-
PDF
- Split View
-
Views
-
Cite
Cite
Junyao Zheng, Yongbo Lu, Wenjie Li, Bin Zhu, Fan Yang, Jie Shen, Prevalence and determinants of defensive medicine among physicians: a systematic review and meta-analysis, International Journal for Quality in Health Care, Volume 35, Issue 4, 2023, mzad096, https://doi.org/10.1093/intqhc/mzad096
Close - Share Icon Share
Abstract
Defensive medicine, characterized by physicians’ inclination toward excessive diagnostic tests and procedures, has emerged as a significant concern in modern healthcare due to its high prevalence and detrimental effects. Despite the growing concerns among healthcare providers, policymakers, and physicians, comprehensive synthesis of the literature on the prevalence and determinants of defensive medicine among physicians has yet been reported. A comprehensive literature search was conducted to identify eligible studies published between 1 January 2000 and 31 December 2022, utilizing six databases (i.e. Web of Science, PubMed, Embase, Scopus, PsycINFO, and Cochrane Library). A meta-analysis was conducted to determine the prevalence and determinants of defensive medicine. Of the 8892 identified articles, 64 eligible studies involving 35.9 thousand physicians across 23 countries were included. The overall pooled prevalence of defense medications was 75.8%. Physicians engaged in both assurance and avoidance behaviors, with the most prevalent subitems being increasing follow-up and avoidance of high-complication treatment protocols. The prevalence of defensive medicine was higher in the African region [88.1%; 95% confidence interval (CI): 80.4%–95.8%] and lower-middle-income countries (89.0%; 95% CI: 78.2%–99.8%). Among the medical specialties, anesthesiologists (92.2%; 95% CI: 89.2%–95.3%) exhibited the highest prevalence. Further, the pooled odds ratios (ORs) of the nine factors at the individual, relational, and organizational levels were calculated, and the influence of previous experience in medical-legal litigation (OR: 1.65; 95% CI: 1.13–2.18) should be considered. The results of this study indicate a high global prevalence of defensive medicine among physicians, underscoring the necessity of implementing targeted interventions to reduce its use, especially in certain regions and specialties. Policymakers should implement measures to improve physicians’ medical skills, enhance physician–patient communication, address physicians’ medical-legal litigation fears, and reform the medical liability system. Future research should focus on devising and assessing interventions to reduce the use of defensive medicine and to improve the quality of patient care.
Introduction
Defensive medicine has become a prominent issue in contemporary healthcare, marked by physicians’ tendency to order excessive diagnostic tests, procedures, or referrals and avoid certain patients and procedures [1, 2]. It is often motivated by concerns about litigation and malpractice claims rather than by patients’ best interests, potentially decreasing the quality while increasing the costs of patient care [3]. Previous studies indicate that defensive medicine can be divided into assurance and avoidance behavior [4, 5]. Assurance behavior is regarded as a positive defensive medicine that prevents unnecessary and additional medical treatments [6], whereas avoidance behavior is considered a negative defense behavior. Owing to the fear of becoming involved in medical litigation, physicians implement avoidance behaviors by avoiding high-risk procedures or patients [7]. These phenomena have been linked to various negative outcomes, including increased healthcare costs, reduced quality of care, and patient harm [8–10].
The prevalence of defensive medicine significantly varies across countries and specialties. A comprehensive national study revealed that 92% of physicians in the USA engaged in defensive medicine practices [10]. In contrast, European data indicated that 74.4% of Belgian physicians and 45.39% of Spanish physicians reported employing such practices [11, 12]. Moreover, physicians of different specialties were found to have different degree of defensive medicine utilization. Several factors have been identified as the determinants, including practice type [4], previous experiences with medical-legal litigation [13, 14], and pressure from patients or colleagues [13]. Moreover, healthcare system factors such as reimbursement policies, quality metrics, and regulatory requirements may also contribute to the prevalence of defensive medicine [3, 15].
To date, there has been no comprehensive synthesis of existing literature on the prevalence and determinants of defensive medicine among physicians. By identifying the prevalence and determinants of defensive medicine among physicians, this systematic review aimed to inform the development of targeted interventions to reduce defensive medicine practices and promote high-quality patient-centered care.
Methods
Data sources and search strategy
As defensive medicine is a multifaceted phenomenon involving medicine, law, and society, multiple electronic literature databases were used. In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16], we conducted a comprehensive literature search spanning from 1 January 2000 to 31 December 2022 across six major and comprehensive databases: Web of Science, PubMed, Embase, Scopus, PsycINFO, and the Cochrane Library. A broad search strategy was used to minimize the risk of bias. Based on the standardized Medical Subject Headings term ‘defensive medicine’ in the PubMed database, four groups of keywords were generated. The full search strategy is shown in Supplemental File 1.
EndNote software (version 20) was employed to manage the citations.
Eligibility criteria
The following eligibility criteria were defined: (i) defensive medicine was performed by or related to practicing physicians from any specialty; (ii) the concept of defensive medicine was clearly defined; (iii) the prevalence of defensive medicine among physicians was explicitly reported, including both overall and subitems; (iv) studies that reported defensive medicine among physicians not in emergencies or extreme circumstances (such as warfare or pandemic); (v) original studies being published in peer-reviewed journals; (vi) full text was available; and (vii) for duplicate publications, the most extensive studies were included.
Study selection and data extraction
Two investigators independently screened the titles and abstracts generated by the search strategy. Once one of the investigators determined that an abstract was eligible, a full-text article was obtained. Subsequently, two investigators examined the full texts and assessed the final study inclusion by referring to the eligibility criteria. Disagreements were resolved by a third investigator. To determine whether additional articles should be included, the reference lists of the included studies were manually searched. Finally, all investigators participated in data extraction.
Information about defensive medicine and its determinants was extracted from each included study using a standardized form (Table 1). Descriptive details included the first author, year of publication, research location, medical specialty investigated, sample size, outcome dimensions, influencing factors, and definition of defensive medicine. The authors of the included studies were contacted for additional clarification or data if needed.
| No . | First author . | Publication year . | Location . | Specialty . | Sample size . | Outcome dimension . | Influencing factorsh . | Definition of defensive medicine . |
|---|---|---|---|---|---|---|---|---|
| 1 | Summerton | 2000 | UK | General practitioners | 339 | Subitems | N/A | Ordering of treatments, tests, and procedures for the purpose of protecting the doctor from criticism rather than diagnosing or treating the patient |
| 2 | Symon | 2000 | UK | Midwives and obstetrician | 211 | Overall | N/A | Personally changed practice as a result of the fear of litigation |
| 3 | Passmore | 2002 | UK | Psychiatrists | 95 | Overall | N/A | Ordering of treatments, tests, and procedures for the purpose of protecting the doctor from criticism rather than diagnosing or treating the patient |
| 4 | Toker | 2004 | Israel | Ear, nose, and throat physicians | 194 | Subitems | N/A | A physician’s deviation from what is considered to be good practice to prevent complaints from patients or their families |
| 5 | Studdert | 2005 | USA | Multiple specialtiesa | 824 | Subitems | Gender, insurance coverage, premium burden, experience of being dropped by insurer practice type, and working experience | Physicians alter their clinical behavior because of the threat of malpractice liability |
| 6 | Sánchez-González | 2005 | Mexico | Unclear | 613 | Overall | N/A | Application of treatments, tests, and procedures with the explicit main purpose of defending the doctor from criticism, having documentary evidence in the event of a lawsuit and avoiding controversies, over and above the diagnosis or treatment of the patient |
| 7 | Hiyama | 2006 | Japan | Gastroenterologists | 131 | Overall | Working experience and practice type | A deviation from sound medical practice that is induced primarily by the threat of liability claims |
| 8 | Krawitz | 2006 | New Zealand | Clinician | 26 | Overall | Public and mass media attention, Ministry of Health, requests by superiors to practice defensive medicine, and politicians and policy | Taken a treatment approach not likely to be in the client’s best interest but protects from medicolegal repercussions |
| 9 | Mullen | 2008 | New Zealand | Psychiatrists | 86 | Subitems | N/A | Additional effort, of marginal clinical utility, is made to avoid complaint or legal liability |
| 10 | Catino | 2009 | Italy | General practitioners | 307 | Overall | Fear of a request for compensation, fear of medical-legal litigation, fear of disciplinary sanctions, fear of negative publicity, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | Healthcare personnel order unnecessary treatments (positive defensive medicine) or avoid high-risk procedures or patients (negative defensive medicine) with the principle—though not exclusive—aim of reducing their exposure to damages claims |
| 11 | Catino | 2009 | Italy | General practitioners, anesthetists, and surgeons | 102 | Overall | Age, fear of a request for compensation, fear of medical-legal litigation, fear of disciplinary sanctions, fear of negative publicity, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | Healthcare personnel effect unnecessary treatments or avoid high-risk procedures, with the principle—though not exclusive—aim of reducing their exposure to malpractice litigation |
| 12 | Bishop | 2010 | USA | Multiple specialtiesb | 1231 | Overall | Gender, practice location (rural or urban), practice type, source of income, and hour-long patient care | Physicians order more tests and procedures than patients need to protect themselves from malpractice suits |
| 13 | Nash | 2010 | Australia | Multiple specialtiesb | 2999 | Subitems | Previous personal experience of medical-legal litigation | Perceived change in practice behavior due to concerns about medicolegal negligence claims and complaints |
| 14 | Anderson | 2011 | USA | Obstetrician/gynecologists | 241 | Subitems | Age, career satisfaction, previous personal experience of medical-legal litigation, insurance premium evolution, and malpractice crisis level of the region | Changes in practices due to malpractice concern |
| 15 | Leary | 2011 | USA | Residents (surgical versus medical) | 76 | Overall | N/A | A deviation from sound medical practice that physicians engage in primarily because they perceive a threat of liability |
| 16 | Asher | 2012 | Israel | Multiple specialtiesc | 877 | Overall | Age, gender, specialty, previous personal experience of medical-legal litigation, exposure to complaint, practice type, managerial job, career satisfaction, and owning private malpractice insurance | Ordering of tests, procedures, and visits or the avoidance of high-risk patients or procedures, primarily to reduce exposure to malpractice liability |
| 17 | Nahed | 2012 | USA | Neurosurgeons | 1028 | Subitems | N/A | Perception changes actions solely to mitigate liability risk |
| 18 | Manish | 2012 | USA | Plastic and aesthetic surgeons | 1214 | Subitems | N/A | Medical practices that may exonerate physicians from liability without significant benefit to patients |
| 19 | Asher | 2013 | Israel | Obstetrician/gynecologists | 117 | Subitems | Age, gender, concern over potential medicolegal litigation, practice location (rural or urban), and professional status | Medical actions, performed mainly in order to refrain from being sued rather than actually aiding the patient |
| 20 | Ortashi | 2013 | UK | Unclear | 204 | Overall | Age, gender, technical title, and specialty | A doctor’s deviation from their usual behavior or that considered good practice, to reduce or prevent complaints or criticism by patients or their families |
| 21 | Prieto-Miranda | 2013 | Mexico | Multiple specialtiesd | 246 | Overall | Age, gender, work shifts, specialty, professional certification, working experience, and previous personal experience of medical-legal litigation | Aapplication of treatments, performance of diagnostic tests and therapeutic procedures, more than with the objective of diagnosing and adequately treating the patient, with the main purpose of defending the doctor from criticism, in addition to having documentary evidence in the event of a lawsuit and avoiding controversies |
| 22 | Jingwei | 2014 | China | Unclear | 504 | Overall | Gender, working experience, education, specialty, technical title, monthly payroll income, workload, type of hospital, and exposure to medical dispute | Medical practice based on fear of legal liability rather than on patients’ best interests |
| 23 | Moosazadeh | 2014 | Iran | General practitioners | 423 | Subitems | Age, gender, working experience, insurance coverage, and previous experience of a colleague being subject to medical-legal litigation | Every therapeutic test or method, whose primary aim is to protect the physician against the threat of being accused of making a forensic medicine mistake or of being sued for medical mistakes |
| 24 | Roytowski | 2014 | South Africa | Neurosurgeons | 66 | Subitems | N/A | Changing practice behavior to try to minimize the risk of a lawsuit |
| 25 | Solaroglu | 2014 | Turkey | Neurosurgeons | 404 | Overall | Gender, working experience, types of hospital, and the geographic regions | Medical practices that help doctors avoid liability without providing any additional benefit to the patient |
| 26 | Bourne | 2015 | UK | Multiple specialties | 7926 | Subitems | Exposure to complaint, length of investigation, outcome of investigation, complaint source, and type of complaint | Broadly categorized into ‘hedging’ and ‘avoidance’. Hedging is when doctors are overcautious, leading to overprescribing, referring too many patients or over investigation. Avoidance includes not taking on complicated patients and avoiding certain procedures or more difficult cases |
| 27 | Motta | 2015 | Italy | Otolaryngology | 100 | Overall | Concern over potential medicolegal disputes, concern over variations in the doctor/patient relationship, and knowledge of insurance clauses | Defensive medicine is defined as the ordering of tests and procedures (positive defensive medicine) or the avoidance of high-risk patients or procedures (negative defensive medicine), primarily to reduce exposure to malpractice liability |
| 28 | Osti | 2015 | Austria | Multiple specialtiese | 193 | Overall | N/A | Medical practices that may exonerate doctors from liability without significant benefit to patients |
| 29 | Reisch | 2015 | USA | Breast pathologists | 252 | Overall | Age, gender, geographic region, medical skills training, previous personal experience of medical-legal litigation, working experience, workloads, and exposure to medical malpractice | A deviation from standard medical practice induced primarily by a threat of liability |
| 30 | Smith | 2015 | USA | Neurosurgeons | 1026 | Overall | Working experience, reimbursement patterns, claims history, insurance coverage and cost, malpractice crisis level of the region, and patients with public insurance | An incentive to administer precautionary treatment with minimal expected medical benefit out of fear of litigation |
| 31 | Tanriverdi | 2015 | Turkey | Medical oncologists | 124 | Overall | Age, gender, academic occupation, working experience, type of hospital, and occupational status | Occasionally indulging unnecessary treatment requests to defend against lawsuits for medical errors and the use of unapproved medical applications |
| 32 | Abdel | 2016 | Sudan | Obstetrician/gynecologists | 117 | Overall | Working experience, professional certification, technical title, and type of hospital | A doctor’s deviation from the usual practice in order to reduce or prevent criticism and/or complaints by patients or their relatives |
| 33 | Panella | 2016 | Italy | Multiple specialties | 1313 | Overall | Age, gender, specialty, working experience, workload, and perception of being a ‘second victim’i | A deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims |
| 34 | Silberstein | 2016 | Israel | Plastic and aesthetic surgeons | 78 | Overall | Gender, working experience, managerial job, exposure to medicolegal literature, and requests by superiors to practice defensive medicine | Medical practices carried out primarily to avoid malpractice liability rather than to benefit the patient |
| 35 | Smith | 2016 | Canada | Neurosurgeons | 75 | Subitems | N/A | A deviation from regular medical practice because of medicolegal fears |
| 36 | Yan | 2016 | Cross-nationf | Neurosurgeons | 1142 | Overall | N/A | The practice of prescribing unnecessary medical care or avoiding high-risk situations out of fear of litigation |
| 37 | Din | 2017 | USA | Spine neurosurgery | 1024 | Overall | Malpractice crisis level of the region, premium burden, patients with public insurance, and exposure to malpractice claims | The provision of services beyond what is needed to improve patient outcomes (assurance behavior) and the evasion of high-risk procedures (avoidance behavior) to either deter litigation or substantiate clinical decision-making in the court |
| 38 | Olcay | 2017 | Turkey | Cardiologists | 253 | Overall | Previous personal experience of medical-legal litigation | Establishing diagnoses that would not alter patient care and performing unnecessary testing and treatments |
| 39 | Panella | 2017 | Italy | Multiple specialties | 1313 | Overall | Exposure to malpractice claims, fear of medical-legal litigation, fear of a request for compensation, fear of negative publicity, ineffective physician–patient relationship, insurance coverage, hospital support for liability issues, and public and mass media attention | A deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims |
| 40 | Ramírez-Alcántara | 2017 | Turkey | General practitioners | 87 | Overall | Work shifts | Application of treatments, performance of diagnostic tests and therapeutic procedures, more than with the aim of properly diagnosing and treating the patient, with the main purpose of defending the doctor from criticism, in addition to having documentary evidence in the event of a lawsuit and avoiding controversies |
| 41 | Reuveni | 2017 | Israel | Psychiatrists | 213 | Subitems | N/A | Medical actions that deviate from sound medical practice, performed primarily to reduce exposure to malpractice liability or to provide legal protection in the case of a malpractice lawsuit |
| 42 | Vandersteegen | 2017 | Belgium | Multiple specialties | 508 | Overall | Age, gender, region, working experience, insurance premium evolution, incitement by fund for medical accidents, consequences of medical lawsuit, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | The avoidance of certain high-risk procedures or patients or the ordering of procedures, tests, or visits, primarily (but not solely) due to the threat of medical liability |
| 43 | Yan | 2017 | Netherlands | Neurosurgeons | 45 | Subitems | N/A | A departure from standard medical practices out of fear of litigation |
| 44 | Tebano | 2018 | Cross-nationg | Antibiotic stewards | 830 | Subitems | Specialty, geographic regions, age, type of employment (contract or permanent), and fear of medical-legal litigation | When physicians perceive litigation as a threat, they may adopt defensive behaviors as a way to reduce the chances of litigation or to ensure a form of defense in the case of malpractice claims |
| 45 | Titus | 2018 | USA | Melanoma pathologists | 207 | Subitems | N/A | Behaviors that are intended to reduce exposure to malpractice litigation but may not clinically benefit the patient |
| 46 | Zhu | 2018 | China | Obstetrician/gynecologists | 1486 | Overall | Gender, level of hospital, education, specialty, exposure to medical dispute, previous personal experience of medical-legal litigation, consequences of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | The alterations of modes of medical practice, induced by the threat of liability, for the principal purposes of forestalling lawsuits by patients as well as providing good legal defense in the event that such lawsuits are instituted |
| 47 | Delice | 2019 | Turkey | Emergency medical specialists | 321 | Overall | N/A | Physicians requesting additional tests in the absence of indications or else avoiding high-risk patient groups in which adverse outcomes may occur during diagnosis and treatment |
| 48 | Ionescu | 2019 | Romania | Obstetrician/gynecologists | 73 | Overall | Working experience | A cesarean delivery recommended by the doctor in the absence of any clear medical indication that such a delivery method is needed to avoid possible litigation or a possible accusation of malpractice (defensive cesarean section) |
| 49 | Renkema | 2019 | Netherlands | Multiple specialties | 214 | Subitems | Age, specialty, technical title, attitude toward justified/unjustified litigation, and perceived patient pressure | The ordering of extra tests or procedures (assurance behavior) or the avoidance of high-risk patients or procedures (avoidance behavior), primarily to reduce the risk of being held liable for malpractice |
| 50 | Qiao | 2019 | China | Multiple specialties | 226 | Overall | N/A | Prescribe procedures or diagnostic tests or drugs that are clinically unnecessary to avoid possible troubles (such as lawsuits and disputes) |
| 51 | Garg | 2020 | India | Neurosurgeons | 214 | Subitems | Working experience and practice type | Clinical and operative practices to prevent medicolegal issues |
| 52 | Borgan | 2020 | USA | Internal medicine residents | 49 | Subitems | N/A | The deviation from routine medical care in order to avoid or reduce the risk of real or perceived future legal consequences |
| 53 | Calikoglu | 2020 | Turkey | Surgeons | 190 | Overall | Gender, academic occupation, specialty, and previous personal experience of medical-legal litigation | Medical behaviors that avoid physician liability without providing increased benefits to the patient |
| 54 | Gadjradj | 2020 | Cross-nation | Neurosurgeons | 490 | Subitems | N/A | Perform unnecessary, additional therapeutic or diagnostic interventions that do not improve the medical condition of the patient (positive defensive medicine), or it may cause physicians to refer or refuse difficult cases (negative defensive medicine) |
| 55 | Abbass | 2021 | Egypt | Multiple specialties | 261 | Subitems | Gender and specialty | The overuse of the resources such as ordering unnecessary investigations, giving treatment, or performing procedures aiming at doctors’ self-protection against claims rather than for the patient best interest |
| 56 | Fineschi | 2021 | Italy | Obstetrician/gynecologists | 168 | Subitems | N/A | The practice of recommending a diagnostic test or medical treatment (positive defensive medicine) or avoidance of risky patients or procedures (negative defensive medicine) that serves the function to protect physicians against patients’ claims |
| 57 | Kolcu | 2021 | Turkey | General practitioners | 196 | Subitems | N/A | The cost-increasing, defensive, or avoidance behavior displayed by physicians in healthcare delivery in order to protect themselves from legal problems |
| 58 | Perea-Pérez | 2021 | Spain | Emergency physicians | 1449 | Subitems | N/A | The making of clinical decisions that, while being explainable, prioritize the doctor’s legal security over other healthcare considerations |
| 59 | Rudey | 2021 | Brazil | Obstetrician/gynecologists | 403 | Overall | Gender, working experience, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | A practice wherein a healthcare professional makes decisions out of fear of litigation and not for the benefit of the patients |
| 60 | Ekici | 2021 | Turkey | Oral and maxillofacial surgeons | 109 | Subitems | N/A | A medical behavior that avoids medical responsibility without offering the patient greater benefits |
| 61 | Tumelty | 2021 | Ireland | Surgeons | 157 | Subitems | N/A | Behaviors engaged in by physicians for the purposes of averting the threat of medical negligence litigation and/or complaints |
| 62 | Zaed | 2021 | Italy | Neurosurgeons | 64 | Subitems | N/A | The practice of prescribing unnecessary medical care to minimize litigation exposure (positive defensive medicine) or the practice of avoiding more risky, albeit important, treatment measures to avoid litigation exposure (negative defensive medicine) |
| 63 | Vizcaino-Rakosnik | 2022 | Spain | Unclear | 282 | Overall | N/A | Made changes in their clinical practice because of the experience of being claimed |
| 64 | Shehata | 2022 | Egypt | Anesthesiologists | 177 | Subitems | Age, gender, marital status, technical title, professional certification, practice location, and type of employment (contract or permanent) | Defensive medicine occurs when doctors order tests, procedures, or visits or avoid high-risk patients or procedures, primarily (but not necessarily or solely) to reduce their exposure to malpractice liability |
| No . | First author . | Publication year . | Location . | Specialty . | Sample size . | Outcome dimension . | Influencing factorsh . | Definition of defensive medicine . |
|---|---|---|---|---|---|---|---|---|
| 1 | Summerton | 2000 | UK | General practitioners | 339 | Subitems | N/A | Ordering of treatments, tests, and procedures for the purpose of protecting the doctor from criticism rather than diagnosing or treating the patient |
| 2 | Symon | 2000 | UK | Midwives and obstetrician | 211 | Overall | N/A | Personally changed practice as a result of the fear of litigation |
| 3 | Passmore | 2002 | UK | Psychiatrists | 95 | Overall | N/A | Ordering of treatments, tests, and procedures for the purpose of protecting the doctor from criticism rather than diagnosing or treating the patient |
| 4 | Toker | 2004 | Israel | Ear, nose, and throat physicians | 194 | Subitems | N/A | A physician’s deviation from what is considered to be good practice to prevent complaints from patients or their families |
| 5 | Studdert | 2005 | USA | Multiple specialtiesa | 824 | Subitems | Gender, insurance coverage, premium burden, experience of being dropped by insurer practice type, and working experience | Physicians alter their clinical behavior because of the threat of malpractice liability |
| 6 | Sánchez-González | 2005 | Mexico | Unclear | 613 | Overall | N/A | Application of treatments, tests, and procedures with the explicit main purpose of defending the doctor from criticism, having documentary evidence in the event of a lawsuit and avoiding controversies, over and above the diagnosis or treatment of the patient |
| 7 | Hiyama | 2006 | Japan | Gastroenterologists | 131 | Overall | Working experience and practice type | A deviation from sound medical practice that is induced primarily by the threat of liability claims |
| 8 | Krawitz | 2006 | New Zealand | Clinician | 26 | Overall | Public and mass media attention, Ministry of Health, requests by superiors to practice defensive medicine, and politicians and policy | Taken a treatment approach not likely to be in the client’s best interest but protects from medicolegal repercussions |
| 9 | Mullen | 2008 | New Zealand | Psychiatrists | 86 | Subitems | N/A | Additional effort, of marginal clinical utility, is made to avoid complaint or legal liability |
| 10 | Catino | 2009 | Italy | General practitioners | 307 | Overall | Fear of a request for compensation, fear of medical-legal litigation, fear of disciplinary sanctions, fear of negative publicity, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | Healthcare personnel order unnecessary treatments (positive defensive medicine) or avoid high-risk procedures or patients (negative defensive medicine) with the principle—though not exclusive—aim of reducing their exposure to damages claims |
| 11 | Catino | 2009 | Italy | General practitioners, anesthetists, and surgeons | 102 | Overall | Age, fear of a request for compensation, fear of medical-legal litigation, fear of disciplinary sanctions, fear of negative publicity, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | Healthcare personnel effect unnecessary treatments or avoid high-risk procedures, with the principle—though not exclusive—aim of reducing their exposure to malpractice litigation |
| 12 | Bishop | 2010 | USA | Multiple specialtiesb | 1231 | Overall | Gender, practice location (rural or urban), practice type, source of income, and hour-long patient care | Physicians order more tests and procedures than patients need to protect themselves from malpractice suits |
| 13 | Nash | 2010 | Australia | Multiple specialtiesb | 2999 | Subitems | Previous personal experience of medical-legal litigation | Perceived change in practice behavior due to concerns about medicolegal negligence claims and complaints |
| 14 | Anderson | 2011 | USA | Obstetrician/gynecologists | 241 | Subitems | Age, career satisfaction, previous personal experience of medical-legal litigation, insurance premium evolution, and malpractice crisis level of the region | Changes in practices due to malpractice concern |
| 15 | Leary | 2011 | USA | Residents (surgical versus medical) | 76 | Overall | N/A | A deviation from sound medical practice that physicians engage in primarily because they perceive a threat of liability |
| 16 | Asher | 2012 | Israel | Multiple specialtiesc | 877 | Overall | Age, gender, specialty, previous personal experience of medical-legal litigation, exposure to complaint, practice type, managerial job, career satisfaction, and owning private malpractice insurance | Ordering of tests, procedures, and visits or the avoidance of high-risk patients or procedures, primarily to reduce exposure to malpractice liability |
| 17 | Nahed | 2012 | USA | Neurosurgeons | 1028 | Subitems | N/A | Perception changes actions solely to mitigate liability risk |
| 18 | Manish | 2012 | USA | Plastic and aesthetic surgeons | 1214 | Subitems | N/A | Medical practices that may exonerate physicians from liability without significant benefit to patients |
| 19 | Asher | 2013 | Israel | Obstetrician/gynecologists | 117 | Subitems | Age, gender, concern over potential medicolegal litigation, practice location (rural or urban), and professional status | Medical actions, performed mainly in order to refrain from being sued rather than actually aiding the patient |
| 20 | Ortashi | 2013 | UK | Unclear | 204 | Overall | Age, gender, technical title, and specialty | A doctor’s deviation from their usual behavior or that considered good practice, to reduce or prevent complaints or criticism by patients or their families |
| 21 | Prieto-Miranda | 2013 | Mexico | Multiple specialtiesd | 246 | Overall | Age, gender, work shifts, specialty, professional certification, working experience, and previous personal experience of medical-legal litigation | Aapplication of treatments, performance of diagnostic tests and therapeutic procedures, more than with the objective of diagnosing and adequately treating the patient, with the main purpose of defending the doctor from criticism, in addition to having documentary evidence in the event of a lawsuit and avoiding controversies |
| 22 | Jingwei | 2014 | China | Unclear | 504 | Overall | Gender, working experience, education, specialty, technical title, monthly payroll income, workload, type of hospital, and exposure to medical dispute | Medical practice based on fear of legal liability rather than on patients’ best interests |
| 23 | Moosazadeh | 2014 | Iran | General practitioners | 423 | Subitems | Age, gender, working experience, insurance coverage, and previous experience of a colleague being subject to medical-legal litigation | Every therapeutic test or method, whose primary aim is to protect the physician against the threat of being accused of making a forensic medicine mistake or of being sued for medical mistakes |
| 24 | Roytowski | 2014 | South Africa | Neurosurgeons | 66 | Subitems | N/A | Changing practice behavior to try to minimize the risk of a lawsuit |
| 25 | Solaroglu | 2014 | Turkey | Neurosurgeons | 404 | Overall | Gender, working experience, types of hospital, and the geographic regions | Medical practices that help doctors avoid liability without providing any additional benefit to the patient |
| 26 | Bourne | 2015 | UK | Multiple specialties | 7926 | Subitems | Exposure to complaint, length of investigation, outcome of investigation, complaint source, and type of complaint | Broadly categorized into ‘hedging’ and ‘avoidance’. Hedging is when doctors are overcautious, leading to overprescribing, referring too many patients or over investigation. Avoidance includes not taking on complicated patients and avoiding certain procedures or more difficult cases |
| 27 | Motta | 2015 | Italy | Otolaryngology | 100 | Overall | Concern over potential medicolegal disputes, concern over variations in the doctor/patient relationship, and knowledge of insurance clauses | Defensive medicine is defined as the ordering of tests and procedures (positive defensive medicine) or the avoidance of high-risk patients or procedures (negative defensive medicine), primarily to reduce exposure to malpractice liability |
| 28 | Osti | 2015 | Austria | Multiple specialtiese | 193 | Overall | N/A | Medical practices that may exonerate doctors from liability without significant benefit to patients |
| 29 | Reisch | 2015 | USA | Breast pathologists | 252 | Overall | Age, gender, geographic region, medical skills training, previous personal experience of medical-legal litigation, working experience, workloads, and exposure to medical malpractice | A deviation from standard medical practice induced primarily by a threat of liability |
| 30 | Smith | 2015 | USA | Neurosurgeons | 1026 | Overall | Working experience, reimbursement patterns, claims history, insurance coverage and cost, malpractice crisis level of the region, and patients with public insurance | An incentive to administer precautionary treatment with minimal expected medical benefit out of fear of litigation |
| 31 | Tanriverdi | 2015 | Turkey | Medical oncologists | 124 | Overall | Age, gender, academic occupation, working experience, type of hospital, and occupational status | Occasionally indulging unnecessary treatment requests to defend against lawsuits for medical errors and the use of unapproved medical applications |
| 32 | Abdel | 2016 | Sudan | Obstetrician/gynecologists | 117 | Overall | Working experience, professional certification, technical title, and type of hospital | A doctor’s deviation from the usual practice in order to reduce or prevent criticism and/or complaints by patients or their relatives |
| 33 | Panella | 2016 | Italy | Multiple specialties | 1313 | Overall | Age, gender, specialty, working experience, workload, and perception of being a ‘second victim’i | A deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims |
| 34 | Silberstein | 2016 | Israel | Plastic and aesthetic surgeons | 78 | Overall | Gender, working experience, managerial job, exposure to medicolegal literature, and requests by superiors to practice defensive medicine | Medical practices carried out primarily to avoid malpractice liability rather than to benefit the patient |
| 35 | Smith | 2016 | Canada | Neurosurgeons | 75 | Subitems | N/A | A deviation from regular medical practice because of medicolegal fears |
| 36 | Yan | 2016 | Cross-nationf | Neurosurgeons | 1142 | Overall | N/A | The practice of prescribing unnecessary medical care or avoiding high-risk situations out of fear of litigation |
| 37 | Din | 2017 | USA | Spine neurosurgery | 1024 | Overall | Malpractice crisis level of the region, premium burden, patients with public insurance, and exposure to malpractice claims | The provision of services beyond what is needed to improve patient outcomes (assurance behavior) and the evasion of high-risk procedures (avoidance behavior) to either deter litigation or substantiate clinical decision-making in the court |
| 38 | Olcay | 2017 | Turkey | Cardiologists | 253 | Overall | Previous personal experience of medical-legal litigation | Establishing diagnoses that would not alter patient care and performing unnecessary testing and treatments |
| 39 | Panella | 2017 | Italy | Multiple specialties | 1313 | Overall | Exposure to malpractice claims, fear of medical-legal litigation, fear of a request for compensation, fear of negative publicity, ineffective physician–patient relationship, insurance coverage, hospital support for liability issues, and public and mass media attention | A deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims |
| 40 | Ramírez-Alcántara | 2017 | Turkey | General practitioners | 87 | Overall | Work shifts | Application of treatments, performance of diagnostic tests and therapeutic procedures, more than with the aim of properly diagnosing and treating the patient, with the main purpose of defending the doctor from criticism, in addition to having documentary evidence in the event of a lawsuit and avoiding controversies |
| 41 | Reuveni | 2017 | Israel | Psychiatrists | 213 | Subitems | N/A | Medical actions that deviate from sound medical practice, performed primarily to reduce exposure to malpractice liability or to provide legal protection in the case of a malpractice lawsuit |
| 42 | Vandersteegen | 2017 | Belgium | Multiple specialties | 508 | Overall | Age, gender, region, working experience, insurance premium evolution, incitement by fund for medical accidents, consequences of medical lawsuit, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | The avoidance of certain high-risk procedures or patients or the ordering of procedures, tests, or visits, primarily (but not solely) due to the threat of medical liability |
| 43 | Yan | 2017 | Netherlands | Neurosurgeons | 45 | Subitems | N/A | A departure from standard medical practices out of fear of litigation |
| 44 | Tebano | 2018 | Cross-nationg | Antibiotic stewards | 830 | Subitems | Specialty, geographic regions, age, type of employment (contract or permanent), and fear of medical-legal litigation | When physicians perceive litigation as a threat, they may adopt defensive behaviors as a way to reduce the chances of litigation or to ensure a form of defense in the case of malpractice claims |
| 45 | Titus | 2018 | USA | Melanoma pathologists | 207 | Subitems | N/A | Behaviors that are intended to reduce exposure to malpractice litigation but may not clinically benefit the patient |
| 46 | Zhu | 2018 | China | Obstetrician/gynecologists | 1486 | Overall | Gender, level of hospital, education, specialty, exposure to medical dispute, previous personal experience of medical-legal litigation, consequences of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | The alterations of modes of medical practice, induced by the threat of liability, for the principal purposes of forestalling lawsuits by patients as well as providing good legal defense in the event that such lawsuits are instituted |
| 47 | Delice | 2019 | Turkey | Emergency medical specialists | 321 | Overall | N/A | Physicians requesting additional tests in the absence of indications or else avoiding high-risk patient groups in which adverse outcomes may occur during diagnosis and treatment |
| 48 | Ionescu | 2019 | Romania | Obstetrician/gynecologists | 73 | Overall | Working experience | A cesarean delivery recommended by the doctor in the absence of any clear medical indication that such a delivery method is needed to avoid possible litigation or a possible accusation of malpractice (defensive cesarean section) |
| 49 | Renkema | 2019 | Netherlands | Multiple specialties | 214 | Subitems | Age, specialty, technical title, attitude toward justified/unjustified litigation, and perceived patient pressure | The ordering of extra tests or procedures (assurance behavior) or the avoidance of high-risk patients or procedures (avoidance behavior), primarily to reduce the risk of being held liable for malpractice |
| 50 | Qiao | 2019 | China | Multiple specialties | 226 | Overall | N/A | Prescribe procedures or diagnostic tests or drugs that are clinically unnecessary to avoid possible troubles (such as lawsuits and disputes) |
| 51 | Garg | 2020 | India | Neurosurgeons | 214 | Subitems | Working experience and practice type | Clinical and operative practices to prevent medicolegal issues |
| 52 | Borgan | 2020 | USA | Internal medicine residents | 49 | Subitems | N/A | The deviation from routine medical care in order to avoid or reduce the risk of real or perceived future legal consequences |
| 53 | Calikoglu | 2020 | Turkey | Surgeons | 190 | Overall | Gender, academic occupation, specialty, and previous personal experience of medical-legal litigation | Medical behaviors that avoid physician liability without providing increased benefits to the patient |
| 54 | Gadjradj | 2020 | Cross-nation | Neurosurgeons | 490 | Subitems | N/A | Perform unnecessary, additional therapeutic or diagnostic interventions that do not improve the medical condition of the patient (positive defensive medicine), or it may cause physicians to refer or refuse difficult cases (negative defensive medicine) |
| 55 | Abbass | 2021 | Egypt | Multiple specialties | 261 | Subitems | Gender and specialty | The overuse of the resources such as ordering unnecessary investigations, giving treatment, or performing procedures aiming at doctors’ self-protection against claims rather than for the patient best interest |
| 56 | Fineschi | 2021 | Italy | Obstetrician/gynecologists | 168 | Subitems | N/A | The practice of recommending a diagnostic test or medical treatment (positive defensive medicine) or avoidance of risky patients or procedures (negative defensive medicine) that serves the function to protect physicians against patients’ claims |
| 57 | Kolcu | 2021 | Turkey | General practitioners | 196 | Subitems | N/A | The cost-increasing, defensive, or avoidance behavior displayed by physicians in healthcare delivery in order to protect themselves from legal problems |
| 58 | Perea-Pérez | 2021 | Spain | Emergency physicians | 1449 | Subitems | N/A | The making of clinical decisions that, while being explainable, prioritize the doctor’s legal security over other healthcare considerations |
| 59 | Rudey | 2021 | Brazil | Obstetrician/gynecologists | 403 | Overall | Gender, working experience, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | A practice wherein a healthcare professional makes decisions out of fear of litigation and not for the benefit of the patients |
| 60 | Ekici | 2021 | Turkey | Oral and maxillofacial surgeons | 109 | Subitems | N/A | A medical behavior that avoids medical responsibility without offering the patient greater benefits |
| 61 | Tumelty | 2021 | Ireland | Surgeons | 157 | Subitems | N/A | Behaviors engaged in by physicians for the purposes of averting the threat of medical negligence litigation and/or complaints |
| 62 | Zaed | 2021 | Italy | Neurosurgeons | 64 | Subitems | N/A | The practice of prescribing unnecessary medical care to minimize litigation exposure (positive defensive medicine) or the practice of avoiding more risky, albeit important, treatment measures to avoid litigation exposure (negative defensive medicine) |
| 63 | Vizcaino-Rakosnik | 2022 | Spain | Unclear | 282 | Overall | N/A | Made changes in their clinical practice because of the experience of being claimed |
| 64 | Shehata | 2022 | Egypt | Anesthesiologists | 177 | Subitems | Age, gender, marital status, technical title, professional certification, practice location, and type of employment (contract or permanent) | Defensive medicine occurs when doctors order tests, procedures, or visits or avoid high-risk patients or procedures, primarily (but not necessarily or solely) to reduce their exposure to malpractice liability |
General surgeons, radiologists, emergency physicians, orthopedic surgeons, obstetrician/gynecologists, and neurosurgeons.
Primary care, surgical specialists, nonsurgical specialists, and other specialists.
Obstetricians, gynecologists, physicians, surgeons, anesthetists, psychiatrists, pathologists, radiologists, pediatricians, accident, and emergency specialists.
Pediatricians, internists, obstetricians and gynecologists, orthopedic surgeons, family medicine practitioners, general surgeons, cardiologists, and neurosurgeons.
Orthopaedic surgeons, trauma surgeons, and radiologists.
USA, Canada, and South Africa.
Including 74 countries.
N/A: not applicable.
Second victim: a healthcare provider involved in an unanticipated adverse patient event, medical error, and/or a patient related injury, who becomes victimized in the sense that the provider is traumatized by the event.
| No . | First author . | Publication year . | Location . | Specialty . | Sample size . | Outcome dimension . | Influencing factorsh . | Definition of defensive medicine . |
|---|---|---|---|---|---|---|---|---|
| 1 | Summerton | 2000 | UK | General practitioners | 339 | Subitems | N/A | Ordering of treatments, tests, and procedures for the purpose of protecting the doctor from criticism rather than diagnosing or treating the patient |
| 2 | Symon | 2000 | UK | Midwives and obstetrician | 211 | Overall | N/A | Personally changed practice as a result of the fear of litigation |
| 3 | Passmore | 2002 | UK | Psychiatrists | 95 | Overall | N/A | Ordering of treatments, tests, and procedures for the purpose of protecting the doctor from criticism rather than diagnosing or treating the patient |
| 4 | Toker | 2004 | Israel | Ear, nose, and throat physicians | 194 | Subitems | N/A | A physician’s deviation from what is considered to be good practice to prevent complaints from patients or their families |
| 5 | Studdert | 2005 | USA | Multiple specialtiesa | 824 | Subitems | Gender, insurance coverage, premium burden, experience of being dropped by insurer practice type, and working experience | Physicians alter their clinical behavior because of the threat of malpractice liability |
| 6 | Sánchez-González | 2005 | Mexico | Unclear | 613 | Overall | N/A | Application of treatments, tests, and procedures with the explicit main purpose of defending the doctor from criticism, having documentary evidence in the event of a lawsuit and avoiding controversies, over and above the diagnosis or treatment of the patient |
| 7 | Hiyama | 2006 | Japan | Gastroenterologists | 131 | Overall | Working experience and practice type | A deviation from sound medical practice that is induced primarily by the threat of liability claims |
| 8 | Krawitz | 2006 | New Zealand | Clinician | 26 | Overall | Public and mass media attention, Ministry of Health, requests by superiors to practice defensive medicine, and politicians and policy | Taken a treatment approach not likely to be in the client’s best interest but protects from medicolegal repercussions |
| 9 | Mullen | 2008 | New Zealand | Psychiatrists | 86 | Subitems | N/A | Additional effort, of marginal clinical utility, is made to avoid complaint or legal liability |
| 10 | Catino | 2009 | Italy | General practitioners | 307 | Overall | Fear of a request for compensation, fear of medical-legal litigation, fear of disciplinary sanctions, fear of negative publicity, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | Healthcare personnel order unnecessary treatments (positive defensive medicine) or avoid high-risk procedures or patients (negative defensive medicine) with the principle—though not exclusive—aim of reducing their exposure to damages claims |
| 11 | Catino | 2009 | Italy | General practitioners, anesthetists, and surgeons | 102 | Overall | Age, fear of a request for compensation, fear of medical-legal litigation, fear of disciplinary sanctions, fear of negative publicity, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | Healthcare personnel effect unnecessary treatments or avoid high-risk procedures, with the principle—though not exclusive—aim of reducing their exposure to malpractice litigation |
| 12 | Bishop | 2010 | USA | Multiple specialtiesb | 1231 | Overall | Gender, practice location (rural or urban), practice type, source of income, and hour-long patient care | Physicians order more tests and procedures than patients need to protect themselves from malpractice suits |
| 13 | Nash | 2010 | Australia | Multiple specialtiesb | 2999 | Subitems | Previous personal experience of medical-legal litigation | Perceived change in practice behavior due to concerns about medicolegal negligence claims and complaints |
| 14 | Anderson | 2011 | USA | Obstetrician/gynecologists | 241 | Subitems | Age, career satisfaction, previous personal experience of medical-legal litigation, insurance premium evolution, and malpractice crisis level of the region | Changes in practices due to malpractice concern |
| 15 | Leary | 2011 | USA | Residents (surgical versus medical) | 76 | Overall | N/A | A deviation from sound medical practice that physicians engage in primarily because they perceive a threat of liability |
| 16 | Asher | 2012 | Israel | Multiple specialtiesc | 877 | Overall | Age, gender, specialty, previous personal experience of medical-legal litigation, exposure to complaint, practice type, managerial job, career satisfaction, and owning private malpractice insurance | Ordering of tests, procedures, and visits or the avoidance of high-risk patients or procedures, primarily to reduce exposure to malpractice liability |
| 17 | Nahed | 2012 | USA | Neurosurgeons | 1028 | Subitems | N/A | Perception changes actions solely to mitigate liability risk |
| 18 | Manish | 2012 | USA | Plastic and aesthetic surgeons | 1214 | Subitems | N/A | Medical practices that may exonerate physicians from liability without significant benefit to patients |
| 19 | Asher | 2013 | Israel | Obstetrician/gynecologists | 117 | Subitems | Age, gender, concern over potential medicolegal litigation, practice location (rural or urban), and professional status | Medical actions, performed mainly in order to refrain from being sued rather than actually aiding the patient |
| 20 | Ortashi | 2013 | UK | Unclear | 204 | Overall | Age, gender, technical title, and specialty | A doctor’s deviation from their usual behavior or that considered good practice, to reduce or prevent complaints or criticism by patients or their families |
| 21 | Prieto-Miranda | 2013 | Mexico | Multiple specialtiesd | 246 | Overall | Age, gender, work shifts, specialty, professional certification, working experience, and previous personal experience of medical-legal litigation | Aapplication of treatments, performance of diagnostic tests and therapeutic procedures, more than with the objective of diagnosing and adequately treating the patient, with the main purpose of defending the doctor from criticism, in addition to having documentary evidence in the event of a lawsuit and avoiding controversies |
| 22 | Jingwei | 2014 | China | Unclear | 504 | Overall | Gender, working experience, education, specialty, technical title, monthly payroll income, workload, type of hospital, and exposure to medical dispute | Medical practice based on fear of legal liability rather than on patients’ best interests |
| 23 | Moosazadeh | 2014 | Iran | General practitioners | 423 | Subitems | Age, gender, working experience, insurance coverage, and previous experience of a colleague being subject to medical-legal litigation | Every therapeutic test or method, whose primary aim is to protect the physician against the threat of being accused of making a forensic medicine mistake or of being sued for medical mistakes |
| 24 | Roytowski | 2014 | South Africa | Neurosurgeons | 66 | Subitems | N/A | Changing practice behavior to try to minimize the risk of a lawsuit |
| 25 | Solaroglu | 2014 | Turkey | Neurosurgeons | 404 | Overall | Gender, working experience, types of hospital, and the geographic regions | Medical practices that help doctors avoid liability without providing any additional benefit to the patient |
| 26 | Bourne | 2015 | UK | Multiple specialties | 7926 | Subitems | Exposure to complaint, length of investigation, outcome of investigation, complaint source, and type of complaint | Broadly categorized into ‘hedging’ and ‘avoidance’. Hedging is when doctors are overcautious, leading to overprescribing, referring too many patients or over investigation. Avoidance includes not taking on complicated patients and avoiding certain procedures or more difficult cases |
| 27 | Motta | 2015 | Italy | Otolaryngology | 100 | Overall | Concern over potential medicolegal disputes, concern over variations in the doctor/patient relationship, and knowledge of insurance clauses | Defensive medicine is defined as the ordering of tests and procedures (positive defensive medicine) or the avoidance of high-risk patients or procedures (negative defensive medicine), primarily to reduce exposure to malpractice liability |
| 28 | Osti | 2015 | Austria | Multiple specialtiese | 193 | Overall | N/A | Medical practices that may exonerate doctors from liability without significant benefit to patients |
| 29 | Reisch | 2015 | USA | Breast pathologists | 252 | Overall | Age, gender, geographic region, medical skills training, previous personal experience of medical-legal litigation, working experience, workloads, and exposure to medical malpractice | A deviation from standard medical practice induced primarily by a threat of liability |
| 30 | Smith | 2015 | USA | Neurosurgeons | 1026 | Overall | Working experience, reimbursement patterns, claims history, insurance coverage and cost, malpractice crisis level of the region, and patients with public insurance | An incentive to administer precautionary treatment with minimal expected medical benefit out of fear of litigation |
| 31 | Tanriverdi | 2015 | Turkey | Medical oncologists | 124 | Overall | Age, gender, academic occupation, working experience, type of hospital, and occupational status | Occasionally indulging unnecessary treatment requests to defend against lawsuits for medical errors and the use of unapproved medical applications |
| 32 | Abdel | 2016 | Sudan | Obstetrician/gynecologists | 117 | Overall | Working experience, professional certification, technical title, and type of hospital | A doctor’s deviation from the usual practice in order to reduce or prevent criticism and/or complaints by patients or their relatives |
| 33 | Panella | 2016 | Italy | Multiple specialties | 1313 | Overall | Age, gender, specialty, working experience, workload, and perception of being a ‘second victim’i | A deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims |
| 34 | Silberstein | 2016 | Israel | Plastic and aesthetic surgeons | 78 | Overall | Gender, working experience, managerial job, exposure to medicolegal literature, and requests by superiors to practice defensive medicine | Medical practices carried out primarily to avoid malpractice liability rather than to benefit the patient |
| 35 | Smith | 2016 | Canada | Neurosurgeons | 75 | Subitems | N/A | A deviation from regular medical practice because of medicolegal fears |
| 36 | Yan | 2016 | Cross-nationf | Neurosurgeons | 1142 | Overall | N/A | The practice of prescribing unnecessary medical care or avoiding high-risk situations out of fear of litigation |
| 37 | Din | 2017 | USA | Spine neurosurgery | 1024 | Overall | Malpractice crisis level of the region, premium burden, patients with public insurance, and exposure to malpractice claims | The provision of services beyond what is needed to improve patient outcomes (assurance behavior) and the evasion of high-risk procedures (avoidance behavior) to either deter litigation or substantiate clinical decision-making in the court |
| 38 | Olcay | 2017 | Turkey | Cardiologists | 253 | Overall | Previous personal experience of medical-legal litigation | Establishing diagnoses that would not alter patient care and performing unnecessary testing and treatments |
| 39 | Panella | 2017 | Italy | Multiple specialties | 1313 | Overall | Exposure to malpractice claims, fear of medical-legal litigation, fear of a request for compensation, fear of negative publicity, ineffective physician–patient relationship, insurance coverage, hospital support for liability issues, and public and mass media attention | A deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims |
| 40 | Ramírez-Alcántara | 2017 | Turkey | General practitioners | 87 | Overall | Work shifts | Application of treatments, performance of diagnostic tests and therapeutic procedures, more than with the aim of properly diagnosing and treating the patient, with the main purpose of defending the doctor from criticism, in addition to having documentary evidence in the event of a lawsuit and avoiding controversies |
| 41 | Reuveni | 2017 | Israel | Psychiatrists | 213 | Subitems | N/A | Medical actions that deviate from sound medical practice, performed primarily to reduce exposure to malpractice liability or to provide legal protection in the case of a malpractice lawsuit |
| 42 | Vandersteegen | 2017 | Belgium | Multiple specialties | 508 | Overall | Age, gender, region, working experience, insurance premium evolution, incitement by fund for medical accidents, consequences of medical lawsuit, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | The avoidance of certain high-risk procedures or patients or the ordering of procedures, tests, or visits, primarily (but not solely) due to the threat of medical liability |
| 43 | Yan | 2017 | Netherlands | Neurosurgeons | 45 | Subitems | N/A | A departure from standard medical practices out of fear of litigation |
| 44 | Tebano | 2018 | Cross-nationg | Antibiotic stewards | 830 | Subitems | Specialty, geographic regions, age, type of employment (contract or permanent), and fear of medical-legal litigation | When physicians perceive litigation as a threat, they may adopt defensive behaviors as a way to reduce the chances of litigation or to ensure a form of defense in the case of malpractice claims |
| 45 | Titus | 2018 | USA | Melanoma pathologists | 207 | Subitems | N/A | Behaviors that are intended to reduce exposure to malpractice litigation but may not clinically benefit the patient |
| 46 | Zhu | 2018 | China | Obstetrician/gynecologists | 1486 | Overall | Gender, level of hospital, education, specialty, exposure to medical dispute, previous personal experience of medical-legal litigation, consequences of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | The alterations of modes of medical practice, induced by the threat of liability, for the principal purposes of forestalling lawsuits by patients as well as providing good legal defense in the event that such lawsuits are instituted |
| 47 | Delice | 2019 | Turkey | Emergency medical specialists | 321 | Overall | N/A | Physicians requesting additional tests in the absence of indications or else avoiding high-risk patient groups in which adverse outcomes may occur during diagnosis and treatment |
| 48 | Ionescu | 2019 | Romania | Obstetrician/gynecologists | 73 | Overall | Working experience | A cesarean delivery recommended by the doctor in the absence of any clear medical indication that such a delivery method is needed to avoid possible litigation or a possible accusation of malpractice (defensive cesarean section) |
| 49 | Renkema | 2019 | Netherlands | Multiple specialties | 214 | Subitems | Age, specialty, technical title, attitude toward justified/unjustified litigation, and perceived patient pressure | The ordering of extra tests or procedures (assurance behavior) or the avoidance of high-risk patients or procedures (avoidance behavior), primarily to reduce the risk of being held liable for malpractice |
| 50 | Qiao | 2019 | China | Multiple specialties | 226 | Overall | N/A | Prescribe procedures or diagnostic tests or drugs that are clinically unnecessary to avoid possible troubles (such as lawsuits and disputes) |
| 51 | Garg | 2020 | India | Neurosurgeons | 214 | Subitems | Working experience and practice type | Clinical and operative practices to prevent medicolegal issues |
| 52 | Borgan | 2020 | USA | Internal medicine residents | 49 | Subitems | N/A | The deviation from routine medical care in order to avoid or reduce the risk of real or perceived future legal consequences |
| 53 | Calikoglu | 2020 | Turkey | Surgeons | 190 | Overall | Gender, academic occupation, specialty, and previous personal experience of medical-legal litigation | Medical behaviors that avoid physician liability without providing increased benefits to the patient |
| 54 | Gadjradj | 2020 | Cross-nation | Neurosurgeons | 490 | Subitems | N/A | Perform unnecessary, additional therapeutic or diagnostic interventions that do not improve the medical condition of the patient (positive defensive medicine), or it may cause physicians to refer or refuse difficult cases (negative defensive medicine) |
| 55 | Abbass | 2021 | Egypt | Multiple specialties | 261 | Subitems | Gender and specialty | The overuse of the resources such as ordering unnecessary investigations, giving treatment, or performing procedures aiming at doctors’ self-protection against claims rather than for the patient best interest |
| 56 | Fineschi | 2021 | Italy | Obstetrician/gynecologists | 168 | Subitems | N/A | The practice of recommending a diagnostic test or medical treatment (positive defensive medicine) or avoidance of risky patients or procedures (negative defensive medicine) that serves the function to protect physicians against patients’ claims |
| 57 | Kolcu | 2021 | Turkey | General practitioners | 196 | Subitems | N/A | The cost-increasing, defensive, or avoidance behavior displayed by physicians in healthcare delivery in order to protect themselves from legal problems |
| 58 | Perea-Pérez | 2021 | Spain | Emergency physicians | 1449 | Subitems | N/A | The making of clinical decisions that, while being explainable, prioritize the doctor’s legal security over other healthcare considerations |
| 59 | Rudey | 2021 | Brazil | Obstetrician/gynecologists | 403 | Overall | Gender, working experience, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | A practice wherein a healthcare professional makes decisions out of fear of litigation and not for the benefit of the patients |
| 60 | Ekici | 2021 | Turkey | Oral and maxillofacial surgeons | 109 | Subitems | N/A | A medical behavior that avoids medical responsibility without offering the patient greater benefits |
| 61 | Tumelty | 2021 | Ireland | Surgeons | 157 | Subitems | N/A | Behaviors engaged in by physicians for the purposes of averting the threat of medical negligence litigation and/or complaints |
| 62 | Zaed | 2021 | Italy | Neurosurgeons | 64 | Subitems | N/A | The practice of prescribing unnecessary medical care to minimize litigation exposure (positive defensive medicine) or the practice of avoiding more risky, albeit important, treatment measures to avoid litigation exposure (negative defensive medicine) |
| 63 | Vizcaino-Rakosnik | 2022 | Spain | Unclear | 282 | Overall | N/A | Made changes in their clinical practice because of the experience of being claimed |
| 64 | Shehata | 2022 | Egypt | Anesthesiologists | 177 | Subitems | Age, gender, marital status, technical title, professional certification, practice location, and type of employment (contract or permanent) | Defensive medicine occurs when doctors order tests, procedures, or visits or avoid high-risk patients or procedures, primarily (but not necessarily or solely) to reduce their exposure to malpractice liability |
| No . | First author . | Publication year . | Location . | Specialty . | Sample size . | Outcome dimension . | Influencing factorsh . | Definition of defensive medicine . |
|---|---|---|---|---|---|---|---|---|
| 1 | Summerton | 2000 | UK | General practitioners | 339 | Subitems | N/A | Ordering of treatments, tests, and procedures for the purpose of protecting the doctor from criticism rather than diagnosing or treating the patient |
| 2 | Symon | 2000 | UK | Midwives and obstetrician | 211 | Overall | N/A | Personally changed practice as a result of the fear of litigation |
| 3 | Passmore | 2002 | UK | Psychiatrists | 95 | Overall | N/A | Ordering of treatments, tests, and procedures for the purpose of protecting the doctor from criticism rather than diagnosing or treating the patient |
| 4 | Toker | 2004 | Israel | Ear, nose, and throat physicians | 194 | Subitems | N/A | A physician’s deviation from what is considered to be good practice to prevent complaints from patients or their families |
| 5 | Studdert | 2005 | USA | Multiple specialtiesa | 824 | Subitems | Gender, insurance coverage, premium burden, experience of being dropped by insurer practice type, and working experience | Physicians alter their clinical behavior because of the threat of malpractice liability |
| 6 | Sánchez-González | 2005 | Mexico | Unclear | 613 | Overall | N/A | Application of treatments, tests, and procedures with the explicit main purpose of defending the doctor from criticism, having documentary evidence in the event of a lawsuit and avoiding controversies, over and above the diagnosis or treatment of the patient |
| 7 | Hiyama | 2006 | Japan | Gastroenterologists | 131 | Overall | Working experience and practice type | A deviation from sound medical practice that is induced primarily by the threat of liability claims |
| 8 | Krawitz | 2006 | New Zealand | Clinician | 26 | Overall | Public and mass media attention, Ministry of Health, requests by superiors to practice defensive medicine, and politicians and policy | Taken a treatment approach not likely to be in the client’s best interest but protects from medicolegal repercussions |
| 9 | Mullen | 2008 | New Zealand | Psychiatrists | 86 | Subitems | N/A | Additional effort, of marginal clinical utility, is made to avoid complaint or legal liability |
| 10 | Catino | 2009 | Italy | General practitioners | 307 | Overall | Fear of a request for compensation, fear of medical-legal litigation, fear of disciplinary sanctions, fear of negative publicity, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | Healthcare personnel order unnecessary treatments (positive defensive medicine) or avoid high-risk procedures or patients (negative defensive medicine) with the principle—though not exclusive—aim of reducing their exposure to damages claims |
| 11 | Catino | 2009 | Italy | General practitioners, anesthetists, and surgeons | 102 | Overall | Age, fear of a request for compensation, fear of medical-legal litigation, fear of disciplinary sanctions, fear of negative publicity, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | Healthcare personnel effect unnecessary treatments or avoid high-risk procedures, with the principle—though not exclusive—aim of reducing their exposure to malpractice litigation |
| 12 | Bishop | 2010 | USA | Multiple specialtiesb | 1231 | Overall | Gender, practice location (rural or urban), practice type, source of income, and hour-long patient care | Physicians order more tests and procedures than patients need to protect themselves from malpractice suits |
| 13 | Nash | 2010 | Australia | Multiple specialtiesb | 2999 | Subitems | Previous personal experience of medical-legal litigation | Perceived change in practice behavior due to concerns about medicolegal negligence claims and complaints |
| 14 | Anderson | 2011 | USA | Obstetrician/gynecologists | 241 | Subitems | Age, career satisfaction, previous personal experience of medical-legal litigation, insurance premium evolution, and malpractice crisis level of the region | Changes in practices due to malpractice concern |
| 15 | Leary | 2011 | USA | Residents (surgical versus medical) | 76 | Overall | N/A | A deviation from sound medical practice that physicians engage in primarily because they perceive a threat of liability |
| 16 | Asher | 2012 | Israel | Multiple specialtiesc | 877 | Overall | Age, gender, specialty, previous personal experience of medical-legal litigation, exposure to complaint, practice type, managerial job, career satisfaction, and owning private malpractice insurance | Ordering of tests, procedures, and visits or the avoidance of high-risk patients or procedures, primarily to reduce exposure to malpractice liability |
| 17 | Nahed | 2012 | USA | Neurosurgeons | 1028 | Subitems | N/A | Perception changes actions solely to mitigate liability risk |
| 18 | Manish | 2012 | USA | Plastic and aesthetic surgeons | 1214 | Subitems | N/A | Medical practices that may exonerate physicians from liability without significant benefit to patients |
| 19 | Asher | 2013 | Israel | Obstetrician/gynecologists | 117 | Subitems | Age, gender, concern over potential medicolegal litigation, practice location (rural or urban), and professional status | Medical actions, performed mainly in order to refrain from being sued rather than actually aiding the patient |
| 20 | Ortashi | 2013 | UK | Unclear | 204 | Overall | Age, gender, technical title, and specialty | A doctor’s deviation from their usual behavior or that considered good practice, to reduce or prevent complaints or criticism by patients or their families |
| 21 | Prieto-Miranda | 2013 | Mexico | Multiple specialtiesd | 246 | Overall | Age, gender, work shifts, specialty, professional certification, working experience, and previous personal experience of medical-legal litigation | Aapplication of treatments, performance of diagnostic tests and therapeutic procedures, more than with the objective of diagnosing and adequately treating the patient, with the main purpose of defending the doctor from criticism, in addition to having documentary evidence in the event of a lawsuit and avoiding controversies |
| 22 | Jingwei | 2014 | China | Unclear | 504 | Overall | Gender, working experience, education, specialty, technical title, monthly payroll income, workload, type of hospital, and exposure to medical dispute | Medical practice based on fear of legal liability rather than on patients’ best interests |
| 23 | Moosazadeh | 2014 | Iran | General practitioners | 423 | Subitems | Age, gender, working experience, insurance coverage, and previous experience of a colleague being subject to medical-legal litigation | Every therapeutic test or method, whose primary aim is to protect the physician against the threat of being accused of making a forensic medicine mistake or of being sued for medical mistakes |
| 24 | Roytowski | 2014 | South Africa | Neurosurgeons | 66 | Subitems | N/A | Changing practice behavior to try to minimize the risk of a lawsuit |
| 25 | Solaroglu | 2014 | Turkey | Neurosurgeons | 404 | Overall | Gender, working experience, types of hospital, and the geographic regions | Medical practices that help doctors avoid liability without providing any additional benefit to the patient |
| 26 | Bourne | 2015 | UK | Multiple specialties | 7926 | Subitems | Exposure to complaint, length of investigation, outcome of investigation, complaint source, and type of complaint | Broadly categorized into ‘hedging’ and ‘avoidance’. Hedging is when doctors are overcautious, leading to overprescribing, referring too many patients or over investigation. Avoidance includes not taking on complicated patients and avoiding certain procedures or more difficult cases |
| 27 | Motta | 2015 | Italy | Otolaryngology | 100 | Overall | Concern over potential medicolegal disputes, concern over variations in the doctor/patient relationship, and knowledge of insurance clauses | Defensive medicine is defined as the ordering of tests and procedures (positive defensive medicine) or the avoidance of high-risk patients or procedures (negative defensive medicine), primarily to reduce exposure to malpractice liability |
| 28 | Osti | 2015 | Austria | Multiple specialtiese | 193 | Overall | N/A | Medical practices that may exonerate doctors from liability without significant benefit to patients |
| 29 | Reisch | 2015 | USA | Breast pathologists | 252 | Overall | Age, gender, geographic region, medical skills training, previous personal experience of medical-legal litigation, working experience, workloads, and exposure to medical malpractice | A deviation from standard medical practice induced primarily by a threat of liability |
| 30 | Smith | 2015 | USA | Neurosurgeons | 1026 | Overall | Working experience, reimbursement patterns, claims history, insurance coverage and cost, malpractice crisis level of the region, and patients with public insurance | An incentive to administer precautionary treatment with minimal expected medical benefit out of fear of litigation |
| 31 | Tanriverdi | 2015 | Turkey | Medical oncologists | 124 | Overall | Age, gender, academic occupation, working experience, type of hospital, and occupational status | Occasionally indulging unnecessary treatment requests to defend against lawsuits for medical errors and the use of unapproved medical applications |
| 32 | Abdel | 2016 | Sudan | Obstetrician/gynecologists | 117 | Overall | Working experience, professional certification, technical title, and type of hospital | A doctor’s deviation from the usual practice in order to reduce or prevent criticism and/or complaints by patients or their relatives |
| 33 | Panella | 2016 | Italy | Multiple specialties | 1313 | Overall | Age, gender, specialty, working experience, workload, and perception of being a ‘second victim’i | A deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims |
| 34 | Silberstein | 2016 | Israel | Plastic and aesthetic surgeons | 78 | Overall | Gender, working experience, managerial job, exposure to medicolegal literature, and requests by superiors to practice defensive medicine | Medical practices carried out primarily to avoid malpractice liability rather than to benefit the patient |
| 35 | Smith | 2016 | Canada | Neurosurgeons | 75 | Subitems | N/A | A deviation from regular medical practice because of medicolegal fears |
| 36 | Yan | 2016 | Cross-nationf | Neurosurgeons | 1142 | Overall | N/A | The practice of prescribing unnecessary medical care or avoiding high-risk situations out of fear of litigation |
| 37 | Din | 2017 | USA | Spine neurosurgery | 1024 | Overall | Malpractice crisis level of the region, premium burden, patients with public insurance, and exposure to malpractice claims | The provision of services beyond what is needed to improve patient outcomes (assurance behavior) and the evasion of high-risk procedures (avoidance behavior) to either deter litigation or substantiate clinical decision-making in the court |
| 38 | Olcay | 2017 | Turkey | Cardiologists | 253 | Overall | Previous personal experience of medical-legal litigation | Establishing diagnoses that would not alter patient care and performing unnecessary testing and treatments |
| 39 | Panella | 2017 | Italy | Multiple specialties | 1313 | Overall | Exposure to malpractice claims, fear of medical-legal litigation, fear of a request for compensation, fear of negative publicity, ineffective physician–patient relationship, insurance coverage, hospital support for liability issues, and public and mass media attention | A deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims |
| 40 | Ramírez-Alcántara | 2017 | Turkey | General practitioners | 87 | Overall | Work shifts | Application of treatments, performance of diagnostic tests and therapeutic procedures, more than with the aim of properly diagnosing and treating the patient, with the main purpose of defending the doctor from criticism, in addition to having documentary evidence in the event of a lawsuit and avoiding controversies |
| 41 | Reuveni | 2017 | Israel | Psychiatrists | 213 | Subitems | N/A | Medical actions that deviate from sound medical practice, performed primarily to reduce exposure to malpractice liability or to provide legal protection in the case of a malpractice lawsuit |
| 42 | Vandersteegen | 2017 | Belgium | Multiple specialties | 508 | Overall | Age, gender, region, working experience, insurance premium evolution, incitement by fund for medical accidents, consequences of medical lawsuit, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | The avoidance of certain high-risk procedures or patients or the ordering of procedures, tests, or visits, primarily (but not solely) due to the threat of medical liability |
| 43 | Yan | 2017 | Netherlands | Neurosurgeons | 45 | Subitems | N/A | A departure from standard medical practices out of fear of litigation |
| 44 | Tebano | 2018 | Cross-nationg | Antibiotic stewards | 830 | Subitems | Specialty, geographic regions, age, type of employment (contract or permanent), and fear of medical-legal litigation | When physicians perceive litigation as a threat, they may adopt defensive behaviors as a way to reduce the chances of litigation or to ensure a form of defense in the case of malpractice claims |
| 45 | Titus | 2018 | USA | Melanoma pathologists | 207 | Subitems | N/A | Behaviors that are intended to reduce exposure to malpractice litigation but may not clinically benefit the patient |
| 46 | Zhu | 2018 | China | Obstetrician/gynecologists | 1486 | Overall | Gender, level of hospital, education, specialty, exposure to medical dispute, previous personal experience of medical-legal litigation, consequences of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | The alterations of modes of medical practice, induced by the threat of liability, for the principal purposes of forestalling lawsuits by patients as well as providing good legal defense in the event that such lawsuits are instituted |
| 47 | Delice | 2019 | Turkey | Emergency medical specialists | 321 | Overall | N/A | Physicians requesting additional tests in the absence of indications or else avoiding high-risk patient groups in which adverse outcomes may occur during diagnosis and treatment |
| 48 | Ionescu | 2019 | Romania | Obstetrician/gynecologists | 73 | Overall | Working experience | A cesarean delivery recommended by the doctor in the absence of any clear medical indication that such a delivery method is needed to avoid possible litigation or a possible accusation of malpractice (defensive cesarean section) |
| 49 | Renkema | 2019 | Netherlands | Multiple specialties | 214 | Subitems | Age, specialty, technical title, attitude toward justified/unjustified litigation, and perceived patient pressure | The ordering of extra tests or procedures (assurance behavior) or the avoidance of high-risk patients or procedures (avoidance behavior), primarily to reduce the risk of being held liable for malpractice |
| 50 | Qiao | 2019 | China | Multiple specialties | 226 | Overall | N/A | Prescribe procedures or diagnostic tests or drugs that are clinically unnecessary to avoid possible troubles (such as lawsuits and disputes) |
| 51 | Garg | 2020 | India | Neurosurgeons | 214 | Subitems | Working experience and practice type | Clinical and operative practices to prevent medicolegal issues |
| 52 | Borgan | 2020 | USA | Internal medicine residents | 49 | Subitems | N/A | The deviation from routine medical care in order to avoid or reduce the risk of real or perceived future legal consequences |
| 53 | Calikoglu | 2020 | Turkey | Surgeons | 190 | Overall | Gender, academic occupation, specialty, and previous personal experience of medical-legal litigation | Medical behaviors that avoid physician liability without providing increased benefits to the patient |
| 54 | Gadjradj | 2020 | Cross-nation | Neurosurgeons | 490 | Subitems | N/A | Perform unnecessary, additional therapeutic or diagnostic interventions that do not improve the medical condition of the patient (positive defensive medicine), or it may cause physicians to refer or refuse difficult cases (negative defensive medicine) |
| 55 | Abbass | 2021 | Egypt | Multiple specialties | 261 | Subitems | Gender and specialty | The overuse of the resources such as ordering unnecessary investigations, giving treatment, or performing procedures aiming at doctors’ self-protection against claims rather than for the patient best interest |
| 56 | Fineschi | 2021 | Italy | Obstetrician/gynecologists | 168 | Subitems | N/A | The practice of recommending a diagnostic test or medical treatment (positive defensive medicine) or avoidance of risky patients or procedures (negative defensive medicine) that serves the function to protect physicians against patients’ claims |
| 57 | Kolcu | 2021 | Turkey | General practitioners | 196 | Subitems | N/A | The cost-increasing, defensive, or avoidance behavior displayed by physicians in healthcare delivery in order to protect themselves from legal problems |
| 58 | Perea-Pérez | 2021 | Spain | Emergency physicians | 1449 | Subitems | N/A | The making of clinical decisions that, while being explainable, prioritize the doctor’s legal security over other healthcare considerations |
| 59 | Rudey | 2021 | Brazil | Obstetrician/gynecologists | 403 | Overall | Gender, working experience, previous personal experience of medical-legal litigation, and previous experience of a colleague being subject to medical-legal litigation | A practice wherein a healthcare professional makes decisions out of fear of litigation and not for the benefit of the patients |
| 60 | Ekici | 2021 | Turkey | Oral and maxillofacial surgeons | 109 | Subitems | N/A | A medical behavior that avoids medical responsibility without offering the patient greater benefits |
| 61 | Tumelty | 2021 | Ireland | Surgeons | 157 | Subitems | N/A | Behaviors engaged in by physicians for the purposes of averting the threat of medical negligence litigation and/or complaints |
| 62 | Zaed | 2021 | Italy | Neurosurgeons | 64 | Subitems | N/A | The practice of prescribing unnecessary medical care to minimize litigation exposure (positive defensive medicine) or the practice of avoiding more risky, albeit important, treatment measures to avoid litigation exposure (negative defensive medicine) |
| 63 | Vizcaino-Rakosnik | 2022 | Spain | Unclear | 282 | Overall | N/A | Made changes in their clinical practice because of the experience of being claimed |
| 64 | Shehata | 2022 | Egypt | Anesthesiologists | 177 | Subitems | Age, gender, marital status, technical title, professional certification, practice location, and type of employment (contract or permanent) | Defensive medicine occurs when doctors order tests, procedures, or visits or avoid high-risk patients or procedures, primarily (but not necessarily or solely) to reduce their exposure to malpractice liability |
General surgeons, radiologists, emergency physicians, orthopedic surgeons, obstetrician/gynecologists, and neurosurgeons.
Primary care, surgical specialists, nonsurgical specialists, and other specialists.
Obstetricians, gynecologists, physicians, surgeons, anesthetists, psychiatrists, pathologists, radiologists, pediatricians, accident, and emergency specialists.
Pediatricians, internists, obstetricians and gynecologists, orthopedic surgeons, family medicine practitioners, general surgeons, cardiologists, and neurosurgeons.
Orthopaedic surgeons, trauma surgeons, and radiologists.
USA, Canada, and South Africa.
Including 74 countries.
N/A: not applicable.
Second victim: a healthcare provider involved in an unanticipated adverse patient event, medical error, and/or a patient related injury, who becomes victimized in the sense that the provider is traumatized by the event.
Quality assessment
The quality of the included studies was assessed using the Joanna Briggs Institute Critical Appraisal Checklist for Studies Reporting Prevalence Data, updated in June 2022 [17, 18]. Two investigators independently assessed study quality, and any disagreements were resolved by consensus.
Data synthesis and analysis
The main outcomes of this review were the prevalence and determinants of defensive medicine among physicians. In the included studies, the pooled prevalence of overall defensive medicine and its subitems was calculated with a 95% confidence interval (CI). For studies that did not report the overall prevalence of defensive medicine, we used the subitem with the highest prevalence rate as a proxy for the total to obtain a conservative estimate. Considering the expected heterogeneity among the included studies owing to variations in geographical location, population, specialty, and culture, we utilized a random-effects model. Subgroup analyses were also performed to compare the pooled prevalence of defensive medicine between studies conducted in different regions of the world and among physicians from different specialties.
We further performed a meta-analysis of the determinants of defensive medicine among physicians, including only factors examined in at least two studies. In the meta-analyses, the pooled odds ratios (ORs) and 95% CIs were reported to assess the effect of the factors, and forest plots were used to visualize the variability among studies. Finally, funnel diagrams and Egger’s tests were used to assess the publication bias in the studies included in the meta-analysis. A significance level of 5% was used for this review. All analyses were performed using Stata 16.0 and the R project.
Results
Search results and included studies
Search results
A systematic literature search initially yielded 8892 records, from which 64 eligible studies were included in review. The PRISMA diagram of the systematic search is shown in Fig. 1, and references for the studies included in this review are presented in Supplemental File 2.
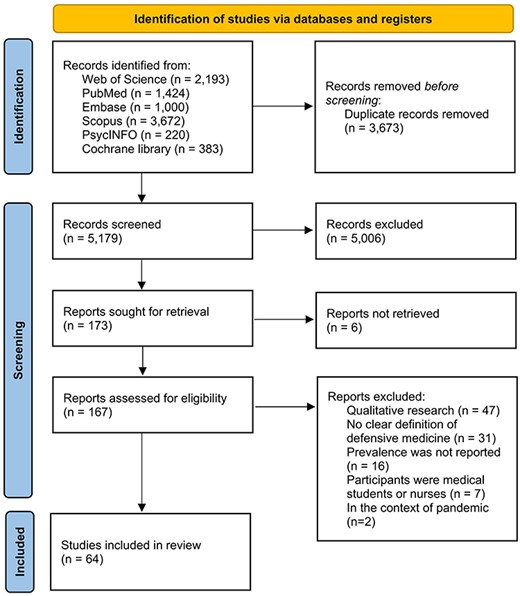
Characteristics of the studies included
Through a full-text review, we extracted contextual details from the included studies (Table 1). The results revealed that all 64 studies encompassing over 23 countries and scrutinizing more than 35 900 physicians reported the overall prevalence of defensive medicine and/or its subitems. Among these studies, 20 were conducted in the European region, which ranked first. The prevalence of defensive medicine across different specialties was also explored, with surgeons receiving the most attention (n = 24). All included studies utilized a cross-sectional design. Moreover, 37 studies discussed the determinants of defensive medicine among physicians. All included studies were rated as having acceptable quality according to the quality assessment, as shown in Supplemental File 3.
Definition and measurement of defensive medicine in the studies included
Based on a comprehensive review of the definitions of defensive medicine in the included studies (listed in Table 1), three fundamental elements of the concept were observed: (i) purpose—aiming to avoid being subject to lawsuits, criticisms, or disputes; (2) process—the alteration of medical practice; and (3) result—a deviation from patient-centered care and the best interest of the patient. Out of the 64 included studies, 16 studies employed a binary categorization to assess defensive medicine, where ‘no’ signified the absence of defensive medical behavior. Meanwhile, 33 studies employed multi-dimensional Likert scales, encompassing terms with negative connotations like ‘never’ and ‘rarely’ to indicate the absence of defensive medical behavior. Additionally, 15 studies evaluated defensive medicine by asking respondents to specify the frequency of such behavior, with only ‘none’ denoting the absence of defensive medical behavior.
Prevalence of defensive medicine among physicians
Prevalence of defensive medicine across regions
Our review examined the total prevalence of defensive medicine among physicians globally. The overall pooled prevalence of defensive medicine was 75.8% (95% CI: 72.3%, 79.3%), as shown in Supplemental File 4. Notably, the prevalence of defensive medicine varies considerably across countries, and the pooled prevalence in each country included in this review is listed in Supplemental File 5. To provide a comprehensive view of the data, we created a hierarchical map, illustrating the prevalence of defensive medicine in various countries (shown in Fig. 2).
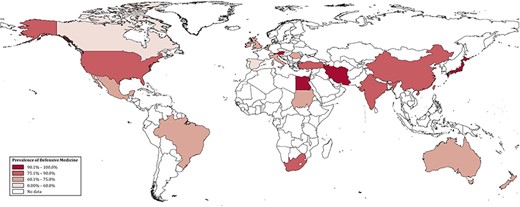
To further explore the regional differences in the prevalence of defensive medicine, we calculated regional estimates by grouping countries according to the six regions defined by the World Health Organization. Simultaneously, we categorized countries into different income groups based on the World Bank classification to assess the variance of defensive medicine across countries of different economic levels. The pooled prevalence of defensive medicine was relatively high in Africa (88.1%; 95% CI: 80.4%–95.8%), the Americas (80.8%; 95% CI: 76.8%–84.9%), and the Western Pacific region (76.1%; 95% CI: 64.0%–88.3%). Comparatively, the prevalence was lower in European (70.8%; 95% CI: 64.3%–77.2%) and Eastern Mediterranean regions (73.2%; 95% CI: 62.6%–83.8%). Notably, the lower-middle-income group (89.0%; 95% CI: 78.2%–99.8%) exhibited a higher prevalence than the upper-middle-income group (77.3%; 95% CI: 68.6%–85.9%) and high-income group (74.6%; 95% CI: 70.8%–78.5%), which is shown in Fig. 3.
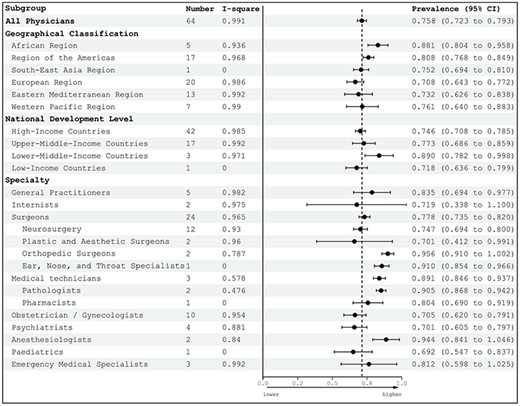
The subgroup analysis of the prevalence of defensive medicine by region and specialty.
Prevalence of defensive medicine by specialty
According to the subgroup analysis by specialty, the prevalence of defensive medicine varied markedly among different medical professionals. Specifically, anesthesiologists (94.4%; 95% CI: 84.1%–104.6%), medical technicians (89.1%; 95% CI: 84.6%–93.7%), general practitioners (83.5%; 95% CI: 69.4%–97.7%), and surgeons (77.8%; 95% CI: 73.5%–82.0%) exhibited a higher prevalence of defensive medicine than the overall pooled prevalence. In contrast, the prevalence rates of defensive medicine among internists, obstetricians/gynecologists, psychiatrists, and pediatrics were lower than the overall pooled prevalence, as shown in Fig. 3. It is worth noting that emergency medical specialists exhibited a slightly higher prevalence than the overall pooled prevalence.
Prevalence of defensive medicine subitems
The frequency of practicing the subitems of defensive medicine varied, as shown in Fig. 4. The subitem with the highest prevalence rate in the category of assurance behavior was increasing follow-up for defensive purposes, which was practiced by 79.8% of the physicians. Moreover, there were two other assurance behaviors with a prevalence of over 60%: consulting specialists (without transferring the primary responsibility of the patient’s care) more often than medically indicated (68.5%; 95% CI: 52.3%–84.7%) and ordering more tests or images than medically indicated (62.2%; 95% CI: 56.0%–68.3%). In contrast, the least frequently practiced assurance behavior was performing invasive procedures contrary to professional judgment (35.6%; 95% CI: 26.5%–44.7%). Furthermore, physicians also made unnecessary referrals (50.8%; 95% CI: 41.0%–60.5%) and prescribed more medications than medically indicated (46.2%; 95% CI: 34.6%–57.8%).

The most adopted avoidance behavior was avoidance of treatment protocols, with high-complication rates (72.3%; 95% CI: 61.6%–82.9%). Physicians also engaged in avoiding or eliminating certain procedures (44.5%; 95% CI: 31.6%–57.3%) and avoiding patients with specific conditions (45.5%; 95% CI: 37.3%–53.7%).
Determinants of defensive medicine among physicians
A typology of the determinants
Among the included studies, 38 studies investigated the determinants of defensive medicine using quantitative or mixed-methods approach. Detailed information on these determinants is presented in Supplemental File 6. They can be classified into individual, relational, organizational, and environmental levels.
Results of the meta-analyses for determinants of defensive medicine
Nine determinants discussed in 21 articles were used in the meta-analysis. At the individual level, physicians with more than 20 years of working experience (OR: 0.82; 95% CI: 0.55–1.09), being 50 years old or above (OR: 0.68; 95% CI: 0.33–1.03), and with a senior technical title (OR: 0.68; 95% CI: 0.44–0.93) were associated with less likelihood of practicing defensive medicine (Fig. 5). In addition, physicians in group practice had a lower likelihood of defensive medicine than those in solo practice (OR: 0.81; 95% CI: 0.59–1.04). At the relational level, the pooled results indicated that physicians having previous experience of medical-legal litigation (OR: 1.65; 95% CI: 1.13–2.18) or with colleagues having previous experience of medical-legal litigation (OR: 1.31; 95% CI: 1.00–1.61) were more likely to conduct defensive medicine. At the organizational level, physicians working in tertiary hospitals tended to have fewer defensive medical practices (OR: 0.57; 95% CI: 0.40, 0.74).
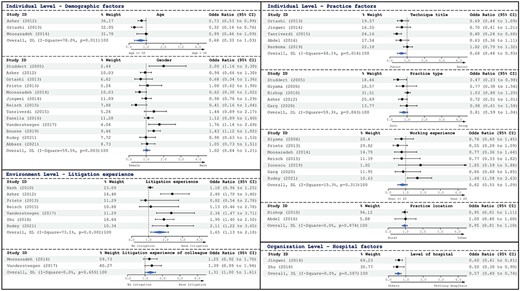
Notably, no environment-related determinants met the inclusion criteria for the meta-analysis. Among the studies analyzed, environment-related determinants were either unmeasured or reported inconsistently, precluding us from including them in the examination.
Publication bias
The results of our systematic review, as shown in Supplemental File 7, suggested minimal publication bias in the included studies, except for a slight bias in the working experience variable (Egger’s test P-value:.027). Nonetheless, the overall results remained robust and reliable, owing to the minimal publication bias observed in most studies. An evaluation of publication bias took into consideration the quality of the included studies. As detailed in Supplemental File 3, each study encompassed in this review has been assessed and deemed to meet acceptable quality standards.
Discussion
Statement of principal findings
This systematic review and meta-analysis revealed an overall pooled prevalence of 75.8% for defensive medicine use among physicians, underscoring the global severity of the issue. This has substantial implications for patient care, especially for addressing increased healthcare costs and potential harm to patients [4]. Disparities in the prevalence of defensive medicine were observed across countries, regions, and specialties. Additionally, factors at the individual, relational, organizational, and environmental levels can have an impact on defensive medicine.
Interpretation within the context of the wider literature
Defensive medicine was more prevalent in Africa, the Americas, and the Western Pacific than in European and the Eastern Mediterranean regions. The observed differences could be a result of the disparities in the cultural contexts in which healthcare settings are based (e.g. blame culture) [19]. We also found that the defensive medicine was more prevalent in low- and middle-income countries compared to high-income countries, which may be attributed to three factors. First, physicians in high-income countries are often required to participate in continuing medical education programs to maintain their licenses, equipping them with the most up-to-date knowledge of the best medical practices [20, 21]. Second, alternative dispute resolution methods, including communication and resolution programs in the USA [22] and Canada [23], as well as disclosure and apology laws [24], promote physician–patient communication, and avoid litigation [25]. Third, robust medical liability legal systems have been implemented, such as no-fault compensation systems in New Zealand [26], Denmark [27], and Finland [28]; tort reform in the USA [29]; and stronger systems of medical liability insurance [11, 12], which provide physicians with a sense of safety toward potential medical liability risks.
Variations in the prevalence of defensive medicine were observed across medical specialties, with anesthesiologists and medical technicians exhibiting the highest adoption rates. Notably, general practitioners ranked third in terms of defensive medicine prevalence, and as a result, more effective support is needed to empower gatekeepers to prevent or reduce the overuse of medical resources in primary healthcare units [30]. Defensive medicine in surgery received the most attention in the studies included in our review, especially in neurosurgery. These studies emphasize the importance of implementing interventions to mitigate defensive medical practices among physicians who perform high-risk procedures daily [15]. Our findings suggest that policy interventions should be tailored to the specific needs of different physician specialties [31]. For instance, the implementation of evidence-based guidelines that furnish obstetrician-gynecologists with a well-defined framework for labor and delivery has been recognized as a useful measure to reduce defensive medicine [14, 32]. For anesthesiologists and medical technicians, it is important to provide regular education and training on new technologies and equipment. Additionally, educating and training physicians on informed consent and shared decision-making could help reduce the probability of malpractice claims, particularly in psychiatry [33, 34].
The meta-analysis indicated that physicians with less experience, working in solo practice, or holding junior titles are more likely to engage in defensive medicine. Therefore, more attention should be paid to designing targeted interventions and support systems for these specific groups [35], like enhancing their medical technology proficiency, which could reduce their ordering additional laboratory tests or imaging, or making more non-essential referrals as a strategy to mitigate potential legal liabilities or risks [36, 37]. It is also important to acknowledge that, as mentioned in a few studies included, there can be a contrasting trend as well [7, 14]. Specifically, some experienced physicians could also become more cautious, leading to an increase in defensive medicine, especially in areas with high litigation rates. This highlighted the complexity of the relationship between work experience and defensive medicine. The findings also revealed that physicians with a history of medical-legal litigation or those who had witnessed colleagues facing such litigation were more likely to practice defensive medicine. Policymakers should design measures to reduce the fear of malpractice litigation among physicians. This can be achieved by enhancing communication between physicians and patients through patient-centered communication techniques [38]. Efforts should also be directed toward increasing transparency in medical decision-making [39] and implementing evidence-based clinical practice guidelines to reduce variability in medical decision-making [39, 40]. Additionally, interventions should be aimed at cultivating a supportive professional environment and encouraging a culture of open communication and learning from errors rather than focusing on blame and punishment [41]. At the organizational level, physicians employed in tertiary hospitals exhibited a lower level of defensive medicine. Accordingly, defensive medicine practice by physicians in clinics, primary and secondary hospitals should receive more attention.
We conducted a qualitative investigation of the environment-related determinants. The high prevalence of defensive medicine within the institutional environment may be attributed to the malpractice crisis level or medical-legal risk environment, premium burden, and coverage of medical liability insurance [19, 42]. Additionally, physicians in countries with complex legal systems and higher malpractice insurance premiums were more likely to practice defensive medicine. In countries with a high prevalence of defensive medicine, the legal system often requires high burden of proof from physicians, making it difficult for them to defend against malpractice claims [43, 44]. In contrast, countries with a lower prevalence, such as Spain, featured a legal system favoring physicians [45]. One feasible policy intervention is to introduce a medical liability system and tort reform [46], including measures such as capping noneconomic damages, streamlining the investigation and litigation processes for medical malpractice claims, and introducing alternative dispute resolution mechanisms such as arbitration or mediation [47, 48]. Tort reform has demonstrated effective reduction of defensive medicine in some states in the USA [49]. Blame culture in healthcare settings also contributes to the prevalence of defensive medicine. Public education campaigns addressing healthcare complexities and promoting realistic patient expectations regarding treatment outcomes may help reduce dissatisfaction and the likelihood of malpractice claims [13, 19]. Moreover, fostering responsible and accurate media coverage of medical malpractice issues could assist in shifting societal attitudes toward a more balanced perspective on litigation and compensation [3, 25].
Implications for policy, practice, and research
Interventions should be tailored to the characteristics of different physician specialties and region, addressing the underlying factors that contribute to defensive medicine. Various measures can be implemented, including enhancing physicians’ medical technology proficiency, improving communication between physicians and patients, reducing the fear of litigation, and establishing stronger medical liability insurance systems. Efforts should also be directed toward addressing the social factors that contribute to blame culture and promoting defensive medical practices. Future research should focus on devising and evaluating the efficacy of these interventions to reduce the use of defensive medicine and to enhance the quality of patient care.
Strengths and limitations
This is the first review to analyze the global prevalence and determinants of defensive medicine, highlighting the heterogeneity of prevalence and the effectiveness of measures. This review also had some limitations. First, the included studies used various measurement tools to assess defensive medicine, which may have affected the comparability of the results. Second, the subitem with the highest prevalence rate was used, which inevitably led to an underestimation of the actual prevalence rate. Finally, all included studies used self-reported measures of defensive medicine, which may contain reporting bias.
Conclusion
The high prevalence of defensive medicine among physicians imposes a significant burden on healthcare systems, with potentially negative consequences for both patients and practitioners. Additionally, the necessity for policy interventions was emphasized, particularly for physicians in specialties with high-risk procedures and litigious environments.
Acknowledgements
Not applicable.
Supplementary data
Supplementary data is available at INTQHC online.
Conflict of interest
No potential conflict of interest was reported by the authors.
Funding
This work was supported by the National Natural Science Foundation of China under Grant No. 72174118 and Shanghai Philosophy and Social Science Project under Grant No. 2021ESH002.
Author contributions
Junyao Zheng: Conceptualization; Data curation; Investigation; Software; Visualization; Writing - original draft; Writing - review & editing. Yongbo Lu: Data curation; Investigation; Visualization; Writing - original draft; Writing - review & editing. Wenjie Li: Data curation; Investigation; Validation. Bin Zhu: Data curation; Writing - review & editing. Fan Yang: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Software; Supervision; Writing - review & editing. Jie Shen: Supervision; Data curation; Writing - review & editing.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Ethics and other permissions
Not applicable.
References
Author notes
Handling Editor: Dr. Phillip Phan



