-
PDF
- Split View
-
Views
-
Cite
Cite
Philippe Gorce, Julien Jacquier-Bret, Three-month work-related musculoskeletal disorders assessment during manual lymphatic drainage in physiotherapists using Generic Postures notion, Journal of Occupational Health, Volume 65, Issue 1, January/December 2023, e12420, https://doi.org/10.1002/1348-9585.12420
Close - Share Icon Share
Abstract
The aim of this work was to quantify the postures and to assess the musculoskeletal disorders (MSDs) risk in physiotherapists repeating a manual lymphatic drainage (MLD) over a three-month period. The underlying hypothesis was that there would be Generic Postures (GP) that would be repeated and could be used to more simply describe repetitive and long-duration complex activities.
The posture of five physiotherapists performing five 20-min MLD at their workplace was captured by two cameras. From the recordings, the adopted postures were extracted every 5 s and quantified through 13 joint angles, that is, 6594 analyzed postures. Rapid Upper Limb (RULA) and Rapid Entire Body Assessment (REBA) were used to assess MSDs risks. A hierarchical analysis was used to define GP.
Seven GP were identified through mean values and standard deviation. GP ergonomic assessment showed a low to moderate MSD risk (RULA between 3 and 6 and REBA between 2 and 7). High neck (>20°) and trunk (>15°) flexion were observed for all GP. High shoulder abduction and flexion (>40°) were evidenced for GP3 to GP5. GP1 was the most used (34%) and presented the lowest ergonomic scores (RULA: 4.46 ± 0.84; REBA: 5.06 ± 1.75). GP3 to GP6 had frequency of between 10 and 20%. GP5, GP6, and GP7 obtained the highest ergonomic scores (RULA>5; REBA>7). All physiotherapists use different GP combinations to perform MLD.
MLD could be described as a combination of GP. Ergonomic analysis showed that MLD exposes physiotherapists to low at moderate MSD risks.
INTRODUCTION
Physiotherapists deal with a large number of patients every day. They perform many different tasks, such as lifting or transferring dependent patients, carrying or moving heavy material/equipment, various manual therapies techniques.1,2 These activities are often achieved in repeated awkward postures maintained for long time.3,4 All these factors expose physiotherapists to the risk of musculoskeletal disorders (MSDs).5,6 Numerous studies have reported a high prevalence of over 80% or even 90%.7–10 Several authors also used cross-sectional surveys to investigate the 12-month MSD prevalence by body area. They highlighted that the most exposed areas (over 40%) were mainly the neck (41.3%11 to 66.5%12), lower back (41.7%10 to 69.8%13), shoulder (42%9 to 62.2%12), and upper extremities (50.314 to 83.3%12).
Among the risk factors reported by physiotherapists, several are linked to the use of awkward postures during professional activities. These included frequent bending or twisting, repeating or maintaining cramped postures for long periods, or working near to joint limits..15
This information supports the importance of taking an interest in the description of posture in order to understand the occurrence of MSDs. Some authors investigated posture description among physiotherapists. Kang et al.16 quantified the kinematics of the lumbar, pelvis, and hips in physical therapists to prevent chronic low back pain. Albert et al.17 studied neck, trunk, and shoulder flexion during massage activities. The authors described posture throughout time spent in angular sectors that qualified the joint range: posture, that is, neutral, mild, and severe.
Other studies have described postures more accurately through angular variables.18 From the whole-body joint angle values, risk level of MSD exposure can be defined using ergonomic tools such as Rapid Upper Limb Assessment (RULA),19 the Rapid Entire Body Assessment (REBA),20 or the Novel Ergonomic Postural Assessment Method (NERPA).21 Jacquier-Bret et al. analyzed postures and the effect of stool movement during manual lymphatic drainage to assess the risk of MSDs.22,23 Based on RULA scores, the authors demonstrated that massage activities exposed physiotherapists to a moderate risk of MSDs. These two studies were carried out, respectively, on samples of 10 massages performed by the same physiotherapist and 14 massages performed by 7 different physiotherapists. In addition, Jacquier-Bret et al. also introduced the notion of Generic Posture.23 The authors showed that it was possible to group together the postures used by physiotherapists into clusters using an hierarchical cluster analysis. Seven GPs were identified. However, in these studies, the effect of time on the risk of MSDs when repeating an activity was not taken into account.
The aim of this work was to quantify the postures and to assess the risk of MSDs in physiotherapists repeating a lymphatic drainage massage over a three-month period. The underlying hypothesis was that there would be Generic Postures (GP) that would be repeated and could be used to more simply describe repetitive and long-duration complex activities.
METHODS
Task and participants
Five physiotherapists (1 male and 4 females named PT1 to PT5, 40.2 ± 11.3 years old, 166.2 ± 6.9 cm, 63.0 ± 7.6 kg, BMI: 22.9 ± 3.6, 17.6 ± 9.8 years of experience, all right-handed) voluntarily participated in the experience. They work in the neurology department of the Léon Bérard hospital. None of them have any pathologies or injuries that prevent them from working normally. They were informed of the entire protocol and gave their written consent before taking part in the experiment. The protocol is in line with the Helsinki agreement24 and has been approved by the ethics committee of the Léon Bérard hospital (LBCE-2023-11).
The task consisted in achieving five 20-min lymphatic drainage massage of an upper or lower limb spread over a three-month period. The physiotherapists were filmed in their department according to their time schedule and the patient’s admission. Two numeric cameras (Samsung Galaxy S20, 60 Hz) were positioned at 90° to each other close to the table to continuous film the entire massage in the frontal and sagittal planes.23 From the video recordings, two experts defined the postures (measurements of joint angles) adopted by the physiotherapists every 5 s, that is, 6594 postures. The joint angles were integrated into a model developed in MATLAB (The Mathworks, Inc.) to reproduce the posture estimated by the experts. This posture was then compared with that obtained from the videos, and the angle values were adjusted if necessary. Each posture was defined through 13 joint angles relative to neck, trunk, shoulders, elbows, hips, and knees flexion/extension and abduction/adduction or inclination following the International Society of Biomechanics recommendations.25,26 Flexions/extensions correspond to movements in the sagittal plane around the mediolateral axis. Abduction and inclination correspond to movements in the frontal plane around the anteroposterior axis of the body. Neck and trunk rotations were estimated using the model. MSD risk level of the 6594 postures was assessed using RULA and REBA.
Data analysis
A hierarchical cluster analysis (HCA) was performed on the 6594 postures using MATLAB (The Mathworks, Inc., Natick, MA). From the 13 joint angles, the Ward’s linkage method27 was used to compute the Euclidean distances and pool the nearest postures into clusters. The result was presented as dendrogram. The identification of the clusters was quantitatively determined by the agglomeration coefficient and this decision was verified by a visual inspection of the dendrogram. All postures attached to the same branch of the dendrogram are considered close and form an independent cluster. Each cluster is then defined by a mean posture called Generic Posture (GP). Each GP was defined by the 13 mean joint angles with standard deviation. The level of ergonomic risk of MSD occurrence (RULA and REBA scores) and the time spent in each GP in relation to the total massage duration (frequency of use) were added to qualify the GP. Dependent variables, that is, 13 joint angles and RULA/REBA scores of all postures constituting each independent cluster, were compared using the Kruskal-Wallis test. The significance level was set at 5%.
A detailed analysis of the 25 massages was then carried out using the RULA and REBA scores and GP frequencies. The mean values of RULA/REBA scores were computed in two different ways for each massage: (1) from the ergonomic scores computed for each posture constituting the massage and (2) from the mean ergonomic scores computed for each GP (Table 2) and its relative frequency in the massage (Table 1). The equations were as follows:
with n corresponding to the number of postures included in a massage. RULA and REBA scores obtained with the Equations (1) and (2) for each massage were also compared using the Kruskal-Wallis test.
Mean (standard deviation) joint angles and frequency for each GP throughout all massages.
| . | GP1 . | GP2 . | GP3 . | GP4 . | GP5 . | GP6 . | GP7 . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 |  |  |  |  |  |  | ||||||||
| Neck flexion (°) | 19.51 | (11.61) #367 | 24.22 | (5.93) | 21.83 | (10.13) #157 | 20.96 | (8.89) #67 | 21.51 | (5.67) #367 | 23.44 | (6.95) #1457 | 25.48 | (4.70) #13456 |
| Neck inclination (°) | 3.02 | (4.19) #234567 | 12.01 | (5.51) #1346 | 3.89 | (4.73) #12567 | 3.38 | (4.12) #12567 | 14.53 | (13.51) #1346 | 7.40 | (7.54) #123457 | 10.97 | (6.67) #1346 |
| Neck rotation (°) | 5.75 | (8.82) #4567 | 2.54 | (0.85) #456 | 3.89 | (3.93) #4567 | 3.83 | (5.58) #12357 | 2.54 | (3.93) #123467 | 2.47 | (2.79) #12357 | 3.71 | (3.60) #13456 |
| Trunk flexion (°) | 14.58 | (7.46) #567 | 16.58 | (6.83) #567 | 14.78 | (9.30) #567 | 14.90 | (8.93) #567 | 21.02 | (4.76) #1234 | 23.30 | (7.83) #1234 | 23.32 | (8.06) #1234 |
| Trunk inclination (°) | 7.28 | (6.75) #4567 | 5.32 | (4.02) #56 | 8.20 | (7.34) #56 | 8.09 | (6.54) #156 | 14.29 | (10.18) #123467 | 16.50 | (11.20) #123457 | 11.28 | (9.93) #156 |
| Trunk rotation (°) | 10.95 | (10.93) #34567 | 4.73 | (2.99) #5 | 4.94 | (5.74) #15 | 6.93 | (7.52) #15 | 14.96 | (10.21) #123467 | 5.28 | (5.63) #15 | 7.80 | (7.58) #15 |
| Shoulder flexion (°) | 11.99 | (12.01) #34567 | 12.27 | (14.88) #34567 | 26.60 | (10.43) #12456 | 44.31 | (16.47) #123567 | 52.30 | (22.02) #123467 | 35.16 | (12.64) #123457 | 29.12 | (14.70) #12456 |
| Shoulder abduction (°) | 13.17 | (10.65) #34567 | 12.93 | (6.06) #34567 | 50.34 | (15.97) #124567 | 21.70 | (17.44) #123567 | 23.62 | (13.33) #123467 | 28.97 | (12.97) #12345 | 28.63 | (14.69) #12345 |
| Elbow flexion (°) | 88.01 | (13.92) #123456 | 77.34 | (9.82) #134567 | 85.84 | (10.16) #124567 | 41.68 | (13.77) #123567 | 63.39 | (16.50) #1234 | 58.56 | (20.42) #1234 | 58.85 | (20.10) #1234 |
| Hip flexion (°) | 85.09 | (6.72) #2456 | 48.85 | (2.12) #134567 | 85.39 | (6.29) #2456 | 87.20 | (7.02) #12356 | 76.15 | (5.28) #123467 | 88.23 | (7.40) #123457 | 84.42 | (14.30) #256 |
| Hip abduction (°) | −1.61 | (13.35) #234567 | 0.00 | (0.00) #13467 | −6.84 | (7.93) #12567 | −6.26 | (6.30) #12567 | −1.28 | (10.36) #13467 | 26.94 | (6.67) #12345 | 22.84 | (12.42) #12345 |
| Hip rotation (°) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.40 | (5.65) | 0.00 | (0.00) |
| Knee flexion (°) | 88.74 | (5.29) #234567 | 0.00 | (0.00) #13467 | 86.61 | (4.90) #12567 | 87.03 | (4.90) #12567 | 73.10 | (9.78) #13467 | 90.78 | (5.37) #123457 | 134.42 | (7.51) #123456 |
| Frequency (%) | 34.0 | 1.1 | 15.5 | 19.2 | 10.4 | 15.2 | 4.7 | |||||||
| . | GP1 . | GP2 . | GP3 . | GP4 . | GP5 . | GP6 . | GP7 . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 |  |  |  |  |  |  | ||||||||
| Neck flexion (°) | 19.51 | (11.61) #367 | 24.22 | (5.93) | 21.83 | (10.13) #157 | 20.96 | (8.89) #67 | 21.51 | (5.67) #367 | 23.44 | (6.95) #1457 | 25.48 | (4.70) #13456 |
| Neck inclination (°) | 3.02 | (4.19) #234567 | 12.01 | (5.51) #1346 | 3.89 | (4.73) #12567 | 3.38 | (4.12) #12567 | 14.53 | (13.51) #1346 | 7.40 | (7.54) #123457 | 10.97 | (6.67) #1346 |
| Neck rotation (°) | 5.75 | (8.82) #4567 | 2.54 | (0.85) #456 | 3.89 | (3.93) #4567 | 3.83 | (5.58) #12357 | 2.54 | (3.93) #123467 | 2.47 | (2.79) #12357 | 3.71 | (3.60) #13456 |
| Trunk flexion (°) | 14.58 | (7.46) #567 | 16.58 | (6.83) #567 | 14.78 | (9.30) #567 | 14.90 | (8.93) #567 | 21.02 | (4.76) #1234 | 23.30 | (7.83) #1234 | 23.32 | (8.06) #1234 |
| Trunk inclination (°) | 7.28 | (6.75) #4567 | 5.32 | (4.02) #56 | 8.20 | (7.34) #56 | 8.09 | (6.54) #156 | 14.29 | (10.18) #123467 | 16.50 | (11.20) #123457 | 11.28 | (9.93) #156 |
| Trunk rotation (°) | 10.95 | (10.93) #34567 | 4.73 | (2.99) #5 | 4.94 | (5.74) #15 | 6.93 | (7.52) #15 | 14.96 | (10.21) #123467 | 5.28 | (5.63) #15 | 7.80 | (7.58) #15 |
| Shoulder flexion (°) | 11.99 | (12.01) #34567 | 12.27 | (14.88) #34567 | 26.60 | (10.43) #12456 | 44.31 | (16.47) #123567 | 52.30 | (22.02) #123467 | 35.16 | (12.64) #123457 | 29.12 | (14.70) #12456 |
| Shoulder abduction (°) | 13.17 | (10.65) #34567 | 12.93 | (6.06) #34567 | 50.34 | (15.97) #124567 | 21.70 | (17.44) #123567 | 23.62 | (13.33) #123467 | 28.97 | (12.97) #12345 | 28.63 | (14.69) #12345 |
| Elbow flexion (°) | 88.01 | (13.92) #123456 | 77.34 | (9.82) #134567 | 85.84 | (10.16) #124567 | 41.68 | (13.77) #123567 | 63.39 | (16.50) #1234 | 58.56 | (20.42) #1234 | 58.85 | (20.10) #1234 |
| Hip flexion (°) | 85.09 | (6.72) #2456 | 48.85 | (2.12) #134567 | 85.39 | (6.29) #2456 | 87.20 | (7.02) #12356 | 76.15 | (5.28) #123467 | 88.23 | (7.40) #123457 | 84.42 | (14.30) #256 |
| Hip abduction (°) | −1.61 | (13.35) #234567 | 0.00 | (0.00) #13467 | −6.84 | (7.93) #12567 | −6.26 | (6.30) #12567 | −1.28 | (10.36) #13467 | 26.94 | (6.67) #12345 | 22.84 | (12.42) #12345 |
| Hip rotation (°) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.40 | (5.65) | 0.00 | (0.00) |
| Knee flexion (°) | 88.74 | (5.29) #234567 | 0.00 | (0.00) #13467 | 86.61 | (4.90) #12567 | 87.03 | (4.90) #12567 | 73.10 | (9.78) #13467 | 90.78 | (5.37) #123457 | 134.42 | (7.51) #123456 |
| Frequency (%) | 34.0 | 1.1 | 15.5 | 19.2 | 10.4 | 15.2 | 4.7 | |||||||
Note: #X: statistically different from GPX with X between 1 and 7 for GP1 to GP7 (Kruskal-Wallis analysis, P < .05).
Abbreviation: GP1 to 7, Generic Posture 1 to 7.
Mean (standard deviation) joint angles and frequency for each GP throughout all massages.
| . | GP1 . | GP2 . | GP3 . | GP4 . | GP5 . | GP6 . | GP7 . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 |  |  |  |  |  |  | ||||||||
| Neck flexion (°) | 19.51 | (11.61) #367 | 24.22 | (5.93) | 21.83 | (10.13) #157 | 20.96 | (8.89) #67 | 21.51 | (5.67) #367 | 23.44 | (6.95) #1457 | 25.48 | (4.70) #13456 |
| Neck inclination (°) | 3.02 | (4.19) #234567 | 12.01 | (5.51) #1346 | 3.89 | (4.73) #12567 | 3.38 | (4.12) #12567 | 14.53 | (13.51) #1346 | 7.40 | (7.54) #123457 | 10.97 | (6.67) #1346 |
| Neck rotation (°) | 5.75 | (8.82) #4567 | 2.54 | (0.85) #456 | 3.89 | (3.93) #4567 | 3.83 | (5.58) #12357 | 2.54 | (3.93) #123467 | 2.47 | (2.79) #12357 | 3.71 | (3.60) #13456 |
| Trunk flexion (°) | 14.58 | (7.46) #567 | 16.58 | (6.83) #567 | 14.78 | (9.30) #567 | 14.90 | (8.93) #567 | 21.02 | (4.76) #1234 | 23.30 | (7.83) #1234 | 23.32 | (8.06) #1234 |
| Trunk inclination (°) | 7.28 | (6.75) #4567 | 5.32 | (4.02) #56 | 8.20 | (7.34) #56 | 8.09 | (6.54) #156 | 14.29 | (10.18) #123467 | 16.50 | (11.20) #123457 | 11.28 | (9.93) #156 |
| Trunk rotation (°) | 10.95 | (10.93) #34567 | 4.73 | (2.99) #5 | 4.94 | (5.74) #15 | 6.93 | (7.52) #15 | 14.96 | (10.21) #123467 | 5.28 | (5.63) #15 | 7.80 | (7.58) #15 |
| Shoulder flexion (°) | 11.99 | (12.01) #34567 | 12.27 | (14.88) #34567 | 26.60 | (10.43) #12456 | 44.31 | (16.47) #123567 | 52.30 | (22.02) #123467 | 35.16 | (12.64) #123457 | 29.12 | (14.70) #12456 |
| Shoulder abduction (°) | 13.17 | (10.65) #34567 | 12.93 | (6.06) #34567 | 50.34 | (15.97) #124567 | 21.70 | (17.44) #123567 | 23.62 | (13.33) #123467 | 28.97 | (12.97) #12345 | 28.63 | (14.69) #12345 |
| Elbow flexion (°) | 88.01 | (13.92) #123456 | 77.34 | (9.82) #134567 | 85.84 | (10.16) #124567 | 41.68 | (13.77) #123567 | 63.39 | (16.50) #1234 | 58.56 | (20.42) #1234 | 58.85 | (20.10) #1234 |
| Hip flexion (°) | 85.09 | (6.72) #2456 | 48.85 | (2.12) #134567 | 85.39 | (6.29) #2456 | 87.20 | (7.02) #12356 | 76.15 | (5.28) #123467 | 88.23 | (7.40) #123457 | 84.42 | (14.30) #256 |
| Hip abduction (°) | −1.61 | (13.35) #234567 | 0.00 | (0.00) #13467 | −6.84 | (7.93) #12567 | −6.26 | (6.30) #12567 | −1.28 | (10.36) #13467 | 26.94 | (6.67) #12345 | 22.84 | (12.42) #12345 |
| Hip rotation (°) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.40 | (5.65) | 0.00 | (0.00) |
| Knee flexion (°) | 88.74 | (5.29) #234567 | 0.00 | (0.00) #13467 | 86.61 | (4.90) #12567 | 87.03 | (4.90) #12567 | 73.10 | (9.78) #13467 | 90.78 | (5.37) #123457 | 134.42 | (7.51) #123456 |
| Frequency (%) | 34.0 | 1.1 | 15.5 | 19.2 | 10.4 | 15.2 | 4.7 | |||||||
| . | GP1 . | GP2 . | GP3 . | GP4 . | GP5 . | GP6 . | GP7 . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 |  |  |  |  |  |  | ||||||||
| Neck flexion (°) | 19.51 | (11.61) #367 | 24.22 | (5.93) | 21.83 | (10.13) #157 | 20.96 | (8.89) #67 | 21.51 | (5.67) #367 | 23.44 | (6.95) #1457 | 25.48 | (4.70) #13456 |
| Neck inclination (°) | 3.02 | (4.19) #234567 | 12.01 | (5.51) #1346 | 3.89 | (4.73) #12567 | 3.38 | (4.12) #12567 | 14.53 | (13.51) #1346 | 7.40 | (7.54) #123457 | 10.97 | (6.67) #1346 |
| Neck rotation (°) | 5.75 | (8.82) #4567 | 2.54 | (0.85) #456 | 3.89 | (3.93) #4567 | 3.83 | (5.58) #12357 | 2.54 | (3.93) #123467 | 2.47 | (2.79) #12357 | 3.71 | (3.60) #13456 |
| Trunk flexion (°) | 14.58 | (7.46) #567 | 16.58 | (6.83) #567 | 14.78 | (9.30) #567 | 14.90 | (8.93) #567 | 21.02 | (4.76) #1234 | 23.30 | (7.83) #1234 | 23.32 | (8.06) #1234 |
| Trunk inclination (°) | 7.28 | (6.75) #4567 | 5.32 | (4.02) #56 | 8.20 | (7.34) #56 | 8.09 | (6.54) #156 | 14.29 | (10.18) #123467 | 16.50 | (11.20) #123457 | 11.28 | (9.93) #156 |
| Trunk rotation (°) | 10.95 | (10.93) #34567 | 4.73 | (2.99) #5 | 4.94 | (5.74) #15 | 6.93 | (7.52) #15 | 14.96 | (10.21) #123467 | 5.28 | (5.63) #15 | 7.80 | (7.58) #15 |
| Shoulder flexion (°) | 11.99 | (12.01) #34567 | 12.27 | (14.88) #34567 | 26.60 | (10.43) #12456 | 44.31 | (16.47) #123567 | 52.30 | (22.02) #123467 | 35.16 | (12.64) #123457 | 29.12 | (14.70) #12456 |
| Shoulder abduction (°) | 13.17 | (10.65) #34567 | 12.93 | (6.06) #34567 | 50.34 | (15.97) #124567 | 21.70 | (17.44) #123567 | 23.62 | (13.33) #123467 | 28.97 | (12.97) #12345 | 28.63 | (14.69) #12345 |
| Elbow flexion (°) | 88.01 | (13.92) #123456 | 77.34 | (9.82) #134567 | 85.84 | (10.16) #124567 | 41.68 | (13.77) #123567 | 63.39 | (16.50) #1234 | 58.56 | (20.42) #1234 | 58.85 | (20.10) #1234 |
| Hip flexion (°) | 85.09 | (6.72) #2456 | 48.85 | (2.12) #134567 | 85.39 | (6.29) #2456 | 87.20 | (7.02) #12356 | 76.15 | (5.28) #123467 | 88.23 | (7.40) #123457 | 84.42 | (14.30) #256 |
| Hip abduction (°) | −1.61 | (13.35) #234567 | 0.00 | (0.00) #13467 | −6.84 | (7.93) #12567 | −6.26 | (6.30) #12567 | −1.28 | (10.36) #13467 | 26.94 | (6.67) #12345 | 22.84 | (12.42) #12345 |
| Hip rotation (°) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.40 | (5.65) | 0.00 | (0.00) |
| Knee flexion (°) | 88.74 | (5.29) #234567 | 0.00 | (0.00) #13467 | 86.61 | (4.90) #12567 | 87.03 | (4.90) #12567 | 73.10 | (9.78) #13467 | 90.78 | (5.37) #123457 | 134.42 | (7.51) #123456 |
| Frequency (%) | 34.0 | 1.1 | 15.5 | 19.2 | 10.4 | 15.2 | 4.7 | |||||||
Note: #X: statistically different from GPX with X between 1 and 7 for GP1 to GP7 (Kruskal-Wallis analysis, P < .05).
Abbreviation: GP1 to 7, Generic Posture 1 to 7.
RESULTS
The analysis of the dendrogram obtained from the HCA evidenced 7 “Generic Postures” (GP) from all measured joint angles (Figure 1). Each GP was defined by mean values and standard deviation of the 13 joint angles (Table 1).
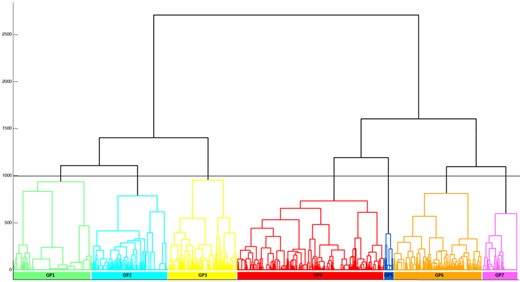
Ward’s minimum variance linkage dendrogram representing the seven-cluster solution of the hierarchical cluster analysis achieved from all measured postures during manual lymphatic drainage. The horizontal black line represents the cluster separation threshold. Each color represents a cluster of similar posture called “Generic Posture”.
The neck flexions ranged from 20 to 26°. GP1 (19.51 ± 11.61°) and GP4 (20.96 ± 8.89°) had the lowest flexion values, statistically lower than GP6 and GP7 (23.44 ± 6.95° and 25.48 ± 4.70°, respectively, P < .05). GP7 had the greatest flexion. The lowest neck inclination was recorded for GP1 (3.02 ± 4.19°, P < .05). GP3 and GP4 also had low inclinations (3.89 ± 4.73° and 3.38 ± 4.12°, respectively, P < .05). GP2, GP5 and GP7 had statistically three times higher values (12.01 ± 5.51°, 14.53 ± 13.51°, and 10.97 ± 6.67°, respectively, P < .05). Neck rotations were low (between 0° and 6°). GP1 has the highest value (5.75 ± 8.82°), which was statistically different from GP4, GP5, GP6, and GP7 (respectively 3.83 ± 5.58°, 2.54 ± 3.93°, 2.47 ± 2.79°, 3.71 ± 3.60°, P < .05).
About the trunk, flexion ranged from 15 to 25°. GP1, GP2, GP3, and GP4 had the lowest mean values, ranging from 14.58 ± 7.46° (GP1) to 16.58 ± 6.83° (GP2). GP5, GP6, and GP7 showed the statistically greatest mean flexions (21.02 ± 4.76°, 23.30 ± 7.81°, 23.32 ± 8.06°, respectively, P < .05). The same distribution was observed for inclination with values between 5.32 ± 4.02° and 8.20 ± 7.34° for GP1, GP2, GP3, and GP4 statistically lower than inclination for GP5, GP6, and GP7 (11.28 ± 9.93° to 16.50 ± 11.20°, P < .05).
GP1 and GP5 had values higher than 10°. GP5 presented the greatest rotation (14.96 ± 10.21°, P < .05). The other GPs had mean rotations of between 4 and 8°.
Wide differences have been highlighted for the shoulder. Mean flexion and abduction ranged from 10 to 55°. GP1 and GP2 had statistically the lowest values (respectively, 11.99 ± 12.01° and 12.27 ± 14.88° for flexion and 13.17 ± 10.65° and 12.93 ± 6.06° for abduction, P < .05). GP5 had the greatest shoulder flexion (52.30 ± 22.02°, P < .05) and GP3 the greatest abduction (50.34 ± 15.97°, P < .05).
For the elbow, flexion varied between 40 and 90°. GP4 had the lowest flexion (41.68 ± 13.77°, P < .05). GP2, GP3, and GP1 presented the highest values (77.34 ± 9.82°, 85.84 ± 10.16°, and 88.01 ± 13.92°, respectively, P < .05).
For the lower limb, the physiotherapists performed the massages in the seated position. GP1, GP3, GP4, GP6 were close to 90° for hip flexion (85.09 ± 6.72° to 88.23 ± 7.40°) and knee flexion (86.61 ± 4.90° to 90.78 ± 5.37°). GP7 had a hip flexion of 84.42 ± 14.30° but with greater knee flexion (134.42 ± 7.51°, P < .05). GP2 was characterized by lower hip and knee flexion of around 75° (76.15 ± 5.28° and 73.10 ± 9.78°, respectively, P < .05). Finally, for GP2, the posture was significantly different with the knee in a neutral position (0°) and a hip flexion of 48.85 ± 2.12° (P < .05). About hip rotations, postures were observed with the thighs in adduction (legs crossed for GP3 and GP4 with hip abduction <0°, P < .05) or in abduction (lower limbs apart for GP6 and GP7 with hip abduction of 26.94 ± 6.67° and 22.84 ± 12.42°, respectively, P < .05).
GP1 was the most used Generic Posture with a frequency of 34.0%. GP2 and GP7 had very low frequencies of use, at 1.1% and 4.7%, respectively. The 4 remaining GPs had an equivalent frequency of between 10 and 20% (Table 1).
Table 2 gives details of the RULA and REBA scores for all the GPs. GP1 had the lowest RULA score (4.46 ± 0.84, P < .05). GP2 and GP3 had slightly higher scores but were not significantly different (4.80 ± 0.40 and 4.93 ± 0.93, respectively, P > .05). These three GPs correspond to a low level of MSD risk for which changes can be envisaged (yellow color). GP5, GP6, and GP7 obtained the highest scores statistically greater than 5 (5.87 ± 0.98, 5.60 ± 1.09, and 5.63 ± 0.81, respectively, with GP5 significantly different from GP6 and GP7, P < .05). These GPs, as well as GP4, have a moderate risk of developing MSDs (orange color).
Detailed and mean (standard deviation) RULA and REBA scores by GP computed from all postures included in each GP.
| . | . | GP1 . | GP2 . | GP3 . | GP4 . | GP5 . | GP6 . | GP7 . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|
| RULA score distribution by GP | 1 | – | – | – | – | – | – | – | ||
| 2 | – | – | – | – | – | – | – | RULA level of MSD risk | ||
| 3 | 9.5% | – | 2.3% | 4.6% | - | 3.2% | 1.0% | 1–2 | Negligible risk. No action needed | |
| 4 | 47.6% | 20.3% | 40.6% | 23.8% | 16.8% | 17.5% | 12.3% | 3–4 | Low risk. Change may be needed | |
| 5 | 30.2% | 79.7% | 19.5% | 25.3% | 4.7% | 14.9% | 15.2% | 5–6 | Medium risk. Further investigation. change soon | |
| 6 | 12.6% | – | 37.4% | 39.8% | 53.1% | 44.3% | 66.1% | 6+ | High risk. Investigate and implement change now | |
| 7 | 0.1% | – | 0.2% | 6.5% | 25.4% | 20.0% | 5.5% | |||
| Mean RULA score | 4.46 (0.84)A | 4.80 (0.40)B | 4.93 (0.93)B | 5.20 (1.02)C | 5.87 (0.98)E | 5.60 (1.09)D | 5.63 (0.81)D | |||
| REBA score distribution by GP | 1 | – | – | – | – | – | – | – | ||
| 2 | – | – | – | – | – | – | – | |||
| 3 | 17.0% | – | 5.0% | – | 1.6% | 0.3% | 0.6% | |||
| 4 | 32.1% | 8.1% | 21.8% | 5.6% | 1.3% | 8.6% | 0.3% | REBA level of MSD risk | ||
| 5 | 17.2% | 45.9% | 27.7% | 34.7% | 29.8% | 21.1% | 12.3% | 1 | Negligible risk. No action needed | |
| 6 | 17.1% | 37.8% | 29.6% | 34.9% | 20.5% | 17.4% | 32.9% | 2–3 | Low risk. Change may be needed | |
| 7 | 0.4% | – | 0.2% | 8.3% | 1.3% | 3.1% | 3.2% | 4–7 | Medium risk. Further investigation. change soon | |
| 8 | 12.9% | 4.1% | 5.4% | 10.0% | 2.2% | 27.4% | 33.9% | 8–10 | High risk. Investigate and implement change | |
| 9 | 1.9% | 4.1% | 10.1% | 0.5% | 16.8% | 1.0% | 5.5% | 11+ | Very high risk. Implement change now | |
| 10 | 0.4% | – | 0.2% | 3.1% | 12.0% | 16.8% | 11.0% | |||
| 11 | 0.8% | – | – | 1.7% | 14.5% | 2.4% | 0.3% | |||
| 12 | – | – | – | 1.3% | – | 1.8% | – | |||
| Mean REBA score | 5.06 (1.75)A | 5.58 (1.07)B | 5.56 (1.60)B | 6.12 (1.57)C | 7.39 (2.39)E | 7.12 (2.12)D | 7.18 (1.59)D | |||
| . | . | GP1 . | GP2 . | GP3 . | GP4 . | GP5 . | GP6 . | GP7 . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|
| RULA score distribution by GP | 1 | – | – | – | – | – | – | – | ||
| 2 | – | – | – | – | – | – | – | RULA level of MSD risk | ||
| 3 | 9.5% | – | 2.3% | 4.6% | - | 3.2% | 1.0% | 1–2 | Negligible risk. No action needed | |
| 4 | 47.6% | 20.3% | 40.6% | 23.8% | 16.8% | 17.5% | 12.3% | 3–4 | Low risk. Change may be needed | |
| 5 | 30.2% | 79.7% | 19.5% | 25.3% | 4.7% | 14.9% | 15.2% | 5–6 | Medium risk. Further investigation. change soon | |
| 6 | 12.6% | – | 37.4% | 39.8% | 53.1% | 44.3% | 66.1% | 6+ | High risk. Investigate and implement change now | |
| 7 | 0.1% | – | 0.2% | 6.5% | 25.4% | 20.0% | 5.5% | |||
| Mean RULA score | 4.46 (0.84)A | 4.80 (0.40)B | 4.93 (0.93)B | 5.20 (1.02)C | 5.87 (0.98)E | 5.60 (1.09)D | 5.63 (0.81)D | |||
| REBA score distribution by GP | 1 | – | – | – | – | – | – | – | ||
| 2 | – | – | – | – | – | – | – | |||
| 3 | 17.0% | – | 5.0% | – | 1.6% | 0.3% | 0.6% | |||
| 4 | 32.1% | 8.1% | 21.8% | 5.6% | 1.3% | 8.6% | 0.3% | REBA level of MSD risk | ||
| 5 | 17.2% | 45.9% | 27.7% | 34.7% | 29.8% | 21.1% | 12.3% | 1 | Negligible risk. No action needed | |
| 6 | 17.1% | 37.8% | 29.6% | 34.9% | 20.5% | 17.4% | 32.9% | 2–3 | Low risk. Change may be needed | |
| 7 | 0.4% | – | 0.2% | 8.3% | 1.3% | 3.1% | 3.2% | 4–7 | Medium risk. Further investigation. change soon | |
| 8 | 12.9% | 4.1% | 5.4% | 10.0% | 2.2% | 27.4% | 33.9% | 8–10 | High risk. Investigate and implement change | |
| 9 | 1.9% | 4.1% | 10.1% | 0.5% | 16.8% | 1.0% | 5.5% | 11+ | Very high risk. Implement change now | |
| 10 | 0.4% | – | 0.2% | 3.1% | 12.0% | 16.8% | 11.0% | |||
| 11 | 0.8% | – | – | 1.7% | 14.5% | 2.4% | 0.3% | |||
| 12 | – | – | – | 1.3% | – | 1.8% | – | |||
| Mean REBA score | 5.06 (1.75)A | 5.58 (1.07)B | 5.56 (1.60)B | 6.12 (1.57)C | 7.39 (2.39)E | 7.12 (2.12)D | 7.18 (1.59)D | |||
Note: A,B,C,D,E: values with the same exponent are not significantly different from each other but are different from other values (Kruskal-Wallis analysis, P < .05, independently for RULA and REBA scores).
Detailed and mean (standard deviation) RULA and REBA scores by GP computed from all postures included in each GP.
| . | . | GP1 . | GP2 . | GP3 . | GP4 . | GP5 . | GP6 . | GP7 . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|
| RULA score distribution by GP | 1 | – | – | – | – | – | – | – | ||
| 2 | – | – | – | – | – | – | – | RULA level of MSD risk | ||
| 3 | 9.5% | – | 2.3% | 4.6% | - | 3.2% | 1.0% | 1–2 | Negligible risk. No action needed | |
| 4 | 47.6% | 20.3% | 40.6% | 23.8% | 16.8% | 17.5% | 12.3% | 3–4 | Low risk. Change may be needed | |
| 5 | 30.2% | 79.7% | 19.5% | 25.3% | 4.7% | 14.9% | 15.2% | 5–6 | Medium risk. Further investigation. change soon | |
| 6 | 12.6% | – | 37.4% | 39.8% | 53.1% | 44.3% | 66.1% | 6+ | High risk. Investigate and implement change now | |
| 7 | 0.1% | – | 0.2% | 6.5% | 25.4% | 20.0% | 5.5% | |||
| Mean RULA score | 4.46 (0.84)A | 4.80 (0.40)B | 4.93 (0.93)B | 5.20 (1.02)C | 5.87 (0.98)E | 5.60 (1.09)D | 5.63 (0.81)D | |||
| REBA score distribution by GP | 1 | – | – | – | – | – | – | – | ||
| 2 | – | – | – | – | – | – | – | |||
| 3 | 17.0% | – | 5.0% | – | 1.6% | 0.3% | 0.6% | |||
| 4 | 32.1% | 8.1% | 21.8% | 5.6% | 1.3% | 8.6% | 0.3% | REBA level of MSD risk | ||
| 5 | 17.2% | 45.9% | 27.7% | 34.7% | 29.8% | 21.1% | 12.3% | 1 | Negligible risk. No action needed | |
| 6 | 17.1% | 37.8% | 29.6% | 34.9% | 20.5% | 17.4% | 32.9% | 2–3 | Low risk. Change may be needed | |
| 7 | 0.4% | – | 0.2% | 8.3% | 1.3% | 3.1% | 3.2% | 4–7 | Medium risk. Further investigation. change soon | |
| 8 | 12.9% | 4.1% | 5.4% | 10.0% | 2.2% | 27.4% | 33.9% | 8–10 | High risk. Investigate and implement change | |
| 9 | 1.9% | 4.1% | 10.1% | 0.5% | 16.8% | 1.0% | 5.5% | 11+ | Very high risk. Implement change now | |
| 10 | 0.4% | – | 0.2% | 3.1% | 12.0% | 16.8% | 11.0% | |||
| 11 | 0.8% | – | – | 1.7% | 14.5% | 2.4% | 0.3% | |||
| 12 | – | – | – | 1.3% | – | 1.8% | – | |||
| Mean REBA score | 5.06 (1.75)A | 5.58 (1.07)B | 5.56 (1.60)B | 6.12 (1.57)C | 7.39 (2.39)E | 7.12 (2.12)D | 7.18 (1.59)D | |||
| . | . | GP1 . | GP2 . | GP3 . | GP4 . | GP5 . | GP6 . | GP7 . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|
| RULA score distribution by GP | 1 | – | – | – | – | – | – | – | ||
| 2 | – | – | – | – | – | – | – | RULA level of MSD risk | ||
| 3 | 9.5% | – | 2.3% | 4.6% | - | 3.2% | 1.0% | 1–2 | Negligible risk. No action needed | |
| 4 | 47.6% | 20.3% | 40.6% | 23.8% | 16.8% | 17.5% | 12.3% | 3–4 | Low risk. Change may be needed | |
| 5 | 30.2% | 79.7% | 19.5% | 25.3% | 4.7% | 14.9% | 15.2% | 5–6 | Medium risk. Further investigation. change soon | |
| 6 | 12.6% | – | 37.4% | 39.8% | 53.1% | 44.3% | 66.1% | 6+ | High risk. Investigate and implement change now | |
| 7 | 0.1% | – | 0.2% | 6.5% | 25.4% | 20.0% | 5.5% | |||
| Mean RULA score | 4.46 (0.84)A | 4.80 (0.40)B | 4.93 (0.93)B | 5.20 (1.02)C | 5.87 (0.98)E | 5.60 (1.09)D | 5.63 (0.81)D | |||
| REBA score distribution by GP | 1 | – | – | – | – | – | – | – | ||
| 2 | – | – | – | – | – | – | – | |||
| 3 | 17.0% | – | 5.0% | – | 1.6% | 0.3% | 0.6% | |||
| 4 | 32.1% | 8.1% | 21.8% | 5.6% | 1.3% | 8.6% | 0.3% | REBA level of MSD risk | ||
| 5 | 17.2% | 45.9% | 27.7% | 34.7% | 29.8% | 21.1% | 12.3% | 1 | Negligible risk. No action needed | |
| 6 | 17.1% | 37.8% | 29.6% | 34.9% | 20.5% | 17.4% | 32.9% | 2–3 | Low risk. Change may be needed | |
| 7 | 0.4% | – | 0.2% | 8.3% | 1.3% | 3.1% | 3.2% | 4–7 | Medium risk. Further investigation. change soon | |
| 8 | 12.9% | 4.1% | 5.4% | 10.0% | 2.2% | 27.4% | 33.9% | 8–10 | High risk. Investigate and implement change | |
| 9 | 1.9% | 4.1% | 10.1% | 0.5% | 16.8% | 1.0% | 5.5% | 11+ | Very high risk. Implement change now | |
| 10 | 0.4% | – | 0.2% | 3.1% | 12.0% | 16.8% | 11.0% | |||
| 11 | 0.8% | – | – | 1.7% | 14.5% | 2.4% | 0.3% | |||
| 12 | – | – | – | 1.3% | – | 1.8% | – | |||
| Mean REBA score | 5.06 (1.75)A | 5.58 (1.07)B | 5.56 (1.60)B | 6.12 (1.57)C | 7.39 (2.39)E | 7.12 (2.12)D | 7.18 (1.59)D | |||
Note: A,B,C,D,E: values with the same exponent are not significantly different from each other but are different from other values (Kruskal-Wallis analysis, P < .05, independently for RULA and REBA scores).
For REBA, all GPs are at level 3 risk of MSD (score from 4 to 7), that is, moderate risk requiring further investigation and change soon. As with RULA, GP1 presented the lowest REBA score (5.06 ± 1.75, P < .05). GP2 and GP3 had slightly higher scores but were not significantly different (5.58 ± 1.07 and 5.56 ± 1.60, respectively, P > .05). GP5, GP6, and GP7 had the statistically highest scores with values above 7 (7.39 ± 2.39, 7.12 ± 2.12, and 7.18 ± 1.59 with GP5 significantly different from GP6 and GP7, P < .05).
Table 3 presents the combination of GPs used for each of the 25 massages and their frequency of use. Three massages used only one GP (M10: 100% GP6; M18: 100% GP6; M19: 100% GP7). Some other massages used a main GP with a high frequency (>75%) supplemented by others with lower frequencies. This was the case for M1, M2, M6, M7 (GP1: 76.2%, 88.8%, 83.0%, 91.2%, respectively), for M4 (GP4: 74.2%), M17 (GP6: 92.1%) and M22 (GP5: 88.3%). The other massages used several GPs more consistently. For each massage, the RULA and REBA scores were computed from all massage postures and from mean scores of each GP used (Table 2) to estimate the risk of MSDs. Figure 2 illustrates the relationship between GP frequency and RULA/REBA scores per massage.
| . | . | M1 . | M2 . | M3 . | M4 . | M5 . | M6 . | M7 . | M8 . | M9 . | M10 . | M11 . | M12 . | M13 . | M14 . | M15 . | M16 . | M17 . | M18 . | M19 . | M20 . | M21 . | M22 . | M23 . | M24 . | M25 . | RR . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP1 | Freq. (%) | 76.2 | 88.8 | 1.0 | 0.0 | 6.4 | 83.0 | 91.2 | 22.7 | 55.1 | 0.0 | 28.6 | 60.1 | 51.5 | 39.1 | 42.4 | 11.6 | 2.1 | 0.0 | 0.0 | 14.0 | 9.6 | 0.6 | 36.2 | 65.2 | 38.0 | |
| RULA | 4.3 | 3.9 | 4.7 | 0 | 6.0 | 5.8 | 3.9 | 5.9 | 5.0 | 0 | 4.9 | 5.0 | 4.0 | 4.3 | 3.9 | 4.4 | 4.0 | 0 | 0 | 4.4 | 4.3 | 4.0 | 4.7 | 5.1 | 4.0 | 4.5 | |
| REBA | 5.1 | 3.6 | 5.7 | 0 | 10.6 | 7.8 | 4.4 | 7.0 | 6.0 | 0 | 4.4 | 7.7 | 4.2 | 3.9 | 4.0 | 4.9 | 3.7 | 0 | 0 | 4.9 | 4.3 | 5.0 | 5.3 | 6.2 | 3.5 | 5.1 | |
| GP2 | Freq. (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 21.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 7.4 | |
| RULA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.1 | 4.8 | |
| REBA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.8 | 5.6 | |
| GP3 | Freq. (%) | 4.1 | 0.5 | 25.9 | 25.8 | 70.3 | 0.0 | 1.8 | 23.1 | 1.6 | 0.0 | 41.8 | 8.5 | 0.0 | 0.0 | 5.1 | 20.6 | 2.9 | 0.0 | 0.0 | 6.1 | 67.8 | 1.7 | 10.5 | 7.6 | 14.8 | |
| RULA | 3.9 | 6.0 | 4.4 | 4.0 | 5.3 | 0 | 4.0 | 6.0 | 6.0 | 0 | 5.2 | 6.0 | 0 | 0 | 5.0 | 5.0 | 5.0 | 0 | 0 | 5.6 | 4.4 | 6.3 | 5.7 | 6.0 | 4.1 | 4.9 | |
| REBA | 3.6 | 5.0 | 5.4 | 4.0 | 7.0 | 0 | 4.1 | 6.4 | 5.0 | 0 | 5.0 | 8.0 | 0 | 0 | 6.0 | 4.9 | 6.0 | 0 | 0 | 5.3 | 4.9 | 8.3 | 5.8 | 6.0 | 4.5 | 5.6 | |
| GP4 | Freq. (%) | 16.0 | 0.5 | 10.4 | 74.2 | 23.2 | 17.0 | 7.1 | 7.0 | 43.3 | 0.0 | 0.7 | 10.3 | 25.5 | 42.7 | 2.0 | 35.4 | 1.4 | 0.0 | 0.0 | 10.5 | 21.4 | 9.4 | 53.3 | 27.2 | 34.1 | |
| RULA | 3.1 | 6.0 | 4.8 | 4.4 | 5.5 | 6.3 | 4.6 | 4.0 | 6.0 | 0 | 6.0 | 5.7 | 5.0 | 5.1 | 6.0 | 5.7 | 4.5 | 0 | 0 | 6.1 | 5.7 | 6.1 | 5.7 | 6.3 | 4.9 | 5.2 | |
| REBA | 4.9 | 5.0 | 6.0 | 5.5 | 7.7 | 8.5 | 5.8 | 5.0 | 5.2 | 0 | 8.0 | 6.5 | 5.7 | 4.8 | 7.0 | 6.4 | 5.0 | 0 | 0 | 8.8 | 6.7 | 7.8 | 6.8 | 6.9 | 5.9 | 6.1 | |
| GP5 | Freq. (%) | 1.6 | 0.0 | 62.8 | 0.0 | 0.0 | 0.0 | 0.0 | 47.3 | 0.0 | 0.0 | 3.4 | 0.0 | 0.0 | 3.4 | 0.0 | 4.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 88.3 | 0.0 | 0.0 | 5.7 | |
| RULA | 4.5 | 0 | 5.0 | 0 | 0 | 0 | 0 | 7.0 | 0 | 0 | 6.0 | 0 | 0 | 4.7 | 0 | 6.4 | 0 | 0 | 0 | 0 | 0 | 6.1 | 0 | 0 | 4.4 | 5.9 | |
| REBA | 5.3 | 0 | 5.0 | 0 | 0 | 0 | 0 | 6.1 | 0 | 0 | 9.8 | 0 | 0 | 3.8 | 0 | 7.7 | 0 | 0 | 0 | 0 | 0 | 9.6 | 0 | 0 | 4.2 | 7.4 | |
| GP6 | Freq. (%) | 2.0 | 10.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 0.0 | 0.0 | 23.0 | 14.8 | 40.4 | 17.7 | 92.1 | 100.0 | 0.0 | 69.4 | 1.2 | 0.0 | 0.0 | 0.0 | 0.0 | |
| RULA | 4.2 | 4.6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6.2 | 0 | 0 | 4.6 | 4.4 | 4.1 | 6.4 | 5.8 | 5.6 | 0 | 6.5 | 4.0 | 0 | 0 | 0 | 0 | 5.6 | |
| REBA | 5.6 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7.7 | 0 | 0 | 5.6 | 5.4 | 5.0 | 8.4 | 7.4 | 6.7 | 0 | 9.0 | 4.0 | 0 | 0 | 0 | 0 | 7.1 | |
| GP7 | Freq. (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 25.5 | 0.0 | 0.0 | 0.0 | 10.2 | 10.8 | 1.4 | 0.0 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| RULA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.9 | 0 | 0 | 0 | 5.2 | 5.2 | 5.0 | 0 | 6.1 | 0 | 0 | 0 | 0 | 0 | 0 | 5.6 | |
| REBA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6.0 | 0 | 0 | 0 | 6.0 | 7.2 | 5.0 | 0 | 7.9 | 0 | 0 | 0 | 0 | 0 | 0 | 7.2 | |
| Mean RULA score from all postures$ | 4.11A | 4.03A | 4.82B | 4.29A | 5.41B | 5.90C | 3.98A | 6.30C | 5.44B | 6.20C | 3.85B | 5.16B | 4.40A | 4.65A | 3.71A | 4.95B | 5.63B | 5.62B | 6.06C | 6.09C | 4.64B | 6.07C | 5.30B | 5.46B | 4.37A | ||
| Mean REBA score from all postures$ | 5.05C | 3.78A | 5.21C | 5.09C | 7.39D | 7.96E | 4.48B | 6.29E | 5.65D | 7.69E | 5.27C | 7.22D | 4.88B | 4.51B | 4.79B | 6.40D | 7.21E | 6.71D | 7.86E | 8.19E | 5.22C | 9.42E | 6.19D | 6.39D | 4.62B | ||
| Mean RULA Score from GP# | 4.64 | 4.58 | 5.54 | 5.13 | 4.96 | 4.59 | 4.52 | 5.29 | 4.79 | 5.60 | 5.01 | 4.65 | 4.91 | 4.99 | 5.08 | 5.20 | 5.55 | 5.60 | 5.63 | 5.36 | 4.95 | 5.78 | 4.90 | 4.70 | 4.89 | ||
| Mean REBA Score from GP# | 5.33 | 5.28 | 6.76 | 5.98 | 5.66 | 5.24 | 5.14 | 6.35 | 5.53 | 7.12 | 5.90 | 5.32 | 5.80 | 5.90 | 6.15 | 6.22 | 7.02 | 7.12 | 7.18 | 6.63 | 5.65 | 7.23 | 5.68 | 5.39 | 5.67 | ||
| . | . | M1 . | M2 . | M3 . | M4 . | M5 . | M6 . | M7 . | M8 . | M9 . | M10 . | M11 . | M12 . | M13 . | M14 . | M15 . | M16 . | M17 . | M18 . | M19 . | M20 . | M21 . | M22 . | M23 . | M24 . | M25 . | RR . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP1 | Freq. (%) | 76.2 | 88.8 | 1.0 | 0.0 | 6.4 | 83.0 | 91.2 | 22.7 | 55.1 | 0.0 | 28.6 | 60.1 | 51.5 | 39.1 | 42.4 | 11.6 | 2.1 | 0.0 | 0.0 | 14.0 | 9.6 | 0.6 | 36.2 | 65.2 | 38.0 | |
| RULA | 4.3 | 3.9 | 4.7 | 0 | 6.0 | 5.8 | 3.9 | 5.9 | 5.0 | 0 | 4.9 | 5.0 | 4.0 | 4.3 | 3.9 | 4.4 | 4.0 | 0 | 0 | 4.4 | 4.3 | 4.0 | 4.7 | 5.1 | 4.0 | 4.5 | |
| REBA | 5.1 | 3.6 | 5.7 | 0 | 10.6 | 7.8 | 4.4 | 7.0 | 6.0 | 0 | 4.4 | 7.7 | 4.2 | 3.9 | 4.0 | 4.9 | 3.7 | 0 | 0 | 4.9 | 4.3 | 5.0 | 5.3 | 6.2 | 3.5 | 5.1 | |
| GP2 | Freq. (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 21.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 7.4 | |
| RULA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.1 | 4.8 | |
| REBA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.8 | 5.6 | |
| GP3 | Freq. (%) | 4.1 | 0.5 | 25.9 | 25.8 | 70.3 | 0.0 | 1.8 | 23.1 | 1.6 | 0.0 | 41.8 | 8.5 | 0.0 | 0.0 | 5.1 | 20.6 | 2.9 | 0.0 | 0.0 | 6.1 | 67.8 | 1.7 | 10.5 | 7.6 | 14.8 | |
| RULA | 3.9 | 6.0 | 4.4 | 4.0 | 5.3 | 0 | 4.0 | 6.0 | 6.0 | 0 | 5.2 | 6.0 | 0 | 0 | 5.0 | 5.0 | 5.0 | 0 | 0 | 5.6 | 4.4 | 6.3 | 5.7 | 6.0 | 4.1 | 4.9 | |
| REBA | 3.6 | 5.0 | 5.4 | 4.0 | 7.0 | 0 | 4.1 | 6.4 | 5.0 | 0 | 5.0 | 8.0 | 0 | 0 | 6.0 | 4.9 | 6.0 | 0 | 0 | 5.3 | 4.9 | 8.3 | 5.8 | 6.0 | 4.5 | 5.6 | |
| GP4 | Freq. (%) | 16.0 | 0.5 | 10.4 | 74.2 | 23.2 | 17.0 | 7.1 | 7.0 | 43.3 | 0.0 | 0.7 | 10.3 | 25.5 | 42.7 | 2.0 | 35.4 | 1.4 | 0.0 | 0.0 | 10.5 | 21.4 | 9.4 | 53.3 | 27.2 | 34.1 | |
| RULA | 3.1 | 6.0 | 4.8 | 4.4 | 5.5 | 6.3 | 4.6 | 4.0 | 6.0 | 0 | 6.0 | 5.7 | 5.0 | 5.1 | 6.0 | 5.7 | 4.5 | 0 | 0 | 6.1 | 5.7 | 6.1 | 5.7 | 6.3 | 4.9 | 5.2 | |
| REBA | 4.9 | 5.0 | 6.0 | 5.5 | 7.7 | 8.5 | 5.8 | 5.0 | 5.2 | 0 | 8.0 | 6.5 | 5.7 | 4.8 | 7.0 | 6.4 | 5.0 | 0 | 0 | 8.8 | 6.7 | 7.8 | 6.8 | 6.9 | 5.9 | 6.1 | |
| GP5 | Freq. (%) | 1.6 | 0.0 | 62.8 | 0.0 | 0.0 | 0.0 | 0.0 | 47.3 | 0.0 | 0.0 | 3.4 | 0.0 | 0.0 | 3.4 | 0.0 | 4.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 88.3 | 0.0 | 0.0 | 5.7 | |
| RULA | 4.5 | 0 | 5.0 | 0 | 0 | 0 | 0 | 7.0 | 0 | 0 | 6.0 | 0 | 0 | 4.7 | 0 | 6.4 | 0 | 0 | 0 | 0 | 0 | 6.1 | 0 | 0 | 4.4 | 5.9 | |
| REBA | 5.3 | 0 | 5.0 | 0 | 0 | 0 | 0 | 6.1 | 0 | 0 | 9.8 | 0 | 0 | 3.8 | 0 | 7.7 | 0 | 0 | 0 | 0 | 0 | 9.6 | 0 | 0 | 4.2 | 7.4 | |
| GP6 | Freq. (%) | 2.0 | 10.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 0.0 | 0.0 | 23.0 | 14.8 | 40.4 | 17.7 | 92.1 | 100.0 | 0.0 | 69.4 | 1.2 | 0.0 | 0.0 | 0.0 | 0.0 | |
| RULA | 4.2 | 4.6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6.2 | 0 | 0 | 4.6 | 4.4 | 4.1 | 6.4 | 5.8 | 5.6 | 0 | 6.5 | 4.0 | 0 | 0 | 0 | 0 | 5.6 | |
| REBA | 5.6 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7.7 | 0 | 0 | 5.6 | 5.4 | 5.0 | 8.4 | 7.4 | 6.7 | 0 | 9.0 | 4.0 | 0 | 0 | 0 | 0 | 7.1 | |
| GP7 | Freq. (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 25.5 | 0.0 | 0.0 | 0.0 | 10.2 | 10.8 | 1.4 | 0.0 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| RULA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.9 | 0 | 0 | 0 | 5.2 | 5.2 | 5.0 | 0 | 6.1 | 0 | 0 | 0 | 0 | 0 | 0 | 5.6 | |
| REBA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6.0 | 0 | 0 | 0 | 6.0 | 7.2 | 5.0 | 0 | 7.9 | 0 | 0 | 0 | 0 | 0 | 0 | 7.2 | |
| Mean RULA score from all postures$ | 4.11A | 4.03A | 4.82B | 4.29A | 5.41B | 5.90C | 3.98A | 6.30C | 5.44B | 6.20C | 3.85B | 5.16B | 4.40A | 4.65A | 3.71A | 4.95B | 5.63B | 5.62B | 6.06C | 6.09C | 4.64B | 6.07C | 5.30B | 5.46B | 4.37A | ||
| Mean REBA score from all postures$ | 5.05C | 3.78A | 5.21C | 5.09C | 7.39D | 7.96E | 4.48B | 6.29E | 5.65D | 7.69E | 5.27C | 7.22D | 4.88B | 4.51B | 4.79B | 6.40D | 7.21E | 6.71D | 7.86E | 8.19E | 5.22C | 9.42E | 6.19D | 6.39D | 4.62B | ||
| Mean RULA Score from GP# | 4.64 | 4.58 | 5.54 | 5.13 | 4.96 | 4.59 | 4.52 | 5.29 | 4.79 | 5.60 | 5.01 | 4.65 | 4.91 | 4.99 | 5.08 | 5.20 | 5.55 | 5.60 | 5.63 | 5.36 | 4.95 | 5.78 | 4.90 | 4.70 | 4.89 | ||
| Mean REBA Score from GP# | 5.33 | 5.28 | 6.76 | 5.98 | 5.66 | 5.24 | 5.14 | 6.35 | 5.53 | 7.12 | 5.90 | 5.32 | 5.80 | 5.90 | 6.15 | 6.22 | 7.02 | 7.12 | 7.18 | 6.63 | 5.65 | 7.23 | 5.68 | 5.39 | 5.67 | ||
Note: The gray values represent the GP frequency that composed each massage. Mean RULA and REBA scores were presented form all postures (horizontally in white) and from GP relative scores (horizontally in blue) presented vertically on the right. A,B,C,D,E: values with the same exponent are not significantly different from each other but are different from other values (Kruskal-Wallis analysis, P < .05, independently for RULA and REBA).
| . | . | M1 . | M2 . | M3 . | M4 . | M5 . | M6 . | M7 . | M8 . | M9 . | M10 . | M11 . | M12 . | M13 . | M14 . | M15 . | M16 . | M17 . | M18 . | M19 . | M20 . | M21 . | M22 . | M23 . | M24 . | M25 . | RR . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP1 | Freq. (%) | 76.2 | 88.8 | 1.0 | 0.0 | 6.4 | 83.0 | 91.2 | 22.7 | 55.1 | 0.0 | 28.6 | 60.1 | 51.5 | 39.1 | 42.4 | 11.6 | 2.1 | 0.0 | 0.0 | 14.0 | 9.6 | 0.6 | 36.2 | 65.2 | 38.0 | |
| RULA | 4.3 | 3.9 | 4.7 | 0 | 6.0 | 5.8 | 3.9 | 5.9 | 5.0 | 0 | 4.9 | 5.0 | 4.0 | 4.3 | 3.9 | 4.4 | 4.0 | 0 | 0 | 4.4 | 4.3 | 4.0 | 4.7 | 5.1 | 4.0 | 4.5 | |
| REBA | 5.1 | 3.6 | 5.7 | 0 | 10.6 | 7.8 | 4.4 | 7.0 | 6.0 | 0 | 4.4 | 7.7 | 4.2 | 3.9 | 4.0 | 4.9 | 3.7 | 0 | 0 | 4.9 | 4.3 | 5.0 | 5.3 | 6.2 | 3.5 | 5.1 | |
| GP2 | Freq. (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 21.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 7.4 | |
| RULA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.1 | 4.8 | |
| REBA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.8 | 5.6 | |
| GP3 | Freq. (%) | 4.1 | 0.5 | 25.9 | 25.8 | 70.3 | 0.0 | 1.8 | 23.1 | 1.6 | 0.0 | 41.8 | 8.5 | 0.0 | 0.0 | 5.1 | 20.6 | 2.9 | 0.0 | 0.0 | 6.1 | 67.8 | 1.7 | 10.5 | 7.6 | 14.8 | |
| RULA | 3.9 | 6.0 | 4.4 | 4.0 | 5.3 | 0 | 4.0 | 6.0 | 6.0 | 0 | 5.2 | 6.0 | 0 | 0 | 5.0 | 5.0 | 5.0 | 0 | 0 | 5.6 | 4.4 | 6.3 | 5.7 | 6.0 | 4.1 | 4.9 | |
| REBA | 3.6 | 5.0 | 5.4 | 4.0 | 7.0 | 0 | 4.1 | 6.4 | 5.0 | 0 | 5.0 | 8.0 | 0 | 0 | 6.0 | 4.9 | 6.0 | 0 | 0 | 5.3 | 4.9 | 8.3 | 5.8 | 6.0 | 4.5 | 5.6 | |
| GP4 | Freq. (%) | 16.0 | 0.5 | 10.4 | 74.2 | 23.2 | 17.0 | 7.1 | 7.0 | 43.3 | 0.0 | 0.7 | 10.3 | 25.5 | 42.7 | 2.0 | 35.4 | 1.4 | 0.0 | 0.0 | 10.5 | 21.4 | 9.4 | 53.3 | 27.2 | 34.1 | |
| RULA | 3.1 | 6.0 | 4.8 | 4.4 | 5.5 | 6.3 | 4.6 | 4.0 | 6.0 | 0 | 6.0 | 5.7 | 5.0 | 5.1 | 6.0 | 5.7 | 4.5 | 0 | 0 | 6.1 | 5.7 | 6.1 | 5.7 | 6.3 | 4.9 | 5.2 | |
| REBA | 4.9 | 5.0 | 6.0 | 5.5 | 7.7 | 8.5 | 5.8 | 5.0 | 5.2 | 0 | 8.0 | 6.5 | 5.7 | 4.8 | 7.0 | 6.4 | 5.0 | 0 | 0 | 8.8 | 6.7 | 7.8 | 6.8 | 6.9 | 5.9 | 6.1 | |
| GP5 | Freq. (%) | 1.6 | 0.0 | 62.8 | 0.0 | 0.0 | 0.0 | 0.0 | 47.3 | 0.0 | 0.0 | 3.4 | 0.0 | 0.0 | 3.4 | 0.0 | 4.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 88.3 | 0.0 | 0.0 | 5.7 | |
| RULA | 4.5 | 0 | 5.0 | 0 | 0 | 0 | 0 | 7.0 | 0 | 0 | 6.0 | 0 | 0 | 4.7 | 0 | 6.4 | 0 | 0 | 0 | 0 | 0 | 6.1 | 0 | 0 | 4.4 | 5.9 | |
| REBA | 5.3 | 0 | 5.0 | 0 | 0 | 0 | 0 | 6.1 | 0 | 0 | 9.8 | 0 | 0 | 3.8 | 0 | 7.7 | 0 | 0 | 0 | 0 | 0 | 9.6 | 0 | 0 | 4.2 | 7.4 | |
| GP6 | Freq. (%) | 2.0 | 10.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 0.0 | 0.0 | 23.0 | 14.8 | 40.4 | 17.7 | 92.1 | 100.0 | 0.0 | 69.4 | 1.2 | 0.0 | 0.0 | 0.0 | 0.0 | |
| RULA | 4.2 | 4.6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6.2 | 0 | 0 | 4.6 | 4.4 | 4.1 | 6.4 | 5.8 | 5.6 | 0 | 6.5 | 4.0 | 0 | 0 | 0 | 0 | 5.6 | |
| REBA | 5.6 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7.7 | 0 | 0 | 5.6 | 5.4 | 5.0 | 8.4 | 7.4 | 6.7 | 0 | 9.0 | 4.0 | 0 | 0 | 0 | 0 | 7.1 | |
| GP7 | Freq. (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 25.5 | 0.0 | 0.0 | 0.0 | 10.2 | 10.8 | 1.4 | 0.0 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| RULA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.9 | 0 | 0 | 0 | 5.2 | 5.2 | 5.0 | 0 | 6.1 | 0 | 0 | 0 | 0 | 0 | 0 | 5.6 | |
| REBA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6.0 | 0 | 0 | 0 | 6.0 | 7.2 | 5.0 | 0 | 7.9 | 0 | 0 | 0 | 0 | 0 | 0 | 7.2 | |
| Mean RULA score from all postures$ | 4.11A | 4.03A | 4.82B | 4.29A | 5.41B | 5.90C | 3.98A | 6.30C | 5.44B | 6.20C | 3.85B | 5.16B | 4.40A | 4.65A | 3.71A | 4.95B | 5.63B | 5.62B | 6.06C | 6.09C | 4.64B | 6.07C | 5.30B | 5.46B | 4.37A | ||
| Mean REBA score from all postures$ | 5.05C | 3.78A | 5.21C | 5.09C | 7.39D | 7.96E | 4.48B | 6.29E | 5.65D | 7.69E | 5.27C | 7.22D | 4.88B | 4.51B | 4.79B | 6.40D | 7.21E | 6.71D | 7.86E | 8.19E | 5.22C | 9.42E | 6.19D | 6.39D | 4.62B | ||
| Mean RULA Score from GP# | 4.64 | 4.58 | 5.54 | 5.13 | 4.96 | 4.59 | 4.52 | 5.29 | 4.79 | 5.60 | 5.01 | 4.65 | 4.91 | 4.99 | 5.08 | 5.20 | 5.55 | 5.60 | 5.63 | 5.36 | 4.95 | 5.78 | 4.90 | 4.70 | 4.89 | ||
| Mean REBA Score from GP# | 5.33 | 5.28 | 6.76 | 5.98 | 5.66 | 5.24 | 5.14 | 6.35 | 5.53 | 7.12 | 5.90 | 5.32 | 5.80 | 5.90 | 6.15 | 6.22 | 7.02 | 7.12 | 7.18 | 6.63 | 5.65 | 7.23 | 5.68 | 5.39 | 5.67 | ||
| . | . | M1 . | M2 . | M3 . | M4 . | M5 . | M6 . | M7 . | M8 . | M9 . | M10 . | M11 . | M12 . | M13 . | M14 . | M15 . | M16 . | M17 . | M18 . | M19 . | M20 . | M21 . | M22 . | M23 . | M24 . | M25 . | RR . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP1 | Freq. (%) | 76.2 | 88.8 | 1.0 | 0.0 | 6.4 | 83.0 | 91.2 | 22.7 | 55.1 | 0.0 | 28.6 | 60.1 | 51.5 | 39.1 | 42.4 | 11.6 | 2.1 | 0.0 | 0.0 | 14.0 | 9.6 | 0.6 | 36.2 | 65.2 | 38.0 | |
| RULA | 4.3 | 3.9 | 4.7 | 0 | 6.0 | 5.8 | 3.9 | 5.9 | 5.0 | 0 | 4.9 | 5.0 | 4.0 | 4.3 | 3.9 | 4.4 | 4.0 | 0 | 0 | 4.4 | 4.3 | 4.0 | 4.7 | 5.1 | 4.0 | 4.5 | |
| REBA | 5.1 | 3.6 | 5.7 | 0 | 10.6 | 7.8 | 4.4 | 7.0 | 6.0 | 0 | 4.4 | 7.7 | 4.2 | 3.9 | 4.0 | 4.9 | 3.7 | 0 | 0 | 4.9 | 4.3 | 5.0 | 5.3 | 6.2 | 3.5 | 5.1 | |
| GP2 | Freq. (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 21.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 7.4 | |
| RULA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.1 | 4.8 | |
| REBA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5.8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.8 | 5.6 | |
| GP3 | Freq. (%) | 4.1 | 0.5 | 25.9 | 25.8 | 70.3 | 0.0 | 1.8 | 23.1 | 1.6 | 0.0 | 41.8 | 8.5 | 0.0 | 0.0 | 5.1 | 20.6 | 2.9 | 0.0 | 0.0 | 6.1 | 67.8 | 1.7 | 10.5 | 7.6 | 14.8 | |
| RULA | 3.9 | 6.0 | 4.4 | 4.0 | 5.3 | 0 | 4.0 | 6.0 | 6.0 | 0 | 5.2 | 6.0 | 0 | 0 | 5.0 | 5.0 | 5.0 | 0 | 0 | 5.6 | 4.4 | 6.3 | 5.7 | 6.0 | 4.1 | 4.9 | |
| REBA | 3.6 | 5.0 | 5.4 | 4.0 | 7.0 | 0 | 4.1 | 6.4 | 5.0 | 0 | 5.0 | 8.0 | 0 | 0 | 6.0 | 4.9 | 6.0 | 0 | 0 | 5.3 | 4.9 | 8.3 | 5.8 | 6.0 | 4.5 | 5.6 | |
| GP4 | Freq. (%) | 16.0 | 0.5 | 10.4 | 74.2 | 23.2 | 17.0 | 7.1 | 7.0 | 43.3 | 0.0 | 0.7 | 10.3 | 25.5 | 42.7 | 2.0 | 35.4 | 1.4 | 0.0 | 0.0 | 10.5 | 21.4 | 9.4 | 53.3 | 27.2 | 34.1 | |
| RULA | 3.1 | 6.0 | 4.8 | 4.4 | 5.5 | 6.3 | 4.6 | 4.0 | 6.0 | 0 | 6.0 | 5.7 | 5.0 | 5.1 | 6.0 | 5.7 | 4.5 | 0 | 0 | 6.1 | 5.7 | 6.1 | 5.7 | 6.3 | 4.9 | 5.2 | |
| REBA | 4.9 | 5.0 | 6.0 | 5.5 | 7.7 | 8.5 | 5.8 | 5.0 | 5.2 | 0 | 8.0 | 6.5 | 5.7 | 4.8 | 7.0 | 6.4 | 5.0 | 0 | 0 | 8.8 | 6.7 | 7.8 | 6.8 | 6.9 | 5.9 | 6.1 | |
| GP5 | Freq. (%) | 1.6 | 0.0 | 62.8 | 0.0 | 0.0 | 0.0 | 0.0 | 47.3 | 0.0 | 0.0 | 3.4 | 0.0 | 0.0 | 3.4 | 0.0 | 4.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 88.3 | 0.0 | 0.0 | 5.7 | |
| RULA | 4.5 | 0 | 5.0 | 0 | 0 | 0 | 0 | 7.0 | 0 | 0 | 6.0 | 0 | 0 | 4.7 | 0 | 6.4 | 0 | 0 | 0 | 0 | 0 | 6.1 | 0 | 0 | 4.4 | 5.9 | |
| REBA | 5.3 | 0 | 5.0 | 0 | 0 | 0 | 0 | 6.1 | 0 | 0 | 9.8 | 0 | 0 | 3.8 | 0 | 7.7 | 0 | 0 | 0 | 0 | 0 | 9.6 | 0 | 0 | 4.2 | 7.4 | |
| GP6 | Freq. (%) | 2.0 | 10.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 0.0 | 0.0 | 23.0 | 14.8 | 40.4 | 17.7 | 92.1 | 100.0 | 0.0 | 69.4 | 1.2 | 0.0 | 0.0 | 0.0 | 0.0 | |
| RULA | 4.2 | 4.6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6.2 | 0 | 0 | 4.6 | 4.4 | 4.1 | 6.4 | 5.8 | 5.6 | 0 | 6.5 | 4.0 | 0 | 0 | 0 | 0 | 5.6 | |
| REBA | 5.6 | 5.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7.7 | 0 | 0 | 5.6 | 5.4 | 5.0 | 8.4 | 7.4 | 6.7 | 0 | 9.0 | 4.0 | 0 | 0 | 0 | 0 | 7.1 | |
| GP7 | Freq. (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 25.5 | 0.0 | 0.0 | 0.0 | 10.2 | 10.8 | 1.4 | 0.0 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| RULA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.9 | 0 | 0 | 0 | 5.2 | 5.2 | 5.0 | 0 | 6.1 | 0 | 0 | 0 | 0 | 0 | 0 | 5.6 | |
| REBA | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6.0 | 0 | 0 | 0 | 6.0 | 7.2 | 5.0 | 0 | 7.9 | 0 | 0 | 0 | 0 | 0 | 0 | 7.2 | |
| Mean RULA score from all postures$ | 4.11A | 4.03A | 4.82B | 4.29A | 5.41B | 5.90C | 3.98A | 6.30C | 5.44B | 6.20C | 3.85B | 5.16B | 4.40A | 4.65A | 3.71A | 4.95B | 5.63B | 5.62B | 6.06C | 6.09C | 4.64B | 6.07C | 5.30B | 5.46B | 4.37A | ||
| Mean REBA score from all postures$ | 5.05C | 3.78A | 5.21C | 5.09C | 7.39D | 7.96E | 4.48B | 6.29E | 5.65D | 7.69E | 5.27C | 7.22D | 4.88B | 4.51B | 4.79B | 6.40D | 7.21E | 6.71D | 7.86E | 8.19E | 5.22C | 9.42E | 6.19D | 6.39D | 4.62B | ||
| Mean RULA Score from GP# | 4.64 | 4.58 | 5.54 | 5.13 | 4.96 | 4.59 | 4.52 | 5.29 | 4.79 | 5.60 | 5.01 | 4.65 | 4.91 | 4.99 | 5.08 | 5.20 | 5.55 | 5.60 | 5.63 | 5.36 | 4.95 | 5.78 | 4.90 | 4.70 | 4.89 | ||
| Mean REBA Score from GP# | 5.33 | 5.28 | 6.76 | 5.98 | 5.66 | 5.24 | 5.14 | 6.35 | 5.53 | 7.12 | 5.90 | 5.32 | 5.80 | 5.90 | 6.15 | 6.22 | 7.02 | 7.12 | 7.18 | 6.63 | 5.65 | 7.23 | 5.68 | 5.39 | 5.67 | ||
Note: The gray values represent the GP frequency that composed each massage. Mean RULA and REBA scores were presented form all postures (horizontally in white) and from GP relative scores (horizontally in blue) presented vertically on the right. A,B,C,D,E: values with the same exponent are not significantly different from each other but are different from other values (Kruskal-Wallis analysis, P < .05, independently for RULA and REBA).
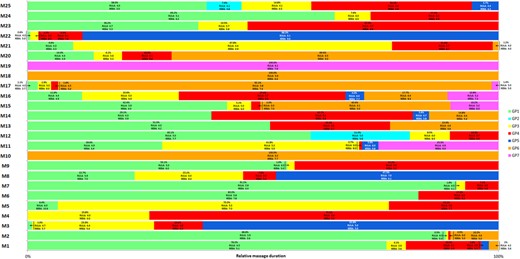
Relationship between GP frequency and RULA/REBA scores per massage.
From the set of postures, the lowest RULA score was found for M15 (3.71, a corresponding REBA score of 4.79). M15 with M1, M2, M4, M13, M14, M21 and M25 presented the significantly lowest RULA score (P < .05). The highest score was observed for M8 (6.30 with a corresponding REBA score of 6.29) and composed of M6, M10, M19, M20, and M22 the group with the highest score (P < .05). About REBA, the lowest score was 3.78 for REBA M2 (corresponding RULA score of 4.03, P < .05) and the highest was 9.42 for M22 (corresponding RULA score of 6.07), included with M6, M8, M10, M17, M19, and M20 in the group with the statistically highest scores (P < .05). From GP ergonomics scores, the overall RULA scores varied between 4.52 (M7) to 5.78 (M23) and REBA overall scores were between 5.14 (M7) to 7.23 (M22).
Figure 3 illustrates the temporal sequencing of the use of the different GPs for the five massages of each physiotherapist (PT1 to PT5). PT2 and PT3 preferentially used GP1 with frequencies of 50.4% and 44.3%, respectively, across their 5 massages. They complemented with the use of GP4 and GP5 with frequencies of between 15 and 20%. The other GPs were less used. PT1 also mainly used GP1 (34.5%) in conjunction with GP3 and GP4 (25.3% and 24.8%, respectively). PT5 used 4 GPs equally (GP1: 29.9%, GP3: 20.5%, GP4: 29.1% and GP5: 18.8%). Finally, PT4 uses GP5 more than half the time (55.9%), followed by GP7 (22.5%), which was not used at all by PT1, PT2, and PT5. The ergonomic assessment showed that PT1, PT2, PT3, and PT5 spend half their massage time with GPs that have the lowest RULA/REBA scores (RULA between 4 and 5, and REBA between 5 and 6, Table 2), that is, with low risk of MSDs. PT4 spent 90% of time in GPs with a higher RULA/REBA score (RULA>5 and REBA>7), that is, moderate risk of MSDs.
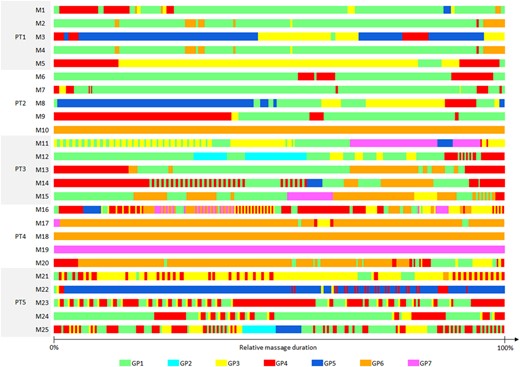
Time sequence of GP during the 25 massages observed. The representation is normalized from 0 to 100% of the massage duration. PT, physiotherapist.
DISCUSSION
The aim of this study was to quantify the postures and to assess the risk of MSDs in physiotherapists repeating a lymphatic drainage massage over a three-month period.
The hierarchical cluster analysis revealed seven GPs from all five massages performed by the five physiotherapists. Each GP was defined by a set of 13 joint mean angles with their respective standard deviation, a frequency of use and a RULA/REBA ergonomic score indicating the level of MSD risk. This result reinforces the concept of GPs introduced by Jacquier-Bret et al. and carried out on 7 physiotherapists.23 In this previous work, the assessment tool was the RULA, whereas in our study we have also used the REBA. The latter takes greater account of the lower limbs through the knee and provides information on activity in a different way. This last point is essential in our study since the aspects of static posture (>1 min) and repetition of small-range actions present in massages are taken into account more in the REBA analysis than in the RULA.
The GP notion enables complex and long-duration tasks to be described through a limited number of key postures. Each GP is defined on the basis of a cluster of postures considered close by a set of joint angles and average ergonomic scores to which a standard deviation was associated. The uncertainty associated with the definition of GPs is directly linked to the agglomeration coefficient value in the HCA. This coefficient has an impact on the number of clusters obtained by the HCA, as well as on the variability of each of them. Indeed, the lower the coefficient is, the higher the number of GPs and the lower their respective variability are. In this case, the GP are very close to each other, which is of little interest in the context of MSD prevention. Conversely, if the coefficient is too high, the number of GPs is too low (and the variability too high), failing to accurately describe the postural particularities of the activity. Some high-risk postures could be included in a cluster with acceptable ergonomic scores. For the purposes of this study, we made an intermediate choice (agglomeration coefficient equal to 1000): the number of GPs is high enough to describe the massage activity while being sufficiently distinct from each other (see Table 1) to perform a relevant ergonomic analysis.
The RULA ergonomic analysis showed that the MSD risks varied from low (scores between 4 and 5 for 3 GPs – 4.46 ± 0.84 to ±4.93 ± 0.93) to moderate (scores above 5 for 4 GPs – 5.20 ± 1.02 to 5.87 ± 0.98). These values are consistent with those presented in our previous work, which included 14 massages.23 Mean RULA scores ranged from 4.0 ± 1.1 to 5.8 ± 1.2, corresponding to the same level of MSD risk as found in the present work. REBA scores were on average 1 point higher than RULA scores (REBA score between 5.06 ± 1.75 and 7.39 ± 2.39). It is difficult to compare these scores directly since the risk assessment scales are different: a scale from 1 to 7 with 4 risk levels for RULA, and a scale from 1 to 12 with 5 risk levels for REBA (Table 2). For the latter, the level of risk associated with massage is moderate for the 7 GP (level 3 of MSD risk, score between 4 and 7). Whole-body management and activity score in REBA could explain the greater risks than those obtained with RULA. These risks can be increased or reduced depending on the posture since the GP were defined by average angles combined with a standard deviation. Indeed, different combinations of joint angles close to the upper or lower limits could significantly affect posture and thus modify the risk of MSDs. In any case, the MLD presents risks that need to be monitored.
The joint angle data presented in Table 2 show which joints were more exposed to MSD, independently of the ergonomic scores. These data are in line with the literature, in particular the works that report significant prevalence by body zone among physiotherapists.1,28–30 All GP presented important neck (>20°) and trunk (>20° for GP5, GP6, GP7, between 15 and 20° for the others) flexion, which is in agreement with previous studies on massage.17,23 These values imply a biomechanical/ergonomic risk, as has been reported in other long-duration static activities, for example, smartphone use.31–33 Numerous studies have reported that significant neck and trunk flexion could be the cause of neck and lower back pain responsible for the occurrence of MSDs. These data largely could explain the high prevalence reported for these two areas among physiotherapists.11,17 In addition, five of the 7 GP (GP1, GP2, GP5, GP6, and GP7) presented an inclination and/or rotation of the neck and/or trunk greater than 10°, which increases the risk of MSDs. These important aspects were rarely quantified in the literature. However, they are systematically taken into account by a “+1” rating during ergonomic assessment using tools such as RULA and REBA.19,20
The shoulder was very involved during massages. GP4 and GP5 showed significant flexion (>40°) with abduction over 20°. Similarly, GP3 had a high abduction higher than 50° combined with flexion over 25°. As for neck and trunk, wide joint angles increase muscle strain and contribute to the development of MSDs34 especially considering repeated movements during massage.5 These postures explain the high prevalence observed for the shoulder among physiotherapists.17,35 GP6 and GP7 exposed the shoulder to MSD since they have values of around 30° for these two joint angles. Only GP1 and 2 had acceptable values for the shoulder (<15°).
Even though they were seated, physiotherapists used many different postures for their lower limbs (legs crossed or spread, knee more or less flexed or leg aligned with the thigh) and changed regularly during the massage. This reflects the discomfort resulting from maintaining these postures for long durations. This aspect was particularly illustrated by the REBA scores, which classified all GP with a moderate MSD risk.
Our results extend the notion of GP introduced in a previous work.23 We introduced the temporality of a complex activity in longitudinal follow-up and defined the GPs more precisely, that is, by integrating trunk and neck rotations. These results support the hypothesis that massage is an activity that exposes physiotherapists to moderate MSD risks that need to be monitored. A particular attention should be paid to postures with large amplitudes and postures close to neutral joint should be preferred. Applied by each physiotherapist over the follow-up period, the GPs allow postural habits to emerge during massages. The analysis showed that GP1 was the most widely used in the sample (34.0%) and was preferred by PT1, PT2, and PT3 (34.5%, 50.4%, and 44.3%, respectively). At the same time, GP1 had the lowest ergonomic scores, that is, the lowest MSD risk. PT4 mainly used GP5 (55.9% of the massage time), which was the posture with the highest RULA/REBA scores and, therefore, the highest risk of MSDs. The GP could be used to propose individualized recommendations as part of MSD prevention. General recommendations could be addressed to prevent the apparition of MSDs in physiotherapists during massage:
Adjust seat and table height to reduce neck, trunk and shoulder flexion, and position elbows at 90°.
Orient the body in relation to the area to be massaged to avoid twisting and tilting.
Limitations
The main limitation concerns the subjects and the analysis period. The study involved five physiotherapists who each performed five massages over a three-month period. In order to generalize the “GP notion,” it is important to extend the analysis on a larger number of subjects and considering more massages per physiotherapist. Secondly, it is possible that the physiotherapists’ profiles (experience, training and awareness of work-related MSD problems) may influence the postures adopted and, therefore, the GP. It would be interesting to take them into account in future work.
Another limitation concerns the definition of the GP through the choice of the agglomeration coefficient to identify posture clusters in the hierarchical cluster analysis. It would be interesting to consider the effect of this choice in the determination of GPs and, therefore, of an activity through this method.
CONCLUSION
The concept of Generic Posture was used to study the MSD risks to which physiotherapists are exposed when performing five massages spread over a three-month period. Seven GPs were used to describe manual lymphatic massage. MSD risk was assessed as low to moderate. Different profiles of postural habits were observed among the physiotherapists, showing that not all were exposed to the same risk when performing massages. Detailed analysis of joint angles enabled the body areas most at risk to be identified, depending on the GPs used. The results led to general recommendations that could be personalized according to each practitioner’s profile. The inclusion of a larger number of physiotherapists over a longer period in future studies could allow to simplify the analysis of MSD risks through GPs in the context of massage.
AUTHOR CONTRIBUTIONS
Philippe Gorce and Julien Jacquier-Bret involved in conceptualization, methodology, software, validation, formal analysis, investigation, resources, data curation, writing the original draft, review and editing, and visualization. Philippe Gorce involved in supervision, project administration, and funding acquisition.
ACKNOWLEDGMENTS
We would like to thank Emilie Rouvière, head of the physiotherapy department, and all the physiotherapists who agreed to take part in the study.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
ETHICS STATEMENT
The protocol was approved by the local ethics committee (LBCE-2023-11).
CONSENT FOR PUBLICATION
They were informed of the entire protocol and gave their written consent before taking part in the experiment.



