-
PDF
- Split View
-
Views
-
Cite
Cite
Joshua S Yoon, Kimberly H Khoo, Arya A Akhavan, Tomer Lagziel, Michael Ha, Carrie A Cox, Renee Blanding, Emily H Werthman, Julie Caffrey, C Scott Hultman, Changes in Burn Surgery Operative Volume and Metrics due to COVID-19, Journal of Burn Care & Research, Volume 43, Issue 6, November/December 2022, Pages 1233–1240, https://doi.org/10.1093/jbcr/irac111
Close - Share Icon Share
Abstract
Due to COVID-19, hospitals underwent drastic changes to operating room policy to mitigate the spread of the disease. Given these unprecedented measures, we aimed to look at the changes in operative volume and metrics of the burn surgery service at our institution. A retrospective review was conducted for operative cases and metrics for the months of March to May for 2019, 2020, and 2021, which correspond with pre-COVID, early COVID (period without elective cases), and late COVID (period with resumed elective cases). Inclusion criteria were cases related to burns. Case types and operative metrics were compared amongst the three time-periods. Compared to the hospital, the burn service had a smaller decrease in volume during early COVID (28.7% vs 50.1%) and exceeded prepandemic volumes during late COVID (+21.8% vs ‐4.6%). There was a significant increase in excision and grafting cases in early and late COVID periods (P < .0001 and P < .002). There was a significant decrease in laser scar procedures that persisted even during late COVID (P < .0001). The projected and actual lengths of cases significantly increased and persisted into late COVID (P < .01). COVID-19 related operating room closures led to an expected decrease in the number of operative cases. However, there was no significant decline in the number of burn specific cases. The elective cases were largely replaced with excision and grafting cases and this shift has persisted even after elective cases have resumed. This change is also reflected in increased operative times.
BACKGROUND
The ongoing pandemic by the COVID-19 virus has had far reaching effects on all aspects of society from sudden lockdowns and prolonged school closures to changes in the way residency and fellowship interviews are conducted.1–3 At the onset of this generational disaster, hospitals were driven to immediately cancel, and discontinue all elective cases because of the overwhelming number of COVID-19 admissions and to minimize any unnecessary exposure to healthcare personnel. Some operating rooms (ORs) were even repurposed into overflow intensive care units (ICUs) to accommodate the rapid surge of critically ill patients.4 Such cancelations were aligned with formal recommendations to proactively minimize all elective operations from national professional organizations and societies such as the Center for Disease Control, the American College of Surgeons, and the American Society of Plastic Surgery.5–7
As expected, the number of elective cases precipitously decreased with the enactment of elective case cancelations.8 Preliminary reports among aesthetic plastic surgeons estimate a 20% decrease in overall revenue due to pandemic related closures.7 Plastic and reconstructive emergency surgeries also saw reductions in case volume ranging from 31.8% to 55%.8,9 However, operative volume of emergency hand and upper extremity surgeries were found to increase by 40% in the same time-period.10 Although the pandemic resulted in the forced cancelation of only elective cases, volumes of nonelective cases were affected as well. To date, there has been no published literature on how the COVID-19 pandemic has affected operative volume and case types in burn surgery. In this study, we present data from our university affiliated American Burn Association verified burn center to characterize how operative volume and case distributions have evolved due to the pandemic.
METHODS
Study Design
An IRB-approved single-institution retrospective review was conducted by querying our institutional OR database. For the purposes of our study, we created three groups based on time-periods. The time-period groupings were March 1st to May 31st for 2019, 2020, and 2021, which correspond with pre-COVID, early COVID (period without elective cases), and late COVID (period with resumed elective cases), respectively. These months were specifically chosen for two reasons. One is to account for seasonal variability. The second is to capture the effects of the lockdown restrictions and OR cancelations at their most severe, which was within the first few months after the onset of COVID. From the database, we obtained case lists for each of these time-periods with associated OR metrics for each case. Our institutional burn registry was also queried for the predefined time-periods to characterize the overall volume of burn patients being cared.
Variables, Outcomes, and Statistics
From the burn registry, we obtained and compared the number of burn patients evaluated and their respective hospital/discharge dispositions, the type of burn injuries, and average TBSAs for each of the respective time-periods. From the OR registry, overall operative volume for each specialty was compared. The specialties were burn and reconstructive surgery, gastroenterology, general surgery, gynecology, gynecology urology, neurosurgery, obstetrics, ophthalmology, orthopedic surgery, otolaryngology, plastics, and reconstructive surgery, pulmonology, urology, and vascular surgery. The case lists were then filtered to identify all procedures performed by the burn and reconstructive surgery service. Each of these cases was then individually chart reviewed so that only cases related to burns were included in the final analysis. The burn cases were then divided into the following groups: excision only, grafting only, excision, and grafting, laser scar procedures, secondary reconstruction without grafting or flaps, secondary reconstruction with grafting, and secondary reconstruction with flaps. Operative metrics that were compared were time during the week the operation occurred (weekday vs weekend), actual case length, projected case length, OR cleanup time, OR set up time, and case disposition (eg, outpatient surgery, extended surgical recovery, surgery requiring admission, inpatient surgery).
Frequencies and percentages for categorical variables and means, standard deviations, medians, interquartile ranges, minima, and maxima for continuous variables were calculated and compared between groups using the Chi-square test for categorical variables and ANOVA test for continuous variables as appropriate. Given the multiple comparisons between case groupings, a Bonferroni correction was applied, and all statistical tests were considered to be statistically significant when a P-value is less than .0024. All other results were statistically significant when a P-value is less than .05. All analyses were performed using RStudio Version 1.3.1093 (Boston, MA).
RESULTS
There were 184, 152, and 166 burn patients evaluated during the predefined time-periods (pre-COVID, early COVID, late COVID), respectively. During the pre-COVID period, there were a significantly higher number of patients that were discharged from the emergency department compared to the early COVID and late COVID periods (P = .04). The most common burn types were flame burns followed by scald burns and there were no significant changes in their incidences between time-periods. The average TBSA was highest in the pre-COVID time-period (9.6%), followed by the late COVID period (8.0%), and then the early COVID period (7.3%) (Table 1).
| . | Pre-COVID . | Early COVID . | Late COVID . | P . |
|---|---|---|---|---|
| Total Number of Burn Patients Evaluated* | 184 | 152 | 166 | .037* ,† |
| Discharged from ED | 125 | 83 | 98 | |
| Admitted | 59 | 69 | 68 | |
| Types of Burn Injury (%) | ||||
| Flame | 49.1 | 46.0 | 46.2 | 1‡ |
| Scald | 33.3 | 34.9 | 35.8 | |
| Other | 17.6 | 19.1 | 18.0 | |
| Average Burn TBSA | 9.6 | 7.3 | 8.0 | .7‡ |
| . | Pre-COVID . | Early COVID . | Late COVID . | P . |
|---|---|---|---|---|
| Total Number of Burn Patients Evaluated* | 184 | 152 | 166 | .037* ,† |
| Discharged from ED | 125 | 83 | 98 | |
| Admitted | 59 | 69 | 68 | |
| Types of Burn Injury (%) | ||||
| Flame | 49.1 | 46.0 | 46.2 | 1‡ |
| Scald | 33.3 | 34.9 | 35.8 | |
| Other | 17.6 | 19.1 | 18.0 | |
| Average Burn TBSA | 9.6 | 7.3 | 8.0 | .7‡ |
ED, emergency department; TBSA, total body surface area.
*P < .05.
†Chi-square test.
‡ANOVA.
| . | Pre-COVID . | Early COVID . | Late COVID . | P . |
|---|---|---|---|---|
| Total Number of Burn Patients Evaluated* | 184 | 152 | 166 | .037* ,† |
| Discharged from ED | 125 | 83 | 98 | |
| Admitted | 59 | 69 | 68 | |
| Types of Burn Injury (%) | ||||
| Flame | 49.1 | 46.0 | 46.2 | 1‡ |
| Scald | 33.3 | 34.9 | 35.8 | |
| Other | 17.6 | 19.1 | 18.0 | |
| Average Burn TBSA | 9.6 | 7.3 | 8.0 | .7‡ |
| . | Pre-COVID . | Early COVID . | Late COVID . | P . |
|---|---|---|---|---|
| Total Number of Burn Patients Evaluated* | 184 | 152 | 166 | .037* ,† |
| Discharged from ED | 125 | 83 | 98 | |
| Admitted | 59 | 69 | 68 | |
| Types of Burn Injury (%) | ||||
| Flame | 49.1 | 46.0 | 46.2 | 1‡ |
| Scald | 33.3 | 34.9 | 35.8 | |
| Other | 17.6 | 19.1 | 18.0 | |
| Average Burn TBSA | 9.6 | 7.3 | 8.0 | .7‡ |
ED, emergency department; TBSA, total body surface area.
*P < .05.
†Chi-square test.
‡ANOVA.
The total number of cases performed by the entire hospital during 2019, 2020, and 2021 was 2375, 1184, and 2265 respectively; overall there was a 50.1% reduction in total volume due to COVID, a 91.3% rebound in total volume when comparing the early and late COVID periods, and a net loss of 4.6% when comparing the pre-CVOID and late COVID time-periods. When looking at the specialty services with at least 100 cases: 1) the most heavily affected by the COVID-related closures were plastic and reconstructive surgery (‐67.5%) followed by otolaryngology (‐64.9%) and gynecology (‐60.1%), 2) those with the greatest rebound in operative volume when comparing the early and late COVID periods were plastic and reconstructive surgery (208.8%) followed by gynecology (138.7%) and urology (96.2%), and 3) those that had the greatest net loss from the pre-COVID and late COVID time-periods were otolaryngology (‐29.8%), urology (‐6.5%), and gynecology (‐4.8%). During those times, the burn, and reconstructive surgery service performed 174, 124, and 212 total cases respectively. Compared to the hospital, the burn service had a smaller decrease in volume during early COVID (28.7% vs 50.1%) and exceeded prepandemic volumes during late COVID (+21.8% vs ‐4.6%) (Table 2).
| . | Pre-COVID . | Early COVID . | Late COVID . | % Change Pre vs Early COVID . | % Change Late vs Early COVID . | % Change Late vs Pre-COVID . |
|---|---|---|---|---|---|---|
| Total Number of Cases | 2375 | 1184 | 2265 | ‐50.1 | 91.3 | ‐4.6 |
| Burn and Reconstructive Surgery | 174 | 124 | 212 | ‐28.7 | 71.0 | 21.8 |
| Gastrointestinal | 2 | 2 | 3 | 0 | 50 | 50 |
| General Surgery | 492 | 258 | 473 | ‐47.6 | 83.3 | ‐3.9 |
| Gynecology | 188 | 75 | 179 | ‐60.1 | 138.7 | ‐4.8 |
| Gynecology/Urology | 1 | 1 | 1 | 0 | 0 | 0 |
| Neurosurgery | 136 | 75 | 134 | ‐44.9 | 78.7 | ‐1.5 |
| Obstetrics | 14 | 0 | 2 | ‐100 | n/a | ‐85.7 |
| Ophthalmology | 1 | 0 | 0 | ‐100 | n/a | ‐100 |
| Orthopedics | 482 | 228 | 437 | ‐52.7 | 91.7 | ‐9.3 |
| Otolaryngology | 131 | 46 | 92 | ‐64.9 | 100 | ‐29.8 |
| Plastics and Reconstructive Surgery | 209 | 68 | 210 | ‐67.5 | 208.8 | 0.5 |
| Pulmonary | 7 | 6 | 3 | ‐14.3 | ‐50 | ‐57.1 |
| Urology | 279 | 133 | 261 | ‐52.3 | 96.2 | ‐6.5 |
| Vascular | 259 | 168 | 258 | ‐35.1 | 53.6 | ‐0.4 |
| . | Pre-COVID . | Early COVID . | Late COVID . | % Change Pre vs Early COVID . | % Change Late vs Early COVID . | % Change Late vs Pre-COVID . |
|---|---|---|---|---|---|---|
| Total Number of Cases | 2375 | 1184 | 2265 | ‐50.1 | 91.3 | ‐4.6 |
| Burn and Reconstructive Surgery | 174 | 124 | 212 | ‐28.7 | 71.0 | 21.8 |
| Gastrointestinal | 2 | 2 | 3 | 0 | 50 | 50 |
| General Surgery | 492 | 258 | 473 | ‐47.6 | 83.3 | ‐3.9 |
| Gynecology | 188 | 75 | 179 | ‐60.1 | 138.7 | ‐4.8 |
| Gynecology/Urology | 1 | 1 | 1 | 0 | 0 | 0 |
| Neurosurgery | 136 | 75 | 134 | ‐44.9 | 78.7 | ‐1.5 |
| Obstetrics | 14 | 0 | 2 | ‐100 | n/a | ‐85.7 |
| Ophthalmology | 1 | 0 | 0 | ‐100 | n/a | ‐100 |
| Orthopedics | 482 | 228 | 437 | ‐52.7 | 91.7 | ‐9.3 |
| Otolaryngology | 131 | 46 | 92 | ‐64.9 | 100 | ‐29.8 |
| Plastics and Reconstructive Surgery | 209 | 68 | 210 | ‐67.5 | 208.8 | 0.5 |
| Pulmonary | 7 | 6 | 3 | ‐14.3 | ‐50 | ‐57.1 |
| Urology | 279 | 133 | 261 | ‐52.3 | 96.2 | ‐6.5 |
| Vascular | 259 | 168 | 258 | ‐35.1 | 53.6 | ‐0.4 |
n/a, Not applicable.
| . | Pre-COVID . | Early COVID . | Late COVID . | % Change Pre vs Early COVID . | % Change Late vs Early COVID . | % Change Late vs Pre-COVID . |
|---|---|---|---|---|---|---|
| Total Number of Cases | 2375 | 1184 | 2265 | ‐50.1 | 91.3 | ‐4.6 |
| Burn and Reconstructive Surgery | 174 | 124 | 212 | ‐28.7 | 71.0 | 21.8 |
| Gastrointestinal | 2 | 2 | 3 | 0 | 50 | 50 |
| General Surgery | 492 | 258 | 473 | ‐47.6 | 83.3 | ‐3.9 |
| Gynecology | 188 | 75 | 179 | ‐60.1 | 138.7 | ‐4.8 |
| Gynecology/Urology | 1 | 1 | 1 | 0 | 0 | 0 |
| Neurosurgery | 136 | 75 | 134 | ‐44.9 | 78.7 | ‐1.5 |
| Obstetrics | 14 | 0 | 2 | ‐100 | n/a | ‐85.7 |
| Ophthalmology | 1 | 0 | 0 | ‐100 | n/a | ‐100 |
| Orthopedics | 482 | 228 | 437 | ‐52.7 | 91.7 | ‐9.3 |
| Otolaryngology | 131 | 46 | 92 | ‐64.9 | 100 | ‐29.8 |
| Plastics and Reconstructive Surgery | 209 | 68 | 210 | ‐67.5 | 208.8 | 0.5 |
| Pulmonary | 7 | 6 | 3 | ‐14.3 | ‐50 | ‐57.1 |
| Urology | 279 | 133 | 261 | ‐52.3 | 96.2 | ‐6.5 |
| Vascular | 259 | 168 | 258 | ‐35.1 | 53.6 | ‐0.4 |
| . | Pre-COVID . | Early COVID . | Late COVID . | % Change Pre vs Early COVID . | % Change Late vs Early COVID . | % Change Late vs Pre-COVID . |
|---|---|---|---|---|---|---|
| Total Number of Cases | 2375 | 1184 | 2265 | ‐50.1 | 91.3 | ‐4.6 |
| Burn and Reconstructive Surgery | 174 | 124 | 212 | ‐28.7 | 71.0 | 21.8 |
| Gastrointestinal | 2 | 2 | 3 | 0 | 50 | 50 |
| General Surgery | 492 | 258 | 473 | ‐47.6 | 83.3 | ‐3.9 |
| Gynecology | 188 | 75 | 179 | ‐60.1 | 138.7 | ‐4.8 |
| Gynecology/Urology | 1 | 1 | 1 | 0 | 0 | 0 |
| Neurosurgery | 136 | 75 | 134 | ‐44.9 | 78.7 | ‐1.5 |
| Obstetrics | 14 | 0 | 2 | ‐100 | n/a | ‐85.7 |
| Ophthalmology | 1 | 0 | 0 | ‐100 | n/a | ‐100 |
| Orthopedics | 482 | 228 | 437 | ‐52.7 | 91.7 | ‐9.3 |
| Otolaryngology | 131 | 46 | 92 | ‐64.9 | 100 | ‐29.8 |
| Plastics and Reconstructive Surgery | 209 | 68 | 210 | ‐67.5 | 208.8 | 0.5 |
| Pulmonary | 7 | 6 | 3 | ‐14.3 | ‐50 | ‐57.1 |
| Urology | 279 | 133 | 261 | ‐52.3 | 96.2 | ‐6.5 |
| Vascular | 259 | 168 | 258 | ‐35.1 | 53.6 | ‐0.4 |
n/a, Not applicable.
Of the 174, 124, and 212 total cases performed during each time-period by the burn and reconstructive surgery service, there were 138 (79.3%), 103 (83.1%), and 114 (53.8%) burn-related cases, respectively. The most common procedures in the pre-COVID time-period were burn scar laser procedures (69) followed by combined excision and grafting cases (41). Combined excision and grafting cases became the most dominant procedures in the early and late COVID periods with 84 and 74 cases respectively. There were statistically significant increases in combined excision and grafting cases when comparing the pre-COVID to early COVID (P = .0001) and pre-COVID to late COVID (P = .002) time-periods, which demonstrate a significant and sustained increased in combined excision and grafting cases after the onset of COVID. Alternatively, the burn scar laser procedures were not performed at all during the early COVID period and were performed significantly less (14) during the late COVID period. During the early COVID period, these cases were being transitioned to the ambulatory surgery center. The decline in burn scar laser cases was statistically significant when comparing the pre-COVID to early COVID (P < .00001) and pre-COVID to late COVID (P < .00001) time-periods. There was also a statistically significant rebound of cases from the early COVID to late COVID time-periods (P = .0002). Overall, primary excision and/or grafting procedures became more common after the onset of COVID, whereas secondary/revisional procedures became less common (Table 3).
| . | Pre-COVID . | % Change Pre vs Early COVID (P-value) . | Early COVID . | % Change Early vs Late COVID (P-value) . | Late COVID . | % Change Pre vs Late COVID (P-value) . |
|---|---|---|---|---|---|---|
| Excision | 9 | 4.2% (.7) | 11 | 1.6% (.5) | 14 | 5.8% (.3) |
| Grafting | 0 | 4.9% (.025) | 5 | ‐4.9% (.03) | 0 | 0% (N/A) |
| Excision and Grafting | 41 | 51.8% (.0001)* | 84 | ‐16.6% (.4) | 74 | 35.2% (.002)* |
| Burn Scar Laser | 69 | ‐50% (<.0001)* | 0 | 12.3% (.0002)* | 14 | ‐37.7% (<.0001)* |
| Secondary Surgery Without Grafting or Flaps | 4 | ‐2.9% (.05) | 0 | 2.6% (.08) | 3 | ‐0.3% (.7) |
| Secondary Surgery with Grafting | 6 | ‐3.4% (.06) | 1 | 3.4% (.1) | 5 | .04% (.8) |
| Secondary Surgery with Flaps | 9 | ‐4.6% (.03) | 2 | 1.6% (.4) | 4 | ‐3.0% (.2) |
| . | Pre-COVID . | % Change Pre vs Early COVID (P-value) . | Early COVID . | % Change Early vs Late COVID (P-value) . | Late COVID . | % Change Pre vs Late COVID (P-value) . |
|---|---|---|---|---|---|---|
| Excision | 9 | 4.2% (.7) | 11 | 1.6% (.5) | 14 | 5.8% (.3) |
| Grafting | 0 | 4.9% (.025) | 5 | ‐4.9% (.03) | 0 | 0% (N/A) |
| Excision and Grafting | 41 | 51.8% (.0001)* | 84 | ‐16.6% (.4) | 74 | 35.2% (.002)* |
| Burn Scar Laser | 69 | ‐50% (<.0001)* | 0 | 12.3% (.0002)* | 14 | ‐37.7% (<.0001)* |
| Secondary Surgery Without Grafting or Flaps | 4 | ‐2.9% (.05) | 0 | 2.6% (.08) | 3 | ‐0.3% (.7) |
| Secondary Surgery with Grafting | 6 | ‐3.4% (.06) | 1 | 3.4% (.1) | 5 | .04% (.8) |
| Secondary Surgery with Flaps | 9 | ‐4.6% (.03) | 2 | 1.6% (.4) | 4 | ‐3.0% (.2) |
n/a, Not applicable.
P values < .0024 considered to be significant due to Bonferroni correction.
*P < .0024.
| . | Pre-COVID . | % Change Pre vs Early COVID (P-value) . | Early COVID . | % Change Early vs Late COVID (P-value) . | Late COVID . | % Change Pre vs Late COVID (P-value) . |
|---|---|---|---|---|---|---|
| Excision | 9 | 4.2% (.7) | 11 | 1.6% (.5) | 14 | 5.8% (.3) |
| Grafting | 0 | 4.9% (.025) | 5 | ‐4.9% (.03) | 0 | 0% (N/A) |
| Excision and Grafting | 41 | 51.8% (.0001)* | 84 | ‐16.6% (.4) | 74 | 35.2% (.002)* |
| Burn Scar Laser | 69 | ‐50% (<.0001)* | 0 | 12.3% (.0002)* | 14 | ‐37.7% (<.0001)* |
| Secondary Surgery Without Grafting or Flaps | 4 | ‐2.9% (.05) | 0 | 2.6% (.08) | 3 | ‐0.3% (.7) |
| Secondary Surgery with Grafting | 6 | ‐3.4% (.06) | 1 | 3.4% (.1) | 5 | .04% (.8) |
| Secondary Surgery with Flaps | 9 | ‐4.6% (.03) | 2 | 1.6% (.4) | 4 | ‐3.0% (.2) |
| . | Pre-COVID . | % Change Pre vs Early COVID (P-value) . | Early COVID . | % Change Early vs Late COVID (P-value) . | Late COVID . | % Change Pre vs Late COVID (P-value) . |
|---|---|---|---|---|---|---|
| Excision | 9 | 4.2% (.7) | 11 | 1.6% (.5) | 14 | 5.8% (.3) |
| Grafting | 0 | 4.9% (.025) | 5 | ‐4.9% (.03) | 0 | 0% (N/A) |
| Excision and Grafting | 41 | 51.8% (.0001)* | 84 | ‐16.6% (.4) | 74 | 35.2% (.002)* |
| Burn Scar Laser | 69 | ‐50% (<.0001)* | 0 | 12.3% (.0002)* | 14 | ‐37.7% (<.0001)* |
| Secondary Surgery Without Grafting or Flaps | 4 | ‐2.9% (.05) | 0 | 2.6% (.08) | 3 | ‐0.3% (.7) |
| Secondary Surgery with Grafting | 6 | ‐3.4% (.06) | 1 | 3.4% (.1) | 5 | .04% (.8) |
| Secondary Surgery with Flaps | 9 | ‐4.6% (.03) | 2 | 1.6% (.4) | 4 | ‐3.0% (.2) |
n/a, Not applicable.
P values < .0024 considered to be significant due to Bonferroni correction.
*P < .0024.
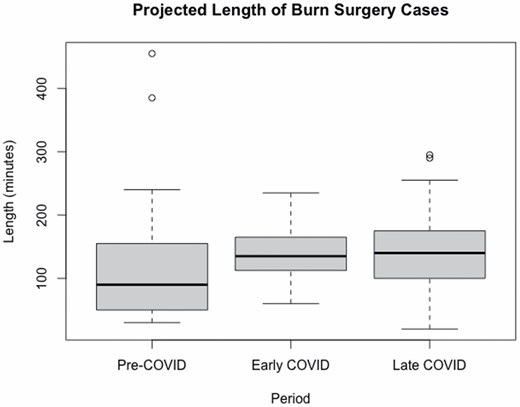
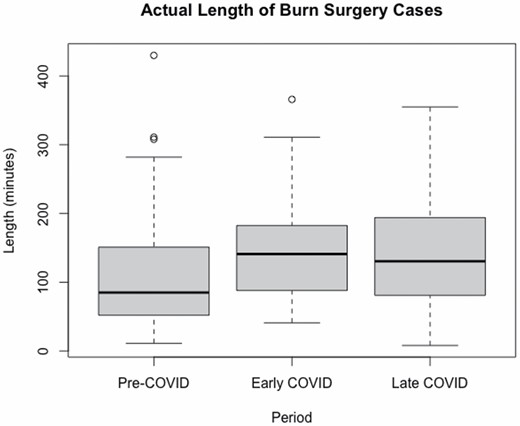
The average projected lengths of cases and actual lengths of cases were similar across all time-periods and the largest discrepancy was found in the pre-COVID period (110.3, 113.3 min). With the onset of COVID, the average projected and actual lengths of cases became significantly longer (137.8, 135.5 min; P = .0004 and .001), which persisted into the late COVID period (136.8, 136.1; P = .002 and .01) (Figures 1 and 2). In regard to case disposition, there was a steady increase in the number of inpatient procedures performed after the onset of COVID (71, 109, 157) whereas there was a steep decline in the number outpatient procedures performed after the onset of COVID with a minor rebound to pre-COVID levels (88, 8, 34). Most procedures were performed during the weekdays and the number of procedures performed during the weekends remained consistent during all time-periods (Table 4).
| . | Pre-COVID . | Early COVID . | Late COVID . |
|---|---|---|---|
| Projected Length Total (min) | 110.3 | 137.8 | 136.8 |
| Actual Length Total (min) | 113.3 | 135.5 | 136.1 |
| Cleanup Time (min) | 29.3 | 32.9 | 33.1 |
| Extended Surgical Recovery | 11 | 4 | 11 |
| Outpatient Surgery | 88 | 8 | 34 |
| Inpatient | 71 | 109 | 157 |
| Admit | 4 | 3 | 10 |
| Number of Cases on Weekend | 2 | 5 | 4 |
| Number of Cases on Weekday | 172 | 169 | 208 |
| . | Pre-COVID . | Early COVID . | Late COVID . |
|---|---|---|---|
| Projected Length Total (min) | 110.3 | 137.8 | 136.8 |
| Actual Length Total (min) | 113.3 | 135.5 | 136.1 |
| Cleanup Time (min) | 29.3 | 32.9 | 33.1 |
| Extended Surgical Recovery | 11 | 4 | 11 |
| Outpatient Surgery | 88 | 8 | 34 |
| Inpatient | 71 | 109 | 157 |
| Admit | 4 | 3 | 10 |
| Number of Cases on Weekend | 2 | 5 | 4 |
| Number of Cases on Weekday | 172 | 169 | 208 |
Statistically significant longer average projected and actual lengths of cases with the onset of COVID (137.8, 135.5 min; P = .0004 and .001) persisting into the late COVID period (136.8, 136.1; P = .002 and .01).
| . | Pre-COVID . | Early COVID . | Late COVID . |
|---|---|---|---|
| Projected Length Total (min) | 110.3 | 137.8 | 136.8 |
| Actual Length Total (min) | 113.3 | 135.5 | 136.1 |
| Cleanup Time (min) | 29.3 | 32.9 | 33.1 |
| Extended Surgical Recovery | 11 | 4 | 11 |
| Outpatient Surgery | 88 | 8 | 34 |
| Inpatient | 71 | 109 | 157 |
| Admit | 4 | 3 | 10 |
| Number of Cases on Weekend | 2 | 5 | 4 |
| Number of Cases on Weekday | 172 | 169 | 208 |
| . | Pre-COVID . | Early COVID . | Late COVID . |
|---|---|---|---|
| Projected Length Total (min) | 110.3 | 137.8 | 136.8 |
| Actual Length Total (min) | 113.3 | 135.5 | 136.1 |
| Cleanup Time (min) | 29.3 | 32.9 | 33.1 |
| Extended Surgical Recovery | 11 | 4 | 11 |
| Outpatient Surgery | 88 | 8 | 34 |
| Inpatient | 71 | 109 | 157 |
| Admit | 4 | 3 | 10 |
| Number of Cases on Weekend | 2 | 5 | 4 |
| Number of Cases on Weekday | 172 | 169 | 208 |
Statistically significant longer average projected and actual lengths of cases with the onset of COVID (137.8, 135.5 min; P = .0004 and .001) persisting into the late COVID period (136.8, 136.1; P = .002 and .01).
DISCUSSION
The COVID-19 pandemic forced healthcare systems and hospitals to reallocate resources in order to meet the rising case numbers of COVID-positive patients, and in doing so, drastically changed the way ORs were used and managed. The ensuing elective procedure moratorium resulted in a significant decline in total hospital operative volume, and it affected all specialties that performed any significant number of procedures during the pre-COVID era. We sought to quantify the changes in both operative volume and OR metrics that occurred due to these forced procedure cancelations.
Our data showed that some specialties, such as the plastic and reconstructive surgery service which has a higher proportion of elective cases, were affected more severely than others, and this significant decline in operative volume is consistent with recently published literature.11,12 However, there also appeared to be a concomitant decline in the number of plastic surgery patients presenting for and undergoing emergency cases as well, which may be secondary to a combination of lockdown mandates and concerns regarding possible increased risk of COVID-19 exposure/infection in the hospitals/emergency departments (EDs).9 Such a decline has also been more broadly observed as ED volumes of non-COVID-19 cases have decreased by 30.9% during the pandemic.13 Similar to previously reported literature, there was also a decrease in the number of burn patients evaluated at our institution after the onset of COVID. However, even with the decline in the overall number of evaluated burn patients, there was an increase in both the absolute number and proportion of burn patients admitted to the hospital.
A primary concern for patients during the COVID-19 pandemic was the fear that presenting or being admitted to the hospital would heighten the risk of contracting COVID-19, which in turn has been associated with significant delays in medical care across all specialties and all parts of the world.14,15 This applies to both patient presentation for emergencies (time of onset to time of arrival) and to delivery of care for urgent nonemergencies (time from diagnosis to delivery of definitive care). The delays in presentation and delivery of care have had a negative impact on patient outcomes; a study examining pediatric appendicitis showed a significant delay to presentation to the ED, which was associated with higher complication rates and worse patient outcomes.16 Urgent nonemergent care also showed significant delays, particularly in cancer; delays in definitive surgery led to significantly worse outcomes for renal cancer, while modeling studies suggest that delaying cancer surgery to spare COVID-19 exposure causes a significant decline in life-years gained.17,18 Contextualizing this in the setting of delays to presentation and delays in surgical care for burn patients would require additional research into the risk of COVID-19 exposure and infection for hospitalized burn patients, as well as outcomes changes in the setting of those delays. Specifically with regards to burn patients, we surmise that the fear of being exposed to COVID-19 at the hospital played a significant role in delays to presentation. Given the nature of burns, the patients with smaller self-limiting burns who may have otherwise needlessly presented to the hospital for evaluation will be able to successfully manage their injuries at home conservatively. This may be reflected in the smaller overall numbers of burn patients being evaluated at our institution. Conversely, those with larger burns in whom treatment in the ED could have prevented admission will present later with potential complications and as a result may need admission. This may be reflected in the higher absolute number and proportion of burn patients requiring admission. The possible delays in presentation and their associated consequences at our institution would be interesting to explore, however we are unable to do so given the limitations of our database.
Another factor that may be influencing likelihood of presenting to an ED is the impact the pandemic has had on the epidemiology and mechanism of injuries of trauma. Various studies have shown that the initial COVID-19 shutdowns or lockdowns have changed the injuries that people experience. Sephton and colleagues in their study evaluating changes in mechanism and diagnoses of orthopedic injuries, found that during the lockdowns, there was a significant decrease in the proportion of sports-related and traffic injuries, and that the total number of operations performed during the lockdown period fell 38.8% as compared to the prelockdown period. These differences are expected considering that individuals were required to stay at home except for limited exercise or essential shopping, decreasing rates of people who were driving or playing sports in large groups.19 Another article by Rapoport and colleagues20 demonstrated a similar decrease in motor vehicle injuries and fatalities in older adults, likely due to the same etiology of lockdowns preventing individuals from leaving their homes. A study examining trends in trauma admissions during COVID-19 lockdowns in Los Angeles County showed that while there were fewer blunt injuries in 2020 versus 2019 (prepandemic), there was a significantly higher incidence of penetrating trauma as compared to pre-COVID lockdown periods. This change in incidence of penetrating trauma may allude to an increase in violent crime during lockdown periods that echoes what other studies have assumed to be due to heightened levels of stress as well as a surge in the demand for guns.21–24
This emerging body of evidence shows that the pandemic has altered the incidence of certain injury etiologies, potentially causing certain subspecialty surgery services to operate less. However, among all specialties, the burn, and reconstructive surgery service appeared to not only be the least affected by the COVID-19 pandemic related OR cancelations, but also the most resilient, and adaptive. The burn and reconstructive surgery service had the smallest decline in operative volume with the elective case cancelations and was the only service that exceeded their prepandemic operative volume after the operative suspensions were lifted. Importantly, even though total case volumes are up for the burn and reconstructive surgery service, the overall number of burn-related procedures has remained stable, which indicates that there is a consistent population of burn patients that will require operative intervention. These findings parallel those of other articles studying burn injuries during the pandemic-lockdown period, which suggests potentially different mechanisms of burn injuries due to the pandemic. A study comparing characteristics of burn patients in 14 burn centers in the Tokyo Burn Unit Association registry before and during COVID-19 lockdowns showed that there was more scald or contact burns in the upper extremity and less intentional or assault injuries in presenting patients.25 The authors also found an increased incidence of inhalation injuries and flame burns as compared to prelockdown periods. In our own review, no significant differences were identified between the types of burn injuries and there was a small decline in TBSA that persisted even into the late COVID period. A retrospective comparison of the lockdown versus prelockdown period in the United Kingdom found that overall admission to the ED decreased in the lockdown period but that incidence of burn injuries in the ED was greater in proportion than in prelockdown periods—in the prelockdown period, burns accounted for 1.5% of ED admissions in contrast to 2.8% during the lockdowns.26 Mittal and colleagues14 found that emergency burn admissions have also declined, however the decline was relatively small at only 5.8%. They also found that the proportion of patients requiring acute operative intervention for their burns remained the same.14 Similarly, we observed not only a stable number of emergent or urgent burn-related procedures, but a statistically significant increase in the total number of emergent or urgent procedures.
Although there is literature to support that the incidence of burn injuries were relatively stable, there is also literature that supports that COVID decreased the incidence of burns presenting to the hospital.27,28 Currently there is not enough literature to say with certainty how the incidence of burns presenting to the hospital were affected in the United States, however we observed at our institution that the incidence of burn injuries were seemingly uninfluenced by the pandemic. Furthermore, it may be more granular to quantify such changes based on region and accounting for a variety of social factors in contrast to the country as a whole. Several studies have examined the impacts of regional factors and social determinants of health during the COVID pandemic.29–31 These studies have found that being part of underrepresented groups and systemic social inequality result in higher COVID-related complications and worse access to care. Similarly, we would believe that such factors would also affect the incidence, etiology, and presentation of patients with burn injuries, and merits further evaluation in future studies.
Due to the nature of the study, which is a database study as opposed to a retrospective chart review, we are unable to provide granular insight as to the reasons the rate of burn admissions remained stable. We hypothesize that patients who experience burn injuries may have had fewer restrictions or hesitations about going to the ED during lockdowns. This may be due logistical factors such as more flexibility in their schedule working from home, having a greater number of caretakers for children in the home during the lockdown, or could be due to the nature of injury and being unable to manage it at home. However, an alternative reason for the seemingly stable number of burn patients being admitted could be related to delayed presentation. Burn patients can be generally divided into three groups. The first group is patients with small burn injuries that present to the ED, however, would have been able to manage their injuries conservatively at home without any intervention or evaluation. The second group is burn patients with severe injuries requiring admission. The third group are patients that require evaluation and treatment in the ED without which they may subsequently develop complications and therefore require admission. Delay in presentation may decrease the overall number of burn patients presenting to the ED primarily from seeing less patients from group one, and conversely cause either stable or increase in burn admissions due to patients in group three not being treated in a timely manner. Further studies should investigate the reason for why the number of burn injuries and procedures remained consistent throughout this unique timeframe. Additionally, given this steady trend, hospitals, and administrators should recognize that even with widespread cancelations and OR closures, an appropriate number of ORs should be staffed to accommodate emergent and urgent burn-related procedures.
Elective procedures were necessarily delayed at the peak of the pandemic. While there is no published literature on the impact of delays or cancelation of elective burn procedures, these delays/cancelations may cause patients distress or a decreased quality of life. Different institutions may have different approaches to elective cases, including blanket bans during peak periods of COVID infection. To help mitigate this impact on care delivery, some surgical journals and surgical societies have provided guidelines on how to safely and effectively resume elective cases.32 Systematic approaches to resuming elective cases allow patients to undergo surgery without any increase in COVID infection rates, which has been shown in multiple studies across multiple disciplines and countries.33–35 When applied to the elective burn reconstruction population, these systematic approaches may allow surgical throughput to normalize, allowing patients to undergo surgery to improve quality of life.
Another option is to use ambulatory surgery centers. At our institution, we were in the midst of transitioning elective cases to our ambulatory surgery center at the onset of the pandemic, which coincides with the precipitous drop of burn scar laser procedures during the moratorium period and persistent decreased numbers in the late COVID period. Performing these elective cases at ambulatory surgery centers safely and without any significant increased risk of COVID-19 transmission benefits not only patients in that they can receive the care they need or desire, but also the hospitals in that they won’t have the burden of allocating scarce OR resources during these unpredictable resource-critical times. As such, a broader transition of elective cases to ambulatory surgery centers should be thoroughly evaluated and considered. Additionally, during periods in which ORs are stretched thin or closed entirely, ambulatory surgery centers may be a useful resource to assist acute care hospitals provide operative care.36,37
Along with managing the impact of canceled elective cases, hospitals also had to adapt operating procedures to ensure that COVID-19 safety guidelines were being followed for surgeries that were still being performed. Hospital systems needed to implement significant changes in the way operations were scheduled, rooms were cleaned, and patients were transported in order to ensure patient and staff safety. However, even with the implementation of these guidelines, the turnover and prep time between cases at our institution for burn procedures was not significantly different during any of the time-periods, which suggests that OR efficiency was not severely affected by the pandemic. This contrasts with other studies that report on changes in OR efficiency during the pandemic. Andreata and colleagues38 noted increases in first case delays, or delay from scheduled time to skin incision, and turnover times for orthopedic surgical cases in Northern Italy. A study of 1243 OR cases was conducted in four London Major Trauma Centers, and the authors described significant increases in the median time of paging for a patient and arrival to the operating room between the pre- and during-pandemic period.39 This decrease in OR efficiency may be attributed to staffing shortages or difficulties in administrative and/or practical implementation of new and unfamiliar protocols. Furthermore, pre-, peri-, and post-operative management of surgical patients becomes more complicated when the patients test positive for COVID-19. Physician–patient interactions become difficult to mitigate exposure, relying heavily on digital tracking tools, possibly leading to delayed management.40,41 In addition to changes and adaptations to operating room workflow, another area of interest that could not be effectively parsed out in our study are either institutional or departmental changes in operative decision making. Given the tremendous stress that COVID had placed on hospitals and their associated bed shortages, hospital administrators and/or providers may advocate for earlier or expedited intervention in order to limit patient time in the hospital and accelerate patient throughput to make more beds available. This is reflected in our own data by the increased volume of combined excision and grafting cases, which when combined with the absence of the shorter burn laser scar cases, resulted in longer projected and actual operative times. This would be particularly interesting due to the ongoing research looking into optimal timing of burn excision and specifically for early excision.
A potential reason for the relatively consistent OR efficiency at our institution compared to other studies could be related to typical patterns of operative intervention. Patients with significant burns requiring operative intervention are generally resuscitated prior to going to the OR. This allows time to determine the patient’s COVID status and can eliminate the need to prophylactically use a dedicated COVID OR. In emergent cases where minimizing time to the OR is essential, hospitals will either need to delay for the results of the COVID test, which were much slower during the beginning of the pandemic, or they would need to take the patient into a COVID OR due to their unknown status.
Limitations of this study include the retrospective nature of the data, the analysis is a database analysis as opposed to chart review, and this data represents the experience of only a single-institution. Although our selected time-periods for comparison would account for seasonal variability, COVID has continued to persist and has intermittently surged with new variants. Ideally, a fourth period representing a post-COVID period should be compared when available, however a foreseeable end to this pandemic is unclear at this time. Future studies should focus on how the COVID-19 pandemic has affected clinical outcomes in burn patients requiring operative intervention utilizing these similar time-periods.
CONCLUSIONS
COVID-19 related OR closures lead to an expected decrease in the number of overall cases and elective cases. However, there was no significant decline in the number of burn specific cases performed. The elective cases were largely replaced with excision and grafting cases and this shift has persisted even after elective cases have resumed. This change is also reflected in increased operative times.
Funding: No funding was obtained or used for this study.
Conflict of interest statement. None of the authors have any conflicts of interests or relevant financial disclosures.
Presented at: the 2022 Annual American Burn Association Meeting in Las Vegas, NV as an oral presentation.



