
| Variable . | Total number of errors . | ||
|---|---|---|---|
| B . | 95% CI . | P . | |
| Age | 0.11 | −0.21 to 0.42 | .498 |
| Gender: female (reference group: male) | −0.77 | −2.76 to 1.23 | .451 |
| Sleep duration | −0.82 | −1.78 to 0.13 | .092 |
| Chronotype: late-type (reference group: early- and intermediate-types) | −0.45 | −1.76 to 0.87 | .505 |
| Shift type (reference group: day shift) | |||
| Night shift | −0.07 | −0.75 to 0.61 | .836 |
| Evening shift | −0.55 | −1.16 to 0.07 | .082 |
Abbreviations: B, unstandardized Gk lower case beta; GEE, generalized estimating equation.
GEE analysis of influence of chronotype and shift type on total number of errors made by nurses.
| Variable . | Total number of errors . | ||
|---|---|---|---|
| B . | 95% CI . | P . | |
| Age | 0.11 | −0.21 to 0.42 | .498 |
| Gender: female (reference group: male) | −0.77 | −2.76 to 1.23 | .451 |
| Sleep duration | −0.82 | −1.78 to 0.13 | .092 |
| Chronotype: late-type (reference group: early- and intermediate-types) | −0.45 | −1.76 to 0.87 | .505 |
| Shift type (reference group: day shift) | |||
| Night shift | −0.07 | −0.75 to 0.61 | .836 |
| Evening shift | −0.55 | −1.16 to 0.07 | .082 |
| Variable . | Total number of errors . | ||
|---|---|---|---|
| B . | 95% CI . | P . | |
| Age | 0.11 | −0.21 to 0.42 | .498 |
| Gender: female (reference group: male) | −0.77 | −2.76 to 1.23 | .451 |
| Sleep duration | −0.82 | −1.78 to 0.13 | .092 |
| Chronotype: late-type (reference group: early- and intermediate-types) | −0.45 | −1.76 to 0.87 | .505 |
| Shift type (reference group: day shift) | |||
| Night shift | −0.07 | −0.75 to 0.61 | .836 |
| Evening shift | −0.55 | −1.16 to 0.07 | .082 |
Abbreviations: B, unstandardized Gk lower case beta; GEE, generalized estimating equation.
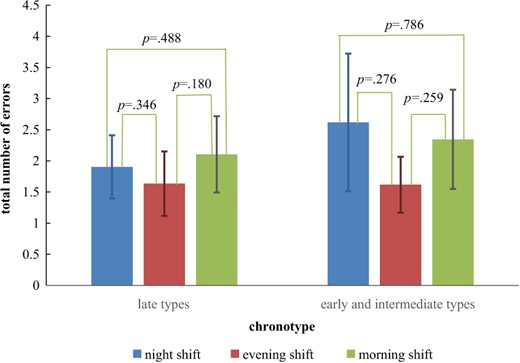
Differences between least squares means (LSMs) and SEMs of total number of errors of interaction effects between chronotype and shift type.
Discussion
The results of this study indicate that the attention of nurses working rotating shifts in acute and critical care units was jointly influenced by their chronotype and shift type rather than by shift type alone. When late-types worked the night shift, the interaction effect between their chronotype and shift type improved their mean RT compared with working the day shift. Encouragingly, the interaction effect between chronotype and shift type did not impact the total number of errors.
An individual’s chronotype indicates when they are most active and focused. The majority of adults who are not rotating-shift workers are intermediate-types.25,26 The changing work and rest schedules of rotating-shift workers indeed impact their biological clocks and disrupt their circadian rhythms. As a result, most rotating-shift workers tend to be early-types or late-types, with very few being intermediate-types.27 This study revealed similar results; that is, a very small proportion of the participants were intermediate-types. Furthermore, we found that the mean RTs of late-type nurses were significantly longer than those of early-types or intermediate-types; thus, we posit that numerous factors (e.g. their biological clocks, hormones, and sleep environment)28–30 may have significantly increased the mean RTs of late-type nurses.16
Chronotype is associated with the time at which the energy levels of an individual are highest during the day. For instance, the energy level of early risers is highest in the morning, whereas that of night owls is highest at night. Learning, work, and various activities should thus be scheduled based on chronotype where possible.31 As nurses are often required to work 3 shifts, their exposure to light at night increases, making late-types more common than early-types among nurses.32 Research has shown that a mismatch between shift type and chronotype can impair the sleep quality of rotating-shift nurses, rendering them fatigued during their shift.32 Human attention is influenced by the interaction effect between sleep schedule and chronotype,33 the latter of which is a moderator variable that influences attention.34 This study verified that the moderating effect of chronotype on attention performance also exists in nurses working rotating shifts. Results of existing research have also found a correlation between circadian misalignment and increases in RT.35,36
Rosa et al37 examined rotating-shift workers at a factory who worked a schedule with fast rotations, that is, a day shift for 2 days, an evening shift for 2 days, and a night shift for 2 days; they found that the performance of the factory workers was influenced by chronotype but not by shift type. With rotating-shift nurses as the research subject, this study derived a similar conclusion; the mean RT of the nurses was not only influenced by chronotype but also influenced jointly by chronotype and shift type. At present, the exact mechanisms underlying this interaction effect are still unclear.38 However, rotating shift workers whose chronotype matches their shift type appear to possess stronger melatonin rhythms than those whose chronotype does not match their shift type, suggesting that the former have better circadian functions.28 Melatonin rhythms are determined by the interaction effect between chronotype and shift type, and a better alignment between the two can reduce disruptions in melatonin rhythms.29
In contrast, the cognitive and neuromotor functions of nurses performing clinical work in rotating shift schedules that do not match their chronotype could be affected due to reduced sleep times and impaired sleep quality,39 which in turn prolongs their mean RT during tests.40 We also discovered that with regard to mean RT, only late chronotypes had interaction effects with shift type. Past research targeting drivers and undergraduate students also observed interaction effects between work time and chronotype; however, this was only found for late-types but not early-types. This indicates that late-types have more difficulty adjusting to sleep schedules that do not match their chronotype than do early-types.41 Furthermore, existing studies have also indicated that late-types have poorer sleep quality than do early-types, which results in poorer attention performance.42,43
Research has shown that memory, learning, executive functions, and physical strength are enhanced during an individual’s peak performance time.33 However, the results of this study indicate no significant differences in the total number of errors made by acute and critical care nurses, regardless of chronotype or shift type, due perhaps to the smaller sample size preventing us from detecting differences that could have existed or to the nature of nursing work in acute and critical care units, which requires nurses to remain highly vigilant. Although rotating shifts could disrupt their circadian rhythms and increase their fatigue, the sense of responsibility that acute and critical care nurses have for their work ensures that errors are kept to a minimum.18 We suggest that future studies increase the number of samples to further elucidate this concept.
This study further identified that the mean RTs of late-type nurses were significantly shorter when they were working the night shift compared with working the day shift. In addition to being influenced by the interaction effects between chronotype and shift type, RT could also be affected by the work pressure and fatigue perceived by nurses.44 The mean RT of the nurses may therefore vary. As the concentration, focus, and response speed of each nurse differ at work, understanding their individual differences can assist medical teams in more effectively allocating work to ensure that severely ill patients receive the best care. We therefore suggest that more related research be conducted to set a mean RT threshold for acute and critical care nurses, thus serving as an index for improving nursing quality.
Despite the smaller number of samples, we employed the GEE in our analysis and chose the exchangeable working correlation matrix, assuming that the variances were equal among the shift types and covariances. The compound symmetry of the covariance matrix in the exchangeable working correlation matrix was the same as that in the repeated measures ANOVA used to calculate the number of samples. We therefore used a repeated measures ANOVA as the sample number calculation model in G-Power. In the GEE in this study, we adopted multivariate analysis, which can suitably control for the effects of moderating variables such as age, gender, and sleep duration and ensure that the differences in the measured RT originated from the interaction effect between chronotype and shift type rather than from other possible moderating variables. We also conducted subgroup analysis on the 2 chronotype groups and the different shift types to examine the RT differences in the 2 chronotype groups and demonstrated that these differences indeed existed consistently within the groups and were thus not the result of bias in the number of samples. In conclusion, the methods above allowed us to determine that the significant differences in RT were the result of the interaction effect between chronotype and shift type rather than bias in the number of samples or other moderating variables.
Practical implications
An advantage of this study is that unlike laboratory research, it was conducted in the actual workplace of nurses. Each nurse took three 3-minute PVTs by which to compare their attention performance during different shifts; therefore, most of the variables influencing internal validity were controlled. It is suggested that hospital management take chronotype into consideration when scheduling shifts. Nurses working rotating shifts in acute and critical care units should also choose suitable shifts based on their chronotype wherever possible. Researchers can consider collecting menstrual cycle data in future studies to investigate the possible influence of menstrual cycles on sleep quality and PVT-B performance. Such data may provide valuable insight regarding the influence of the health and menstrual cycles of female rotating-shift nurses on their sleep and cognitive functions.
Conclusions
This study demonstrated that the shift type of nurses working in acute and critical care units does not independently affect their attention and that chronotype can moderate attention performance during shifts, that is, improvements in their RT. This means that the interaction between chronotype and shift type influences the RT of said nurses.
Acknowledgments
The protocol of this prospective interventional study was approved by the Ethics Committee at the Tri-Service General Hospital (No. A202205213), and written informed consent was obtained from all participants prior to inclusion.
Author contributions
W.-P.C. and A.L. conceived the presented idea, developed the theory, and performed the computations. Y.-K.L. and Y.-H.L. verified the analytical methods. W.-P.C. supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
Funding
This research received no specific grant from any funding agency in the commercial or not-for-profit sectors.
Conflicts of interest
The authors have no conflicts of interest.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.



