-
PDF
- Split View
-
Views
-
Cite
Cite
Jonathan I Mitchell, Ian D Graham, Wendy Nicklin, The unrecognized power of health services accreditation: more than external evaluation, International Journal for Quality in Health Care, Volume 32, Issue 7, August 2020, Pages 445–455, https://doi.org/10.1093/intqhc/mzaa063
Close - Share Icon Share
Abstract
While it is widely recognized that accreditation enables an organization to improve its performance and sustain a culture of quality, changing healthcare practices to align with evidence-informed guidelines (clinical and administrative) is a complex process that takes time. The true value of accreditation lies in its contribution to healthcare safety and quality as a means to prompt and support ‘knowledge to action’, a key value of accreditation that ‘has yet to be articulated’. Using the ‘knowledge to action’ cycle, a planned action framework, we illustrate that accreditation is a knowledge translation (KT) or implementation intervention that seeks to improve and increase the uptake of evidence in healthcare organizations. The accreditation components, including the quality framework, standards, self-assessment process and on-site survey visit, ultimately serve to improve quality, decreasing variation in practice and strengthening a culture of quality. With a unique perspective and alignment obtained through the implementation lens, we examine the accreditation process and components relative to the ‘knowledge to action cycle’ with implications for enhancing the value of accreditation beyond current appreciation to both accreditation bodies worldwide and those organizations that participate in accreditation programs. Until organizations and accreditation bodies embrace the accreditation process as a knowledge to action intervention to bring about meaningful and sustained change, the full benefits of the process will not be optimized nor achieved.
More Than External Evaluation
Worldwide, health services accreditation is typically viewed as an external third-party peer review to assess and improve the quality of healthcare and to identify the achievement of standards [1, 2]. The underlying premise is that organizations aspire to meet or exceed the evaluation criteria (the standards) to obtain the accrediting body’s recognition and endorsement. The documented benefits of accreditation are many and include enabling the establishment of organizational structures and processes, promotion of quality and safety cultures and improvements in patient care [1]. Organizational benefits in terms of effectiveness, efficiency and integration of health services, as well as innovation, supports for evidence-based decision-making and increased stakeholder engagement, have also been linked to accreditation [3, 4]. However, internal and external contextual factors as well as organizational buy-in have been shown to influence an organization’s experience of accreditation [5]. The true value of accreditation results when it is reframed from an ‘externally’ imposed add-on project to a critical tool to complement and strengthen the organization’s quality improvement process, effectively enabling knowledge translation—KT (KT is defined as a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically sound application of knowledge to improve the health of a population, provide more effective health services and products and strengthen the healthcare system [7].). KT is about reducing the know-do gap by facilitating the use of evidence-informed practice and policy. Using the KT literature, we show that the optimal impact and value of the accreditation methodology is achieved when it is fully recognized as an ongoing capacity building tool and as a quality improvement and patient safety evaluation tool [1].
The Knowledge to Action Cycle
The knowledge to action cycle is a framework developed from a synthesis of 30 planned action models that highlights the key knowledge creation and action phases to activate or mobilize the use of knowledge or evidence. The ‘knowledge to action cycle’ [6] has been widely used and cited [7–9]. It comprises two major components: knowledge creation and the knowledge action or application cycle as shown in Fig. 1 [6]. We have adapted the labels in Fig. 1 to align with the accreditation context.
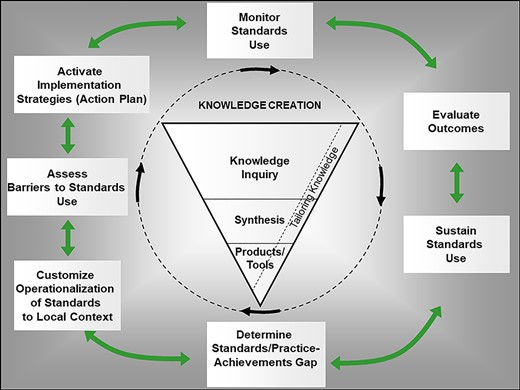
The knowledge to action cycle adapted to the accreditation process. Source: Adapted from Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N.J. Lost in knowledge translation: time for a map? Contin Educ Health Prof. 2006; 26(1):13–24.
The knowledge creation component draws attention to the refinement of the knowledge and the evidence to be implemented, for example, in the accreditation standards. The action cycle comprises seven action phases needed to implement knowledge in healthcare settings. These seven action phases involve the identification of the standards/practice–achievement gap; interpreting the standards within the local context (i.e. customization of the operationalization of the standards); assessing barriers and facilitators to the application of the standards; selecting, tailoring and activating implementation strategies to promote use of the standards; monitoring use of the standards; evaluating outcomes or impact from using the standards; and sustaining use of the standards. Given that the theory and evidence suggest that attending to these phases increases the likelihood of bringing about successful uptake of evidence [6–9], can this optimize organizations’ motivation and ability to engage with these action phases within accreditation?
In What Ways Is Accreditation KT?
The International Society for Quality in Health Care undertook an extensive process to clarify the different terms used with reference to external evaluation, including a comparison of the distinguishing features of accreditation, certification, regulation and licensing [10]. National health services accreditation programs feature comprehensive standards, a survey plan, a thorough self-assessment and on-site survey process (both of which should involve staff throughout the organization) and provision of a detailed accreditation report identifying strengths and opportunities for improvement. An ongoing relationship between the accreditation body (i.e. the accreditation organization) and the client organization (i.e. the health organization being accredited by the accreditation body) is generally sustained over the course of the accreditation cycle.
Appendix 1 maps generic components, processes and outputs of accreditation with the ‘knowledge to action cycle’ [6]. Specifically, the knowledge creation funnel of the ‘knowledge to action cycle’ represents the accreditation program synthesized knowledge to be implemented (the standards) as well as knowledge products and tools to facilitate the implementation of the standards. It can also represent the local knowledge or evidence that client organizations create to support and guide their accreditation and implementation efforts. The phases of the ‘knowledge to action cycle’s’ outer circle largely represent the activities that most accreditation processes intend to encourage. Indeed, they are the activities that client organizations use to facilitate knowledge uptake as part of the accreditation program. For example, related to the KTA phase of determining the evidence standards/practice–achievement gaps, the corresponding accreditation activities would be the self-assessment process and the on-site survey. These processes determine where there may be less than optimal achievement of or adherence to best practice standards that the organization can then prioritize for action.
Accreditation is about quality improvement, enabling the healthcare organization (acute care through to home care) to improve its processes according to standards (best practice) with the ultimate goal of improving care and outcomes. Those reading and applying the standards acquire access to a wealth of knowledge that supports their practice to ‘keep pace’—an example of the ‘sustaining knowledge use’ phase of the ‘knowledge to action cycle’. The self-assessment complements the standards and provides real-time data—customized to the local context (customization phase)—identifying strengths, opportunities for improvement and readiness for change (barrier/facilitator assessment phase). Acting as a KT vehicle and knowledge broker, surveyors foster mutual learning and knowledge exchange; examples of knowledge creation (producing/co-producing local knowledge and customization phases) and sustaining standards use in the ‘knowledge to action cycle’. Learning from the on-site visits, surveyors take the knowledge back to their own accredited organizations, yet another form of KT. By refocusing on KT rather than purely meeting the required accreditation standards/criteria, we argue that the accreditation process is KT as it encourages client organizations to follow the action phases. See Appendix 2 for illustrative scenarios from two different accreditation bodies (Canada and Australia) regarding how elements of their programs align with the KTA framework.
By actively engaging the entire organization in a culture of improvement through participation in a quality improvement action plan that includes the accreditation process, enhanced levels of quality can result (outcome and sustainability phases). However, accreditation is not the only quality improvement tool an organization will use. Every organization should have a quality improvement plan of which accreditation is one complementary component. Sustaining a culture of quality improvement is facilitated in part by promoting the principles of accreditation and quality improvement in each of the organization’s daily activities. In the ‘knowledge to action cycle’, this is operationalized as ‘sustain standards use’.
Embracing Accreditation as a KT Intervention to Improve Care Delivery and Outcomes
How can external evaluation be made more relevant for the challenges facing society and healthcare into the future [11] and, in particular, contribute to improving quality and outcomes? Conceptualizing accreditation within a KT framework must become a critical consideration as accrediting bodies are under increasing pressure to demonstrate relevance and value. For the CEOs of accreditation bodies, the resulting question becomes: must the accreditation product be changed to further enhance impact for sustaining culture change, quality improvement and other benefits? Indeed, one of the great challenges in healthcare is the effective, efficient and timely uptake of evidence-informed practices and policies which is the purpose of KT. From the time new knowledge is confirmed, putting this into practice has been elusive and generally a long-term effort (only to have newer evidence replace the older evidence quickly). Accreditation with renewed standards is a key enabler to this essential KTA process. While it may take 17 years to move evidence into practice, the half-life of knowledge in some areas is <5 years [12]. As accreditation bodies generally have a 4-year cycle to update standards, this enables those organizing and providing health services to continuously improve organizational quality and provision of care in a timely way, improving the quality of care offered as well as improving population health.
For this to occur, health services and professional accreditation programs will need to embrace the science of KT and implementation [13], review their processes and assess how they contribute to each of the KTA phases. They also need to consider how to further optimize their processes so as to facilitate and support client organizations to better engage with all the action phases of the KTA framework. Client organizations will also need to embrace KT and implementation science and better appreciate and understand how accreditation processes are specifically designed to support and encourage their KTA aspirations and goals. When conceptualizing and approaching the accreditation process as KT, there will be significantly greater potential for healthcare organizations to achieve a timely and powerful impact.
Acknowledgements
The authors thankfully acknowledge those who completed the scenario table (Appendix 2) on behalf of their organizations:
Accreditation Canada: Leslee Thompson, CEO; Patricia Sullivan-Taylor, Executive Lead—Policy and Partner Engagement.
AGPAL: Dr Stephen Clark, CEO of the AGPAL Group; Louise Kulper, National Manager of Quality Systems.
Ian D Graham is a recipient of a Canadian Institutes of Health Research Foundation Grant entitled, Moving knowledge into action for more effective practice, programs and policy: A research program focusing on integrated knowledge translation (FDN# 143237).
APPENDIX
| Mapping to ‘knowledge to action cycle’ . | Accreditation body program elements . | Description of client actions and rationale . |
|---|---|---|
| Knowledge/standards creation | ||
| ‘Knowledge/standards’ KT goal: to identify the knowledge to be implemented to optimize quality of care and patient safety. | Standards synthesize the best available evidence and expert opinion to offer guidance on how to enable quality improvement, mitigate safety risks and improve quality. These standards are reviewed regularly to ensure they are reflective of the current evidence. | The client organization implements or attempts to implement these standards on a regular basis, at minimum 1 year prior to the on-site survey visit. The currency and evidence-informed nature of the standards support the client organization in achieving their goal of keeping practices and decision-making current. |
| ‘Knowledge tools/products’ KT goal: to provide resources to facilitate meeting accreditation requirements and to encourage engagement with phases of the action cycle. | Specific assessment tools such as a staff engagement survey and/or a patient safety culture survey may be required which are utilized by the client organization on a cyclic basis. The results contribute toward identifying achievement of a particular standard criterion. These tools are often embedded in the accreditation body’s software that is made available to all client organizations. | The survey tools are of value to the client organization in that the results can be used, even in isolation from the standards assessment, to identify areas of strength or deficiency requiring an action plan. The tools could be reapplied at an appropriate interval to determine if change has occurred in the desired direction. |
| Action Phases | ||
| ‘Determine the standards/practice–achievement gap’ KT goal: to determine gaps between the standards and current practice–achievement so as to quantify the need for improvement. This information can be used to promote organizational consensus on the need to act to reduce the gap. | The accreditation body encourages the client organization to conduct a self-assessment against the standards. The purpose of this exercise is to enable identification of areas of strength and areas for improvement. The survey tools facilitate in identifying areas of strength and areas for improvement further strengthening the assessment of performance against a particular standard. The accreditation body organizes an on-site survey visit, conducted by surveyors carefully selected for their expertise and training, which is a vital component of their third-party external review process. The surveyors use different methodologies depending on the accreditation body’s program. At minimum it includes that surveyors visit the client organization in person to gather evidence of current practice which they can compare to the practice described in the standards. During the on-site visit, surveyors may interview the board, leadership, staff, patients, their families and key stakeholders in the community. The surveyors observe the environment, staff interactions and review documentation in the health record and policies. During discussion with individuals, the surveyors may provide feedback and evidence back to each team to encourage their practice going forward, reinforce those areas requiring improvement and share their own expertise. | The client organization conducts the self-assessment to determine the degree to which they achieve a particular standard and the specific criteria within the standard. This process enables their identification of performance relative to the standard and areas in which there are opportunities for improvement, as well as organizational readiness for change. The identified areas for improvement then become the focus of the client organization’s quality improvement action plan to address areas needing improvement. It is the decision of the client organization as to how the self-assessment process is conducted—whether an entire team collectively completes the assessment or whether a designated person does this on behalf of the team. Depending on the information technology resources of the client organization, the exercise may be conducted ‘online’ or manually on paper and then entered into the accreditation body’s software program. The survey instruments (e.g. staff engagement, patient safety culture) generally require involvement of staff, individually or as a team. In addition to providing useful results in identifying areas of strength and areas of improvement, the process contributes to team building. The client organization prepares for the on-site visit to ensure all necessary information is available for the surveyors, including availability of teams to be interviewed and preparation to enable observation of care/service being provided (e.g. surgery in the OR, a clinic as patients receive treatment). The recipients of care are available to speak with a surveyor when required while at all times maintaining anonymity and confidentiality to the degree necessary. Copies of health records are made available as appropriate. |
| ‘Customize operationalization of standards to local context’ KT goal: to adapt and customize the operationalization of the standard to foster organizational buy-in and contribute to optimal implementation of standards tailored to organizational needs. | While the standards are set and somewhat prescriptive, the accreditation body encourages the client organizations to review and develop an implementation strategy that is relevant to their own context. While standards outline a particular desired practice or result, the means by which this is achieved, the “how”, is the decision of the client organization. | The client organization has the responsibility to carefully assess each standard and determine how best to implement/achieve the standards within their own context. Every client organization’s structure, patient population, staffing arrangement and resource availability is different. There are unique elements in every client organization’s milieu. |
| ‘Assess barriers/facilitators to standards use’ KT goal: to identify potential barriers (and facilitators) to implementing the standards. This information can be used to more strategically to select implementation strategies explicitly targeting the barriers, thereby improving implementation success. | The self-assessment process enables the identification of the degree to which a standard is being achieved, identification of gaps or areas for improvement and in some cases identification of barriers to uptake of the particular standards. Furthermore, during the site visit, the surveyors may further identify barriers and offer suggestions for effective strategies for overcoming the identified barriers. These suggestions may be included in the final accreditation report. For example, a standard may require that a hand-washing procedure is in place, with evidence of its effectiveness. How that procedure is designed and implemented is the decision of the client organization. Throughout this design period and then assessment of its effectiveness after implementation, barriers and facilitators to the process are identified and adjustments made in order to obtain the optimum result for the client organization, their patients and staff. | Carefully reviewing each standard and then adapting the implementation to apply to their context are critical components from the beginning of the self-assessment process to the development of the quality improvement action plan. The client organization identifies those factors that are barriers and facilitators and indicates how they will be addressed in the action or implementation plan. Thus, if the standard requires an annual board evaluation, the type of tool utilized, the content, the means of administration, steps taken to analyze and actions taken to address the results lie with the client organization. Barriers to undertaking this exercise must be considered as well as those factors that will facilitate achieving this standard. Once the strategy is implemented, monitoring its effectiveness is important as is making corrections to the strategy as necessary to enable buy-in and achievement of the goal. |
| ‘Select, tailor and activate implementation strategies (the action plan)’ KT goal: to tailor implementation strategies to the identified barriers so as to increase implementation success. | The implementation strategy or quality improvement action plan that is developed by teams during the self-assessment process is the responsibility of the client organization—both to implement and monitor progress. Most accreditation bodies require that progress on this plan is provided back to them on a regular basis, e.g. every 6 months or annually. The accreditation report that is given to the organization post the on-site visit reinforces the actions that are required and assists in the determination of priorities for action. Other implementation strategies supported by accreditation bodies include providing education and training based on the learning needs of the client organization. Given the wealth of information that is obtained both online and during the on-site visit, many accreditation bodies are creating a ‘library’ of best or leading implementation practices that is accessible to all client organizations. The accreditation body develops eligibility criteria against which to assess if a strategy indeed qualifies as a best or leading practice (e.g. clinical, service, governance/leadership). | The quality improvement action plan is unique to each client organization and should ideally consider identified barriers to implementing the standards and identify how selected implementation strategies will address the barriers. There are many different implementation strategies to achieve uptake of a particular standard/criterion. Client organizations are encouraged to identify those strategies most relevant to them, optimizing buy-ins and results. Teams together develop these plans. The accreditation report is a useful tool for the client organization, confirming areas important to focus actions. Within the specified timeframes as to when reports should be provided to the accreditation body, the client organization’s implementation strategies are developed, monitored and assessed accordingly. The sharing of ‘leading or best practices’ between organizations is a major benefit for all client organizations. Rather than ‘reinventing the wheel’ to identify a strategy to meet a particular standard, reviewing what other client organizations have considered is very helpful. The client organization may then contact the ‘owner’ of that leading practice, seek advice and then consider and/or adapt that practice to their own setting, or choose to reject it. |
| ‘Monitor use of the standards’ KT goal: to determine the extent to which the organization is adhering to the standards so that the organization can assess its performance against the desired practice (the standard). The monitoring of indicators serves as a mechanism to ensure/facilitate that users’ knowledge and practice are ‘keeping pace’. | The standards may identify specific indicators that should be monitored to allow assessment of performance toward meeting the standards. Monitoring of strategic and operational indicators/performance measures occurs in all organizations. Utilizing the specific indicators that may be identified by the accreditation body provides further direction to confirm priority areas for monitoring. The accreditation bodies establish a mechanism with the client organizations to have regular contact throughout the accreditation cycle. Generally, following the receipt of the accreditation report, it is required that there be a 6-month report, an annual report or something similar. This ongoing monitoring of compliance and ongoing assessment of implementation of the action plan are critical components of the accreditation process. The goal is that accreditation is not a onetime event but an ongoing cycle, with an expectation of ongoing assessment of compliance with the standards, implementation of action plans, ongoing monitoring and continuing to improve care and services. At minimum, there is an expectation to receive a report, online or hard copy, at regular intervals of progress with the action plans. | The client organization has a responsibility to follow through on the implementation of the quality improvement action plan that results from the survey process. A sincere commitment by the organization to value this process is fundamental to its success and to having maximum impact on quality of care. Monitoring of strategic and operational indicators/performance measures occurs in all organizations. Utilizing specific indicators identified by the accreditation body provides further direction to confirm priority areas for monitoring and are used to determine adherence to the standards. The client organization recognizes that accreditation is a major quality improvement tool that complements other quality improvement strategies within their organization, e.g. LEAN, Six Sigma, etc. The client organization’s overall quality improvement plan at a strategic level acknowledges how these initiatives comprehensively integrate to enable improvement of care and services, from the governance level to the point of care. |
| ‘Evaluate outcome/impact’ KT goal: to determine the extent to which adherence to the standards translate into improved health outcomes or health system outcomes. This information can further motivate maintaining adherence to the standards and to celebrate organizational achievements. | As the primary goal of accreditation is to improve quality and safety, requirements to report on specific outcomes or specific clinical indicators may not be required by accreditation bodies. However, one of the key goals of accreditation is to provide an organization with tools that enable resilience. The content of the standards focuses on quality improvement and the prevention or mitigation of risk. If an adverse event arises, the organization knows how to learn from the event, recover and continue improving. Thus, accreditation does not guarantee quality of care but demonstrates accountability that the organization is focused on improvement and meeting evidence-based standards. | If outcomes of adherence to standards are collected, client organizations can use this information to justify implementing the standards, demonstrate to the community how they improve patient health outcomes and better demonstrate the value of money invested in healthcare. The challenge, however, is that the standard alone does not directly improve outcomes. Factors such as the knowledge and expertise of the ‘user’, patient behaviors and resource availability combine to enable the desired outcome. |
| ‘Sustain use of standards’ KT goal: to continue to focus the organization on maintaining adherence to the standard and maintaining quality and patient safety. If declines in adherence are observed, the organization can double efforts to identify barriers to ongoing use of the standards and institute more/different implementation strategies (starting the knowledge to action cycle over again). | If the accreditation body becomes concerned about the performance of the client organization, i.e. that insufficient attention is being paid to areas of concerns/deficiencies, or perhaps significant complaints from the public have been received by the accreditation body, mechanisms are in place to send a surveyor to the organization mid-cycle. Similar strategies can also be undertaken to identify problems and suggest improvements. This relationship is critical and an important part of the accreditation process. It provides support and assists with quality improvement and the implementation of recommendations. From one on-site visit to the next, the ongoing relationship with the client organization is sustained. Additional education and training are provided as appropriate to the client organization and its needs. Ongoing monitoring of performance is critical to sustaining standards use. | Client organizations are encouraged to use the standards in an ongoing way, perhaps to annually review the relevant standards. For example, the Emergency Department team should review the standards for emergency care annually, conduct a self-assessment and continuously monitor adherence to the standards. Are any new deficiencies identified? If the standard has been updated since previously utilized, there may be new important knowledge/practices to consider and be included in the quality improvement plan, including mechanisms to monitor progress. |
| Mapping to ‘knowledge to action cycle’ . | Accreditation body program elements . | Description of client actions and rationale . |
|---|---|---|
| Knowledge/standards creation | ||
| ‘Knowledge/standards’ KT goal: to identify the knowledge to be implemented to optimize quality of care and patient safety. | Standards synthesize the best available evidence and expert opinion to offer guidance on how to enable quality improvement, mitigate safety risks and improve quality. These standards are reviewed regularly to ensure they are reflective of the current evidence. | The client organization implements or attempts to implement these standards on a regular basis, at minimum 1 year prior to the on-site survey visit. The currency and evidence-informed nature of the standards support the client organization in achieving their goal of keeping practices and decision-making current. |
| ‘Knowledge tools/products’ KT goal: to provide resources to facilitate meeting accreditation requirements and to encourage engagement with phases of the action cycle. | Specific assessment tools such as a staff engagement survey and/or a patient safety culture survey may be required which are utilized by the client organization on a cyclic basis. The results contribute toward identifying achievement of a particular standard criterion. These tools are often embedded in the accreditation body’s software that is made available to all client organizations. | The survey tools are of value to the client organization in that the results can be used, even in isolation from the standards assessment, to identify areas of strength or deficiency requiring an action plan. The tools could be reapplied at an appropriate interval to determine if change has occurred in the desired direction. |
| Action Phases | ||
| ‘Determine the standards/practice–achievement gap’ KT goal: to determine gaps between the standards and current practice–achievement so as to quantify the need for improvement. This information can be used to promote organizational consensus on the need to act to reduce the gap. | The accreditation body encourages the client organization to conduct a self-assessment against the standards. The purpose of this exercise is to enable identification of areas of strength and areas for improvement. The survey tools facilitate in identifying areas of strength and areas for improvement further strengthening the assessment of performance against a particular standard. The accreditation body organizes an on-site survey visit, conducted by surveyors carefully selected for their expertise and training, which is a vital component of their third-party external review process. The surveyors use different methodologies depending on the accreditation body’s program. At minimum it includes that surveyors visit the client organization in person to gather evidence of current practice which they can compare to the practice described in the standards. During the on-site visit, surveyors may interview the board, leadership, staff, patients, their families and key stakeholders in the community. The surveyors observe the environment, staff interactions and review documentation in the health record and policies. During discussion with individuals, the surveyors may provide feedback and evidence back to each team to encourage their practice going forward, reinforce those areas requiring improvement and share their own expertise. | The client organization conducts the self-assessment to determine the degree to which they achieve a particular standard and the specific criteria within the standard. This process enables their identification of performance relative to the standard and areas in which there are opportunities for improvement, as well as organizational readiness for change. The identified areas for improvement then become the focus of the client organization’s quality improvement action plan to address areas needing improvement. It is the decision of the client organization as to how the self-assessment process is conducted—whether an entire team collectively completes the assessment or whether a designated person does this on behalf of the team. Depending on the information technology resources of the client organization, the exercise may be conducted ‘online’ or manually on paper and then entered into the accreditation body’s software program. The survey instruments (e.g. staff engagement, patient safety culture) generally require involvement of staff, individually or as a team. In addition to providing useful results in identifying areas of strength and areas of improvement, the process contributes to team building. The client organization prepares for the on-site visit to ensure all necessary information is available for the surveyors, including availability of teams to be interviewed and preparation to enable observation of care/service being provided (e.g. surgery in the OR, a clinic as patients receive treatment). The recipients of care are available to speak with a surveyor when required while at all times maintaining anonymity and confidentiality to the degree necessary. Copies of health records are made available as appropriate. |
| ‘Customize operationalization of standards to local context’ KT goal: to adapt and customize the operationalization of the standard to foster organizational buy-in and contribute to optimal implementation of standards tailored to organizational needs. | While the standards are set and somewhat prescriptive, the accreditation body encourages the client organizations to review and develop an implementation strategy that is relevant to their own context. While standards outline a particular desired practice or result, the means by which this is achieved, the “how”, is the decision of the client organization. | The client organization has the responsibility to carefully assess each standard and determine how best to implement/achieve the standards within their own context. Every client organization’s structure, patient population, staffing arrangement and resource availability is different. There are unique elements in every client organization’s milieu. |
| ‘Assess barriers/facilitators to standards use’ KT goal: to identify potential barriers (and facilitators) to implementing the standards. This information can be used to more strategically to select implementation strategies explicitly targeting the barriers, thereby improving implementation success. | The self-assessment process enables the identification of the degree to which a standard is being achieved, identification of gaps or areas for improvement and in some cases identification of barriers to uptake of the particular standards. Furthermore, during the site visit, the surveyors may further identify barriers and offer suggestions for effective strategies for overcoming the identified barriers. These suggestions may be included in the final accreditation report. For example, a standard may require that a hand-washing procedure is in place, with evidence of its effectiveness. How that procedure is designed and implemented is the decision of the client organization. Throughout this design period and then assessment of its effectiveness after implementation, barriers and facilitators to the process are identified and adjustments made in order to obtain the optimum result for the client organization, their patients and staff. | Carefully reviewing each standard and then adapting the implementation to apply to their context are critical components from the beginning of the self-assessment process to the development of the quality improvement action plan. The client organization identifies those factors that are barriers and facilitators and indicates how they will be addressed in the action or implementation plan. Thus, if the standard requires an annual board evaluation, the type of tool utilized, the content, the means of administration, steps taken to analyze and actions taken to address the results lie with the client organization. Barriers to undertaking this exercise must be considered as well as those factors that will facilitate achieving this standard. Once the strategy is implemented, monitoring its effectiveness is important as is making corrections to the strategy as necessary to enable buy-in and achievement of the goal. |
| ‘Select, tailor and activate implementation strategies (the action plan)’ KT goal: to tailor implementation strategies to the identified barriers so as to increase implementation success. | The implementation strategy or quality improvement action plan that is developed by teams during the self-assessment process is the responsibility of the client organization—both to implement and monitor progress. Most accreditation bodies require that progress on this plan is provided back to them on a regular basis, e.g. every 6 months or annually. The accreditation report that is given to the organization post the on-site visit reinforces the actions that are required and assists in the determination of priorities for action. Other implementation strategies supported by accreditation bodies include providing education and training based on the learning needs of the client organization. Given the wealth of information that is obtained both online and during the on-site visit, many accreditation bodies are creating a ‘library’ of best or leading implementation practices that is accessible to all client organizations. The accreditation body develops eligibility criteria against which to assess if a strategy indeed qualifies as a best or leading practice (e.g. clinical, service, governance/leadership). | The quality improvement action plan is unique to each client organization and should ideally consider identified barriers to implementing the standards and identify how selected implementation strategies will address the barriers. There are many different implementation strategies to achieve uptake of a particular standard/criterion. Client organizations are encouraged to identify those strategies most relevant to them, optimizing buy-ins and results. Teams together develop these plans. The accreditation report is a useful tool for the client organization, confirming areas important to focus actions. Within the specified timeframes as to when reports should be provided to the accreditation body, the client organization’s implementation strategies are developed, monitored and assessed accordingly. The sharing of ‘leading or best practices’ between organizations is a major benefit for all client organizations. Rather than ‘reinventing the wheel’ to identify a strategy to meet a particular standard, reviewing what other client organizations have considered is very helpful. The client organization may then contact the ‘owner’ of that leading practice, seek advice and then consider and/or adapt that practice to their own setting, or choose to reject it. |
| ‘Monitor use of the standards’ KT goal: to determine the extent to which the organization is adhering to the standards so that the organization can assess its performance against the desired practice (the standard). The monitoring of indicators serves as a mechanism to ensure/facilitate that users’ knowledge and practice are ‘keeping pace’. | The standards may identify specific indicators that should be monitored to allow assessment of performance toward meeting the standards. Monitoring of strategic and operational indicators/performance measures occurs in all organizations. Utilizing the specific indicators that may be identified by the accreditation body provides further direction to confirm priority areas for monitoring. The accreditation bodies establish a mechanism with the client organizations to have regular contact throughout the accreditation cycle. Generally, following the receipt of the accreditation report, it is required that there be a 6-month report, an annual report or something similar. This ongoing monitoring of compliance and ongoing assessment of implementation of the action plan are critical components of the accreditation process. The goal is that accreditation is not a onetime event but an ongoing cycle, with an expectation of ongoing assessment of compliance with the standards, implementation of action plans, ongoing monitoring and continuing to improve care and services. At minimum, there is an expectation to receive a report, online or hard copy, at regular intervals of progress with the action plans. | The client organization has a responsibility to follow through on the implementation of the quality improvement action plan that results from the survey process. A sincere commitment by the organization to value this process is fundamental to its success and to having maximum impact on quality of care. Monitoring of strategic and operational indicators/performance measures occurs in all organizations. Utilizing specific indicators identified by the accreditation body provides further direction to confirm priority areas for monitoring and are used to determine adherence to the standards. The client organization recognizes that accreditation is a major quality improvement tool that complements other quality improvement strategies within their organization, e.g. LEAN, Six Sigma, etc. The client organization’s overall quality improvement plan at a strategic level acknowledges how these initiatives comprehensively integrate to enable improvement of care and services, from the governance level to the point of care. |
| ‘Evaluate outcome/impact’ KT goal: to determine the extent to which adherence to the standards translate into improved health outcomes or health system outcomes. This information can further motivate maintaining adherence to the standards and to celebrate organizational achievements. | As the primary goal of accreditation is to improve quality and safety, requirements to report on specific outcomes or specific clinical indicators may not be required by accreditation bodies. However, one of the key goals of accreditation is to provide an organization with tools that enable resilience. The content of the standards focuses on quality improvement and the prevention or mitigation of risk. If an adverse event arises, the organization knows how to learn from the event, recover and continue improving. Thus, accreditation does not guarantee quality of care but demonstrates accountability that the organization is focused on improvement and meeting evidence-based standards. | If outcomes of adherence to standards are collected, client organizations can use this information to justify implementing the standards, demonstrate to the community how they improve patient health outcomes and better demonstrate the value of money invested in healthcare. The challenge, however, is that the standard alone does not directly improve outcomes. Factors such as the knowledge and expertise of the ‘user’, patient behaviors and resource availability combine to enable the desired outcome. |
| ‘Sustain use of standards’ KT goal: to continue to focus the organization on maintaining adherence to the standard and maintaining quality and patient safety. If declines in adherence are observed, the organization can double efforts to identify barriers to ongoing use of the standards and institute more/different implementation strategies (starting the knowledge to action cycle over again). | If the accreditation body becomes concerned about the performance of the client organization, i.e. that insufficient attention is being paid to areas of concerns/deficiencies, or perhaps significant complaints from the public have been received by the accreditation body, mechanisms are in place to send a surveyor to the organization mid-cycle. Similar strategies can also be undertaken to identify problems and suggest improvements. This relationship is critical and an important part of the accreditation process. It provides support and assists with quality improvement and the implementation of recommendations. From one on-site visit to the next, the ongoing relationship with the client organization is sustained. Additional education and training are provided as appropriate to the client organization and its needs. Ongoing monitoring of performance is critical to sustaining standards use. | Client organizations are encouraged to use the standards in an ongoing way, perhaps to annually review the relevant standards. For example, the Emergency Department team should review the standards for emergency care annually, conduct a self-assessment and continuously monitor adherence to the standards. Are any new deficiencies identified? If the standard has been updated since previously utilized, there may be new important knowledge/practices to consider and be included in the quality improvement plan, including mechanisms to monitor progress. |
| Mapping to ‘knowledge to action cycle’ . | Accreditation body program elements . | Description of client actions and rationale . |
|---|---|---|
| Knowledge/standards creation | ||
| ‘Knowledge/standards’ KT goal: to identify the knowledge to be implemented to optimize quality of care and patient safety. | Standards synthesize the best available evidence and expert opinion to offer guidance on how to enable quality improvement, mitigate safety risks and improve quality. These standards are reviewed regularly to ensure they are reflective of the current evidence. | The client organization implements or attempts to implement these standards on a regular basis, at minimum 1 year prior to the on-site survey visit. The currency and evidence-informed nature of the standards support the client organization in achieving their goal of keeping practices and decision-making current. |
| ‘Knowledge tools/products’ KT goal: to provide resources to facilitate meeting accreditation requirements and to encourage engagement with phases of the action cycle. | Specific assessment tools such as a staff engagement survey and/or a patient safety culture survey may be required which are utilized by the client organization on a cyclic basis. The results contribute toward identifying achievement of a particular standard criterion. These tools are often embedded in the accreditation body’s software that is made available to all client organizations. | The survey tools are of value to the client organization in that the results can be used, even in isolation from the standards assessment, to identify areas of strength or deficiency requiring an action plan. The tools could be reapplied at an appropriate interval to determine if change has occurred in the desired direction. |
| Action Phases | ||
| ‘Determine the standards/practice–achievement gap’ KT goal: to determine gaps between the standards and current practice–achievement so as to quantify the need for improvement. This information can be used to promote organizational consensus on the need to act to reduce the gap. | The accreditation body encourages the client organization to conduct a self-assessment against the standards. The purpose of this exercise is to enable identification of areas of strength and areas for improvement. The survey tools facilitate in identifying areas of strength and areas for improvement further strengthening the assessment of performance against a particular standard. The accreditation body organizes an on-site survey visit, conducted by surveyors carefully selected for their expertise and training, which is a vital component of their third-party external review process. The surveyors use different methodologies depending on the accreditation body’s program. At minimum it includes that surveyors visit the client organization in person to gather evidence of current practice which they can compare to the practice described in the standards. During the on-site visit, surveyors may interview the board, leadership, staff, patients, their families and key stakeholders in the community. The surveyors observe the environment, staff interactions and review documentation in the health record and policies. During discussion with individuals, the surveyors may provide feedback and evidence back to each team to encourage their practice going forward, reinforce those areas requiring improvement and share their own expertise. | The client organization conducts the self-assessment to determine the degree to which they achieve a particular standard and the specific criteria within the standard. This process enables their identification of performance relative to the standard and areas in which there are opportunities for improvement, as well as organizational readiness for change. The identified areas for improvement then become the focus of the client organization’s quality improvement action plan to address areas needing improvement. It is the decision of the client organization as to how the self-assessment process is conducted—whether an entire team collectively completes the assessment or whether a designated person does this on behalf of the team. Depending on the information technology resources of the client organization, the exercise may be conducted ‘online’ or manually on paper and then entered into the accreditation body’s software program. The survey instruments (e.g. staff engagement, patient safety culture) generally require involvement of staff, individually or as a team. In addition to providing useful results in identifying areas of strength and areas of improvement, the process contributes to team building. The client organization prepares for the on-site visit to ensure all necessary information is available for the surveyors, including availability of teams to be interviewed and preparation to enable observation of care/service being provided (e.g. surgery in the OR, a clinic as patients receive treatment). The recipients of care are available to speak with a surveyor when required while at all times maintaining anonymity and confidentiality to the degree necessary. Copies of health records are made available as appropriate. |
| ‘Customize operationalization of standards to local context’ KT goal: to adapt and customize the operationalization of the standard to foster organizational buy-in and contribute to optimal implementation of standards tailored to organizational needs. | While the standards are set and somewhat prescriptive, the accreditation body encourages the client organizations to review and develop an implementation strategy that is relevant to their own context. While standards outline a particular desired practice or result, the means by which this is achieved, the “how”, is the decision of the client organization. | The client organization has the responsibility to carefully assess each standard and determine how best to implement/achieve the standards within their own context. Every client organization’s structure, patient population, staffing arrangement and resource availability is different. There are unique elements in every client organization’s milieu. |
| ‘Assess barriers/facilitators to standards use’ KT goal: to identify potential barriers (and facilitators) to implementing the standards. This information can be used to more strategically to select implementation strategies explicitly targeting the barriers, thereby improving implementation success. | The self-assessment process enables the identification of the degree to which a standard is being achieved, identification of gaps or areas for improvement and in some cases identification of barriers to uptake of the particular standards. Furthermore, during the site visit, the surveyors may further identify barriers and offer suggestions for effective strategies for overcoming the identified barriers. These suggestions may be included in the final accreditation report. For example, a standard may require that a hand-washing procedure is in place, with evidence of its effectiveness. How that procedure is designed and implemented is the decision of the client organization. Throughout this design period and then assessment of its effectiveness after implementation, barriers and facilitators to the process are identified and adjustments made in order to obtain the optimum result for the client organization, their patients and staff. | Carefully reviewing each standard and then adapting the implementation to apply to their context are critical components from the beginning of the self-assessment process to the development of the quality improvement action plan. The client organization identifies those factors that are barriers and facilitators and indicates how they will be addressed in the action or implementation plan. Thus, if the standard requires an annual board evaluation, the type of tool utilized, the content, the means of administration, steps taken to analyze and actions taken to address the results lie with the client organization. Barriers to undertaking this exercise must be considered as well as those factors that will facilitate achieving this standard. Once the strategy is implemented, monitoring its effectiveness is important as is making corrections to the strategy as necessary to enable buy-in and achievement of the goal. |
| ‘Select, tailor and activate implementation strategies (the action plan)’ KT goal: to tailor implementation strategies to the identified barriers so as to increase implementation success. | The implementation strategy or quality improvement action plan that is developed by teams during the self-assessment process is the responsibility of the client organization—both to implement and monitor progress. Most accreditation bodies require that progress on this plan is provided back to them on a regular basis, e.g. every 6 months or annually. The accreditation report that is given to the organization post the on-site visit reinforces the actions that are required and assists in the determination of priorities for action. Other implementation strategies supported by accreditation bodies include providing education and training based on the learning needs of the client organization. Given the wealth of information that is obtained both online and during the on-site visit, many accreditation bodies are creating a ‘library’ of best or leading implementation practices that is accessible to all client organizations. The accreditation body develops eligibility criteria against which to assess if a strategy indeed qualifies as a best or leading practice (e.g. clinical, service, governance/leadership). | The quality improvement action plan is unique to each client organization and should ideally consider identified barriers to implementing the standards and identify how selected implementation strategies will address the barriers. There are many different implementation strategies to achieve uptake of a particular standard/criterion. Client organizations are encouraged to identify those strategies most relevant to them, optimizing buy-ins and results. Teams together develop these plans. The accreditation report is a useful tool for the client organization, confirming areas important to focus actions. Within the specified timeframes as to when reports should be provided to the accreditation body, the client organization’s implementation strategies are developed, monitored and assessed accordingly. The sharing of ‘leading or best practices’ between organizations is a major benefit for all client organizations. Rather than ‘reinventing the wheel’ to identify a strategy to meet a particular standard, reviewing what other client organizations have considered is very helpful. The client organization may then contact the ‘owner’ of that leading practice, seek advice and then consider and/or adapt that practice to their own setting, or choose to reject it. |
| ‘Monitor use of the standards’ KT goal: to determine the extent to which the organization is adhering to the standards so that the organization can assess its performance against the desired practice (the standard). The monitoring of indicators serves as a mechanism to ensure/facilitate that users’ knowledge and practice are ‘keeping pace’. | The standards may identify specific indicators that should be monitored to allow assessment of performance toward meeting the standards. Monitoring of strategic and operational indicators/performance measures occurs in all organizations. Utilizing the specific indicators that may be identified by the accreditation body provides further direction to confirm priority areas for monitoring. The accreditation bodies establish a mechanism with the client organizations to have regular contact throughout the accreditation cycle. Generally, following the receipt of the accreditation report, it is required that there be a 6-month report, an annual report or something similar. This ongoing monitoring of compliance and ongoing assessment of implementation of the action plan are critical components of the accreditation process. The goal is that accreditation is not a onetime event but an ongoing cycle, with an expectation of ongoing assessment of compliance with the standards, implementation of action plans, ongoing monitoring and continuing to improve care and services. At minimum, there is an expectation to receive a report, online or hard copy, at regular intervals of progress with the action plans. | The client organization has a responsibility to follow through on the implementation of the quality improvement action plan that results from the survey process. A sincere commitment by the organization to value this process is fundamental to its success and to having maximum impact on quality of care. Monitoring of strategic and operational indicators/performance measures occurs in all organizations. Utilizing specific indicators identified by the accreditation body provides further direction to confirm priority areas for monitoring and are used to determine adherence to the standards. The client organization recognizes that accreditation is a major quality improvement tool that complements other quality improvement strategies within their organization, e.g. LEAN, Six Sigma, etc. The client organization’s overall quality improvement plan at a strategic level acknowledges how these initiatives comprehensively integrate to enable improvement of care and services, from the governance level to the point of care. |
| ‘Evaluate outcome/impact’ KT goal: to determine the extent to which adherence to the standards translate into improved health outcomes or health system outcomes. This information can further motivate maintaining adherence to the standards and to celebrate organizational achievements. | As the primary goal of accreditation is to improve quality and safety, requirements to report on specific outcomes or specific clinical indicators may not be required by accreditation bodies. However, one of the key goals of accreditation is to provide an organization with tools that enable resilience. The content of the standards focuses on quality improvement and the prevention or mitigation of risk. If an adverse event arises, the organization knows how to learn from the event, recover and continue improving. Thus, accreditation does not guarantee quality of care but demonstrates accountability that the organization is focused on improvement and meeting evidence-based standards. | If outcomes of adherence to standards are collected, client organizations can use this information to justify implementing the standards, demonstrate to the community how they improve patient health outcomes and better demonstrate the value of money invested in healthcare. The challenge, however, is that the standard alone does not directly improve outcomes. Factors such as the knowledge and expertise of the ‘user’, patient behaviors and resource availability combine to enable the desired outcome. |
| ‘Sustain use of standards’ KT goal: to continue to focus the organization on maintaining adherence to the standard and maintaining quality and patient safety. If declines in adherence are observed, the organization can double efforts to identify barriers to ongoing use of the standards and institute more/different implementation strategies (starting the knowledge to action cycle over again). | If the accreditation body becomes concerned about the performance of the client organization, i.e. that insufficient attention is being paid to areas of concerns/deficiencies, or perhaps significant complaints from the public have been received by the accreditation body, mechanisms are in place to send a surveyor to the organization mid-cycle. Similar strategies can also be undertaken to identify problems and suggest improvements. This relationship is critical and an important part of the accreditation process. It provides support and assists with quality improvement and the implementation of recommendations. From one on-site visit to the next, the ongoing relationship with the client organization is sustained. Additional education and training are provided as appropriate to the client organization and its needs. Ongoing monitoring of performance is critical to sustaining standards use. | Client organizations are encouraged to use the standards in an ongoing way, perhaps to annually review the relevant standards. For example, the Emergency Department team should review the standards for emergency care annually, conduct a self-assessment and continuously monitor adherence to the standards. Are any new deficiencies identified? If the standard has been updated since previously utilized, there may be new important knowledge/practices to consider and be included in the quality improvement plan, including mechanisms to monitor progress. |
| Mapping to ‘knowledge to action cycle’ . | Accreditation body program elements . | Description of client actions and rationale . |
|---|---|---|
| Knowledge/standards creation | ||
| ‘Knowledge/standards’ KT goal: to identify the knowledge to be implemented to optimize quality of care and patient safety. | Standards synthesize the best available evidence and expert opinion to offer guidance on how to enable quality improvement, mitigate safety risks and improve quality. These standards are reviewed regularly to ensure they are reflective of the current evidence. | The client organization implements or attempts to implement these standards on a regular basis, at minimum 1 year prior to the on-site survey visit. The currency and evidence-informed nature of the standards support the client organization in achieving their goal of keeping practices and decision-making current. |
| ‘Knowledge tools/products’ KT goal: to provide resources to facilitate meeting accreditation requirements and to encourage engagement with phases of the action cycle. | Specific assessment tools such as a staff engagement survey and/or a patient safety culture survey may be required which are utilized by the client organization on a cyclic basis. The results contribute toward identifying achievement of a particular standard criterion. These tools are often embedded in the accreditation body’s software that is made available to all client organizations. | The survey tools are of value to the client organization in that the results can be used, even in isolation from the standards assessment, to identify areas of strength or deficiency requiring an action plan. The tools could be reapplied at an appropriate interval to determine if change has occurred in the desired direction. |
| Action Phases | ||
| ‘Determine the standards/practice–achievement gap’ KT goal: to determine gaps between the standards and current practice–achievement so as to quantify the need for improvement. This information can be used to promote organizational consensus on the need to act to reduce the gap. | The accreditation body encourages the client organization to conduct a self-assessment against the standards. The purpose of this exercise is to enable identification of areas of strength and areas for improvement. The survey tools facilitate in identifying areas of strength and areas for improvement further strengthening the assessment of performance against a particular standard. The accreditation body organizes an on-site survey visit, conducted by surveyors carefully selected for their expertise and training, which is a vital component of their third-party external review process. The surveyors use different methodologies depending on the accreditation body’s program. At minimum it includes that surveyors visit the client organization in person to gather evidence of current practice which they can compare to the practice described in the standards. During the on-site visit, surveyors may interview the board, leadership, staff, patients, their families and key stakeholders in the community. The surveyors observe the environment, staff interactions and review documentation in the health record and policies. During discussion with individuals, the surveyors may provide feedback and evidence back to each team to encourage their practice going forward, reinforce those areas requiring improvement and share their own expertise. | The client organization conducts the self-assessment to determine the degree to which they achieve a particular standard and the specific criteria within the standard. This process enables their identification of performance relative to the standard and areas in which there are opportunities for improvement, as well as organizational readiness for change. The identified areas for improvement then become the focus of the client organization’s quality improvement action plan to address areas needing improvement. It is the decision of the client organization as to how the self-assessment process is conducted—whether an entire team collectively completes the assessment or whether a designated person does this on behalf of the team. Depending on the information technology resources of the client organization, the exercise may be conducted ‘online’ or manually on paper and then entered into the accreditation body’s software program. The survey instruments (e.g. staff engagement, patient safety culture) generally require involvement of staff, individually or as a team. In addition to providing useful results in identifying areas of strength and areas of improvement, the process contributes to team building. The client organization prepares for the on-site visit to ensure all necessary information is available for the surveyors, including availability of teams to be interviewed and preparation to enable observation of care/service being provided (e.g. surgery in the OR, a clinic as patients receive treatment). The recipients of care are available to speak with a surveyor when required while at all times maintaining anonymity and confidentiality to the degree necessary. Copies of health records are made available as appropriate. |
| ‘Customize operationalization of standards to local context’ KT goal: to adapt and customize the operationalization of the standard to foster organizational buy-in and contribute to optimal implementation of standards tailored to organizational needs. | While the standards are set and somewhat prescriptive, the accreditation body encourages the client organizations to review and develop an implementation strategy that is relevant to their own context. While standards outline a particular desired practice or result, the means by which this is achieved, the “how”, is the decision of the client organization. | The client organization has the responsibility to carefully assess each standard and determine how best to implement/achieve the standards within their own context. Every client organization’s structure, patient population, staffing arrangement and resource availability is different. There are unique elements in every client organization’s milieu. |
| ‘Assess barriers/facilitators to standards use’ KT goal: to identify potential barriers (and facilitators) to implementing the standards. This information can be used to more strategically to select implementation strategies explicitly targeting the barriers, thereby improving implementation success. | The self-assessment process enables the identification of the degree to which a standard is being achieved, identification of gaps or areas for improvement and in some cases identification of barriers to uptake of the particular standards. Furthermore, during the site visit, the surveyors may further identify barriers and offer suggestions for effective strategies for overcoming the identified barriers. These suggestions may be included in the final accreditation report. For example, a standard may require that a hand-washing procedure is in place, with evidence of its effectiveness. How that procedure is designed and implemented is the decision of the client organization. Throughout this design period and then assessment of its effectiveness after implementation, barriers and facilitators to the process are identified and adjustments made in order to obtain the optimum result for the client organization, their patients and staff. | Carefully reviewing each standard and then adapting the implementation to apply to their context are critical components from the beginning of the self-assessment process to the development of the quality improvement action plan. The client organization identifies those factors that are barriers and facilitators and indicates how they will be addressed in the action or implementation plan. Thus, if the standard requires an annual board evaluation, the type of tool utilized, the content, the means of administration, steps taken to analyze and actions taken to address the results lie with the client organization. Barriers to undertaking this exercise must be considered as well as those factors that will facilitate achieving this standard. Once the strategy is implemented, monitoring its effectiveness is important as is making corrections to the strategy as necessary to enable buy-in and achievement of the goal. |
| ‘Select, tailor and activate implementation strategies (the action plan)’ KT goal: to tailor implementation strategies to the identified barriers so as to increase implementation success. | The implementation strategy or quality improvement action plan that is developed by teams during the self-assessment process is the responsibility of the client organization—both to implement and monitor progress. Most accreditation bodies require that progress on this plan is provided back to them on a regular basis, e.g. every 6 months or annually. The accreditation report that is given to the organization post the on-site visit reinforces the actions that are required and assists in the determination of priorities for action. Other implementation strategies supported by accreditation bodies include providing education and training based on the learning needs of the client organization. Given the wealth of information that is obtained both online and during the on-site visit, many accreditation bodies are creating a ‘library’ of best or leading implementation practices that is accessible to all client organizations. The accreditation body develops eligibility criteria against which to assess if a strategy indeed qualifies as a best or leading practice (e.g. clinical, service, governance/leadership). | The quality improvement action plan is unique to each client organization and should ideally consider identified barriers to implementing the standards and identify how selected implementation strategies will address the barriers. There are many different implementation strategies to achieve uptake of a particular standard/criterion. Client organizations are encouraged to identify those strategies most relevant to them, optimizing buy-ins and results. Teams together develop these plans. The accreditation report is a useful tool for the client organization, confirming areas important to focus actions. Within the specified timeframes as to when reports should be provided to the accreditation body, the client organization’s implementation strategies are developed, monitored and assessed accordingly. The sharing of ‘leading or best practices’ between organizations is a major benefit for all client organizations. Rather than ‘reinventing the wheel’ to identify a strategy to meet a particular standard, reviewing what other client organizations have considered is very helpful. The client organization may then contact the ‘owner’ of that leading practice, seek advice and then consider and/or adapt that practice to their own setting, or choose to reject it. |
| ‘Monitor use of the standards’ KT goal: to determine the extent to which the organization is adhering to the standards so that the organization can assess its performance against the desired practice (the standard). The monitoring of indicators serves as a mechanism to ensure/facilitate that users’ knowledge and practice are ‘keeping pace’. | The standards may identify specific indicators that should be monitored to allow assessment of performance toward meeting the standards. Monitoring of strategic and operational indicators/performance measures occurs in all organizations. Utilizing the specific indicators that may be identified by the accreditation body provides further direction to confirm priority areas for monitoring. The accreditation bodies establish a mechanism with the client organizations to have regular contact throughout the accreditation cycle. Generally, following the receipt of the accreditation report, it is required that there be a 6-month report, an annual report or something similar. This ongoing monitoring of compliance and ongoing assessment of implementation of the action plan are critical components of the accreditation process. The goal is that accreditation is not a onetime event but an ongoing cycle, with an expectation of ongoing assessment of compliance with the standards, implementation of action plans, ongoing monitoring and continuing to improve care and services. At minimum, there is an expectation to receive a report, online or hard copy, at regular intervals of progress with the action plans. | The client organization has a responsibility to follow through on the implementation of the quality improvement action plan that results from the survey process. A sincere commitment by the organization to value this process is fundamental to its success and to having maximum impact on quality of care. Monitoring of strategic and operational indicators/performance measures occurs in all organizations. Utilizing specific indicators identified by the accreditation body provides further direction to confirm priority areas for monitoring and are used to determine adherence to the standards. The client organization recognizes that accreditation is a major quality improvement tool that complements other quality improvement strategies within their organization, e.g. LEAN, Six Sigma, etc. The client organization’s overall quality improvement plan at a strategic level acknowledges how these initiatives comprehensively integrate to enable improvement of care and services, from the governance level to the point of care. |
| ‘Evaluate outcome/impact’ KT goal: to determine the extent to which adherence to the standards translate into improved health outcomes or health system outcomes. This information can further motivate maintaining adherence to the standards and to celebrate organizational achievements. | As the primary goal of accreditation is to improve quality and safety, requirements to report on specific outcomes or specific clinical indicators may not be required by accreditation bodies. However, one of the key goals of accreditation is to provide an organization with tools that enable resilience. The content of the standards focuses on quality improvement and the prevention or mitigation of risk. If an adverse event arises, the organization knows how to learn from the event, recover and continue improving. Thus, accreditation does not guarantee quality of care but demonstrates accountability that the organization is focused on improvement and meeting evidence-based standards. | If outcomes of adherence to standards are collected, client organizations can use this information to justify implementing the standards, demonstrate to the community how they improve patient health outcomes and better demonstrate the value of money invested in healthcare. The challenge, however, is that the standard alone does not directly improve outcomes. Factors such as the knowledge and expertise of the ‘user’, patient behaviors and resource availability combine to enable the desired outcome. |
| ‘Sustain use of standards’ KT goal: to continue to focus the organization on maintaining adherence to the standard and maintaining quality and patient safety. If declines in adherence are observed, the organization can double efforts to identify barriers to ongoing use of the standards and institute more/different implementation strategies (starting the knowledge to action cycle over again). | If the accreditation body becomes concerned about the performance of the client organization, i.e. that insufficient attention is being paid to areas of concerns/deficiencies, or perhaps significant complaints from the public have been received by the accreditation body, mechanisms are in place to send a surveyor to the organization mid-cycle. Similar strategies can also be undertaken to identify problems and suggest improvements. This relationship is critical and an important part of the accreditation process. It provides support and assists with quality improvement and the implementation of recommendations. From one on-site visit to the next, the ongoing relationship with the client organization is sustained. Additional education and training are provided as appropriate to the client organization and its needs. Ongoing monitoring of performance is critical to sustaining standards use. | Client organizations are encouraged to use the standards in an ongoing way, perhaps to annually review the relevant standards. For example, the Emergency Department team should review the standards for emergency care annually, conduct a self-assessment and continuously monitor adherence to the standards. Are any new deficiencies identified? If the standard has been updated since previously utilized, there may be new important knowledge/practices to consider and be included in the quality improvement plan, including mechanisms to monitor progress. |
Illustrative scenarios aligning two different accreditation programs (Canada and Australia) with the knowledge to action cycle
| Knowledge to action component . | Illustrative example from the Accreditation Canada Qmentum Program [The medication management standard is used as an example]: carriage return www.accreditation.ca Accreditation Canada is a not-for-profit organization established in the 1950s as a provider of health services accreditation. Clients include healthcare organizations across the continuum from home and community to acute care and palliative care. . | Illustrative example from the AGPAL Accreditation Organization applying the National Safety and Quality Health Service (NSQHS) Standards www.agpal.com.au Australian General Practice Accreditation Limited (AGPAL) is a leading not-for-profit organization, established in 1997 as a provider for general practice accreditation and quality improvement services within Australia. . |
|---|---|---|
| Knowledge/standards creation | ||
| Knowledge/standards, products/tools | -Based on the best evidence and input from patients, providers, product users, researchers and policymakers, the medication management standard for acute care organizations specifies organizational-level requirements that prevent and reduce patient safety incidents involving medications carriage return.—The standard addresses all aspects of the medication management process (e.g. ‘ensuring the people managing medications are educated and competent; managing client and medication information’).—The standard incorporates required (mandatory) organizational practices (ROPs) such as antimicrobial stewardship and medication reconciliation to ensure evidence-based practices are embedded in care delivery.—The standards are regularly reviewed, and where needed based on changes in evidence, revised every 5 years to remain relevant and applicable. | -The NSQHS Standards have numerous requirements for health services to be consistent with evidence-based practices including: 5.13 Clinicians use processes for shared decision-making to develop and document a comprehensive and individualized plan that: f. Is consistent with best practice and evidence -As standards are developed, the evidence required for each indicator is determined and from where this evidence can be obtained, e.g. document review, interview or observation. -The NSQHS Standards are owned by the Australian Commission on Safety and Quality in Health Care. The Commission has a process for keeping the standards up to date with the emerging evidence. The Commission also has a ‘live literature searches’ function on their website that can be used to find evidence to support best practice in line with the NSQHS Standards. The Commission provides accrediting agencies with NSQHS Standards Advisories as a formal communication from the Commission to provide guidance and direction on the interpretation and/or assessment of the NSQHS Standards. The NSQHS Standards advisories are routinely reviewed to ensure they remain current and supported by available evidence. |
| Action cycle | ||
| Elements include: determine the standards/practice–achievement gap, customize operationalization of standards to the local context, assess barriers/facilitators to standards use (meeting the standards), select, tailor and activate implementation strategies (action plan), monitor standards use and evaluate outcomes | - Organizations use this standard to conduct self-assessments across acute care units (e.g. emergency department, critical care, etc.), typically a year before an on-site survey visit although they are encouraged to self-assess on a more regular schedule as well, e.g. carriage return annually. -The self-assessment results are used by organizations to identify areas for improvement and provide the foundation to collaboratively develop an action plan. -Accredited organizations are required to conduct surveys using instruments (e.g. patient experience, governance, patient safety culture, worklife ‘pulse’ assessment of the environment for staff and physicians). -Self-assessments and surveys are completed using a secure online client portal that allows the client organization to view the standard criterion, guidance, survey instruments and their results. -The accreditation process encourages formal self-assessment as well as third-party assessment of facilitators and barriers organizations may experience in their effort to meet the standards. It allows organizations to have a clear understanding of how well they meet each criterion within a standard and to monitor trends over time. | -All accredited organizations undertake self-assessment via online self-assessment software. This self-assessment process using AccreditationPro enables the active involvement of individual staff or teams, engaging the whole organization in the self-assessment process and preparation for accreditation. -Each indicator or criterion is rated as ‘met’ or ‘not met’. If rated as ‘not met’, the client organizations can then develop an action plan for that specific indicator which includes: • The action that needs to occur • Progress notes • Person responsible • Due date • Completion -Outstanding actions or improvements must be completed before the self-assessment can be submitted. The self-assessment process via AccreditationPro cannot be submitted until all indicators/criteria have been rated as met. This forcing factor ensures that client organizations address each indicator. If any indicators are rated as ‘not met’, the client organization is directed to complete all indicators as met before the self-assessment can be submitted. When a client organization rates an indicator a ‘not met’, they commence an action plan for that indicator. Not until all actions within the action plan have been completed can the client organization confirm that the indicator has now been ‘met’ and submission of AccreditationPro is then able to occur. |
| -The results of accredited organizations’ survey data and their respective action plans are reviewed by the survey team and discussed as part of the on-site visit. For example, poor results on a patient experience survey may lead to a further inquiry on the processes used for patient and family engagement, staff and physician training and assessment of patient/family advisory committees. Furthermore, the assessment team would explore what interventions the accredited organization has implemented to address the results and evaluate progress made. This helps to inform whether accredited organizations are successfully meeting the standards. -Accreditation Canada offers education and training aligned to these standards to support client organizations. -Upon conclusion of the on-site assessment, the surveyor team recommends an accreditation decision based on results, assessment of risk and accreditation decision guidelines. Surveyor inputs and observations are vital components. -Survey instrument data and respective action plans are reviewed by the survey team and discussed as part of the on-site visit. -Client organizations may submit relevant information (e.g. evidence that demonstrate a criterion is being met) in advance of an on-site visit. One medication management example is ‘The interdisciplinary committee has defined roles and responsibilities for medication management that are in line with legislation and applicable regulations’. carriage return -The process of assessment includes evaluation against each standard criterion. For example, with medication management, the surveyors would seek evidence that ‘Pharmacists collaborate with clients and interprofessional clinical teams to provide care using evidence-informed care activities associated with improved client and system outcomes’. -Surveyor qualification typically includes practicing physicians, nurses, therapists, pharmacists and administrators with a demonstrated experience in quality and safety. Since 2019 patient surveyors have been incorporated into the surveyor teams. Patient surveyors focus on people-centered care criteria. Surveyors use a combination of methods to assess medication management criteria (e.g. direct observation, patient and provider interviews, chart review, etc.). -The on-site assessment enables a review of the evidence that the standards have been achieved and/or where gaps are identified as noted in performance measures such as medication error rates and evidence of collaboration. -Upon conclusion of the on-site assessment, the surveyor team recommends an accreditation decision based on results, assessment of risk and accreditation decision guidelines. | -To support the selection, tailoring and development of the action plan, client organizations assess/identify any barriers or knowledge needed in order to meet the standards. AccreditationPro includes a resource library that consists of a variety of resources including direct links to external websites, policies, procedures and templates to assist client organizations to reduce any barriers that they may find in meeting the requirements of the standards. Each resource can be linked directly to the specific indicator/criteria within AccreditationPro which provides the client organization with instant access to resources to support them in meeting the indicators/standards. -AGPAL provides a direct support for the implementation interventions/strategies by offering education and training to client organizations to assist them to overcome knowledge barriers related to the standards or processes required to meet the standards. The types of education and training activities range from face-to-face workshops, webinars and online modules. -Throughout the on-site survey, surveyors/assessors rate compliance with the standards. Findings are collated into a final report, and these data are intended to assist organizations identify where further improvement is required. -AGPAL requires the collection of outcomes related to the use of the standards. The use of the NSQHS Standards have the following outcomes: • Decreased rates of healthcare-associated infections. • Decreased in-hospital cardiac arrests. • Increased documentation of adverse drug reactions and medication histories. • Decreased prescribing of antibiotics due to improvements in antibiotic stewardship. -The AGPAL decision-making framework states decisions will be timely and made within a fair and transparent decision-making framework. The client organization has the opportunity to respond to the draft before the final accreditation decision. -The principles of decision-making incorporate natural justice, transparency and independence (no conflict of interest and impartiality). -Decision process: Decision-makers rely substantially on the information supplied by the assessment team including the assessment report, assessor comments, the corrective actions taken by the client organization and the accredited organization’s assessment history. -Accreditation report: The accreditation report is provided to the client organization within specified timeframes with the expectation that it will be used to continue to make necessary improvements and maintain the improvements made. | |
| -The final accreditation decision is conferred by an independent body, the Accreditation Decision Committee (ADC). They review results, summarize findings and prepare a report within 3 weeks of the on-site assessment. -Organizations that successfully complete the Accreditation Canada Qmentum program are issued an accreditation award and are eligible to receive the Accreditation Canada banner and seal. -Organizations that are unsuccessful in their accreditation may undergo a supplementary survey within 5 months of the original ADC decision. | ||
| Sustain standards use | - To ensure continuous quality improvement, Accreditation Canada is evolving assessments to sequential assessments, whereby organizations and health systems receive targeted surveys on fewer standards every 18–24 months. -Client organizations are encouraged to submit to HSO’s https://healthstandards.org/leading-practices/, a good example of how the program enables the spread of evidence-based practice and innovations across the country. A leading practice is a practice carried out by a health and/or social service organization that has demonstrated a positive change and is people-centered, safe and efficient. This further reinforces quality improvement and recognizes organizations and health systems. -Accreditation Canada offers ongoing education and training aligned to standards to support client organizations. | -All the follow-up mechanisms provide ongoing maintenance of an accredited organization’s progress against the standards and assist them in preparing for the next accreditation cycle, i.e. supports ongoing standard implementation and maintenance via continuous self- evaluation. The follow-up mechanisms include annual and mid-cycle quality improvement plans, mid-cycle on-site assessment, short notice assessment and ongoing support including online resources, webinars, face-to-face training and newsletters. -AGPAL’s ongoing provision of education and training for client organizations also contributes to sustaining of the standards. -Twelve months prior to accredited organizations’ accreditation expiry, contacts via email and phone calls are made with client organizations at 3-month intervals to assist accredited organizations with preparation for their next accreditation survey. |
| Knowledge to action component . | Illustrative example from the Accreditation Canada Qmentum Program [The medication management standard is used as an example]: carriage return www.accreditation.ca Accreditation Canada is a not-for-profit organization established in the 1950s as a provider of health services accreditation. Clients include healthcare organizations across the continuum from home and community to acute care and palliative care. . | Illustrative example from the AGPAL Accreditation Organization applying the National Safety and Quality Health Service (NSQHS) Standards www.agpal.com.au Australian General Practice Accreditation Limited (AGPAL) is a leading not-for-profit organization, established in 1997 as a provider for general practice accreditation and quality improvement services within Australia. . |
|---|---|---|
| Knowledge/standards creation | ||
| Knowledge/standards, products/tools | -Based on the best evidence and input from patients, providers, product users, researchers and policymakers, the medication management standard for acute care organizations specifies organizational-level requirements that prevent and reduce patient safety incidents involving medications carriage return.—The standard addresses all aspects of the medication management process (e.g. ‘ensuring the people managing medications are educated and competent; managing client and medication information’).—The standard incorporates required (mandatory) organizational practices (ROPs) such as antimicrobial stewardship and medication reconciliation to ensure evidence-based practices are embedded in care delivery.—The standards are regularly reviewed, and where needed based on changes in evidence, revised every 5 years to remain relevant and applicable. | -The NSQHS Standards have numerous requirements for health services to be consistent with evidence-based practices including: 5.13 Clinicians use processes for shared decision-making to develop and document a comprehensive and individualized plan that: f. Is consistent with best practice and evidence -As standards are developed, the evidence required for each indicator is determined and from where this evidence can be obtained, e.g. document review, interview or observation. -The NSQHS Standards are owned by the Australian Commission on Safety and Quality in Health Care. The Commission has a process for keeping the standards up to date with the emerging evidence. The Commission also has a ‘live literature searches’ function on their website that can be used to find evidence to support best practice in line with the NSQHS Standards. The Commission provides accrediting agencies with NSQHS Standards Advisories as a formal communication from the Commission to provide guidance and direction on the interpretation and/or assessment of the NSQHS Standards. The NSQHS Standards advisories are routinely reviewed to ensure they remain current and supported by available evidence. |
| Action cycle | ||
| Elements include: determine the standards/practice–achievement gap, customize operationalization of standards to the local context, assess barriers/facilitators to standards use (meeting the standards), select, tailor and activate implementation strategies (action plan), monitor standards use and evaluate outcomes | - Organizations use this standard to conduct self-assessments across acute care units (e.g. emergency department, critical care, etc.), typically a year before an on-site survey visit although they are encouraged to self-assess on a more regular schedule as well, e.g. carriage return annually. -The self-assessment results are used by organizations to identify areas for improvement and provide the foundation to collaboratively develop an action plan. -Accredited organizations are required to conduct surveys using instruments (e.g. patient experience, governance, patient safety culture, worklife ‘pulse’ assessment of the environment for staff and physicians). -Self-assessments and surveys are completed using a secure online client portal that allows the client organization to view the standard criterion, guidance, survey instruments and their results. -The accreditation process encourages formal self-assessment as well as third-party assessment of facilitators and barriers organizations may experience in their effort to meet the standards. It allows organizations to have a clear understanding of how well they meet each criterion within a standard and to monitor trends over time. | -All accredited organizations undertake self-assessment via online self-assessment software. This self-assessment process using AccreditationPro enables the active involvement of individual staff or teams, engaging the whole organization in the self-assessment process and preparation for accreditation. -Each indicator or criterion is rated as ‘met’ or ‘not met’. If rated as ‘not met’, the client organizations can then develop an action plan for that specific indicator which includes: • The action that needs to occur • Progress notes • Person responsible • Due date • Completion -Outstanding actions or improvements must be completed before the self-assessment can be submitted. The self-assessment process via AccreditationPro cannot be submitted until all indicators/criteria have been rated as met. This forcing factor ensures that client organizations address each indicator. If any indicators are rated as ‘not met’, the client organization is directed to complete all indicators as met before the self-assessment can be submitted. When a client organization rates an indicator a ‘not met’, they commence an action plan for that indicator. Not until all actions within the action plan have been completed can the client organization confirm that the indicator has now been ‘met’ and submission of AccreditationPro is then able to occur. |
| -The results of accredited organizations’ survey data and their respective action plans are reviewed by the survey team and discussed as part of the on-site visit. For example, poor results on a patient experience survey may lead to a further inquiry on the processes used for patient and family engagement, staff and physician training and assessment of patient/family advisory committees. Furthermore, the assessment team would explore what interventions the accredited organization has implemented to address the results and evaluate progress made. This helps to inform whether accredited organizations are successfully meeting the standards. -Accreditation Canada offers education and training aligned to these standards to support client organizations. -Upon conclusion of the on-site assessment, the surveyor team recommends an accreditation decision based on results, assessment of risk and accreditation decision guidelines. Surveyor inputs and observations are vital components. -Survey instrument data and respective action plans are reviewed by the survey team and discussed as part of the on-site visit. -Client organizations may submit relevant information (e.g. evidence that demonstrate a criterion is being met) in advance of an on-site visit. One medication management example is ‘The interdisciplinary committee has defined roles and responsibilities for medication management that are in line with legislation and applicable regulations’. carriage return -The process of assessment includes evaluation against each standard criterion. For example, with medication management, the surveyors would seek evidence that ‘Pharmacists collaborate with clients and interprofessional clinical teams to provide care using evidence-informed care activities associated with improved client and system outcomes’. -Surveyor qualification typically includes practicing physicians, nurses, therapists, pharmacists and administrators with a demonstrated experience in quality and safety. Since 2019 patient surveyors have been incorporated into the surveyor teams. Patient surveyors focus on people-centered care criteria. Surveyors use a combination of methods to assess medication management criteria (e.g. direct observation, patient and provider interviews, chart review, etc.). -The on-site assessment enables a review of the evidence that the standards have been achieved and/or where gaps are identified as noted in performance measures such as medication error rates and evidence of collaboration. -Upon conclusion of the on-site assessment, the surveyor team recommends an accreditation decision based on results, assessment of risk and accreditation decision guidelines. | -To support the selection, tailoring and development of the action plan, client organizations assess/identify any barriers or knowledge needed in order to meet the standards. AccreditationPro includes a resource library that consists of a variety of resources including direct links to external websites, policies, procedures and templates to assist client organizations to reduce any barriers that they may find in meeting the requirements of the standards. Each resource can be linked directly to the specific indicator/criteria within AccreditationPro which provides the client organization with instant access to resources to support them in meeting the indicators/standards. -AGPAL provides a direct support for the implementation interventions/strategies by offering education and training to client organizations to assist them to overcome knowledge barriers related to the standards or processes required to meet the standards. The types of education and training activities range from face-to-face workshops, webinars and online modules. -Throughout the on-site survey, surveyors/assessors rate compliance with the standards. Findings are collated into a final report, and these data are intended to assist organizations identify where further improvement is required. -AGPAL requires the collection of outcomes related to the use of the standards. The use of the NSQHS Standards have the following outcomes: • Decreased rates of healthcare-associated infections. • Decreased in-hospital cardiac arrests. • Increased documentation of adverse drug reactions and medication histories. • Decreased prescribing of antibiotics due to improvements in antibiotic stewardship. -The AGPAL decision-making framework states decisions will be timely and made within a fair and transparent decision-making framework. The client organization has the opportunity to respond to the draft before the final accreditation decision. -The principles of decision-making incorporate natural justice, transparency and independence (no conflict of interest and impartiality). -Decision process: Decision-makers rely substantially on the information supplied by the assessment team including the assessment report, assessor comments, the corrective actions taken by the client organization and the accredited organization’s assessment history. -Accreditation report: The accreditation report is provided to the client organization within specified timeframes with the expectation that it will be used to continue to make necessary improvements and maintain the improvements made. | |
| -The final accreditation decision is conferred by an independent body, the Accreditation Decision Committee (ADC). They review results, summarize findings and prepare a report within 3 weeks of the on-site assessment. -Organizations that successfully complete the Accreditation Canada Qmentum program are issued an accreditation award and are eligible to receive the Accreditation Canada banner and seal. -Organizations that are unsuccessful in their accreditation may undergo a supplementary survey within 5 months of the original ADC decision. | ||
| Sustain standards use | - To ensure continuous quality improvement, Accreditation Canada is evolving assessments to sequential assessments, whereby organizations and health systems receive targeted surveys on fewer standards every 18–24 months. -Client organizations are encouraged to submit to HSO’s https://healthstandards.org/leading-practices/, a good example of how the program enables the spread of evidence-based practice and innovations across the country. A leading practice is a practice carried out by a health and/or social service organization that has demonstrated a positive change and is people-centered, safe and efficient. This further reinforces quality improvement and recognizes organizations and health systems. -Accreditation Canada offers ongoing education and training aligned to standards to support client organizations. | -All the follow-up mechanisms provide ongoing maintenance of an accredited organization’s progress against the standards and assist them in preparing for the next accreditation cycle, i.e. supports ongoing standard implementation and maintenance via continuous self- evaluation. The follow-up mechanisms include annual and mid-cycle quality improvement plans, mid-cycle on-site assessment, short notice assessment and ongoing support including online resources, webinars, face-to-face training and newsletters. -AGPAL’s ongoing provision of education and training for client organizations also contributes to sustaining of the standards. -Twelve months prior to accredited organizations’ accreditation expiry, contacts via email and phone calls are made with client organizations at 3-month intervals to assist accredited organizations with preparation for their next accreditation survey. |
Illustrative scenarios aligning two different accreditation programs (Canada and Australia) with the knowledge to action cycle
| Knowledge to action component . | Illustrative example from the Accreditation Canada Qmentum Program [The medication management standard is used as an example]: carriage return www.accreditation.ca Accreditation Canada is a not-for-profit organization established in the 1950s as a provider of health services accreditation. Clients include healthcare organizations across the continuum from home and community to acute care and palliative care. . | Illustrative example from the AGPAL Accreditation Organization applying the National Safety and Quality Health Service (NSQHS) Standards www.agpal.com.au Australian General Practice Accreditation Limited (AGPAL) is a leading not-for-profit organization, established in 1997 as a provider for general practice accreditation and quality improvement services within Australia. . |
|---|---|---|
| Knowledge/standards creation | ||
| Knowledge/standards, products/tools | -Based on the best evidence and input from patients, providers, product users, researchers and policymakers, the medication management standard for acute care organizations specifies organizational-level requirements that prevent and reduce patient safety incidents involving medications carriage return.—The standard addresses all aspects of the medication management process (e.g. ‘ensuring the people managing medications are educated and competent; managing client and medication information’).—The standard incorporates required (mandatory) organizational practices (ROPs) such as antimicrobial stewardship and medication reconciliation to ensure evidence-based practices are embedded in care delivery.—The standards are regularly reviewed, and where needed based on changes in evidence, revised every 5 years to remain relevant and applicable. | -The NSQHS Standards have numerous requirements for health services to be consistent with evidence-based practices including: 5.13 Clinicians use processes for shared decision-making to develop and document a comprehensive and individualized plan that: f. Is consistent with best practice and evidence -As standards are developed, the evidence required for each indicator is determined and from where this evidence can be obtained, e.g. document review, interview or observation. -The NSQHS Standards are owned by the Australian Commission on Safety and Quality in Health Care. The Commission has a process for keeping the standards up to date with the emerging evidence. The Commission also has a ‘live literature searches’ function on their website that can be used to find evidence to support best practice in line with the NSQHS Standards. The Commission provides accrediting agencies with NSQHS Standards Advisories as a formal communication from the Commission to provide guidance and direction on the interpretation and/or assessment of the NSQHS Standards. The NSQHS Standards advisories are routinely reviewed to ensure they remain current and supported by available evidence. |
| Action cycle | ||
| Elements include: determine the standards/practice–achievement gap, customize operationalization of standards to the local context, assess barriers/facilitators to standards use (meeting the standards), select, tailor and activate implementation strategies (action plan), monitor standards use and evaluate outcomes | - Organizations use this standard to conduct self-assessments across acute care units (e.g. emergency department, critical care, etc.), typically a year before an on-site survey visit although they are encouraged to self-assess on a more regular schedule as well, e.g. carriage return annually. -The self-assessment results are used by organizations to identify areas for improvement and provide the foundation to collaboratively develop an action plan. -Accredited organizations are required to conduct surveys using instruments (e.g. patient experience, governance, patient safety culture, worklife ‘pulse’ assessment of the environment for staff and physicians). -Self-assessments and surveys are completed using a secure online client portal that allows the client organization to view the standard criterion, guidance, survey instruments and their results. -The accreditation process encourages formal self-assessment as well as third-party assessment of facilitators and barriers organizations may experience in their effort to meet the standards. It allows organizations to have a clear understanding of how well they meet each criterion within a standard and to monitor trends over time. | -All accredited organizations undertake self-assessment via online self-assessment software. This self-assessment process using AccreditationPro enables the active involvement of individual staff or teams, engaging the whole organization in the self-assessment process and preparation for accreditation. -Each indicator or criterion is rated as ‘met’ or ‘not met’. If rated as ‘not met’, the client organizations can then develop an action plan for that specific indicator which includes: • The action that needs to occur • Progress notes • Person responsible • Due date • Completion -Outstanding actions or improvements must be completed before the self-assessment can be submitted. The self-assessment process via AccreditationPro cannot be submitted until all indicators/criteria have been rated as met. This forcing factor ensures that client organizations address each indicator. If any indicators are rated as ‘not met’, the client organization is directed to complete all indicators as met before the self-assessment can be submitted. When a client organization rates an indicator a ‘not met’, they commence an action plan for that indicator. Not until all actions within the action plan have been completed can the client organization confirm that the indicator has now been ‘met’ and submission of AccreditationPro is then able to occur. |
| -The results of accredited organizations’ survey data and their respective action plans are reviewed by the survey team and discussed as part of the on-site visit. For example, poor results on a patient experience survey may lead to a further inquiry on the processes used for patient and family engagement, staff and physician training and assessment of patient/family advisory committees. Furthermore, the assessment team would explore what interventions the accredited organization has implemented to address the results and evaluate progress made. This helps to inform whether accredited organizations are successfully meeting the standards. -Accreditation Canada offers education and training aligned to these standards to support client organizations. -Upon conclusion of the on-site assessment, the surveyor team recommends an accreditation decision based on results, assessment of risk and accreditation decision guidelines. Surveyor inputs and observations are vital components. -Survey instrument data and respective action plans are reviewed by the survey team and discussed as part of the on-site visit. -Client organizations may submit relevant information (e.g. evidence that demonstrate a criterion is being met) in advance of an on-site visit. One medication management example is ‘The interdisciplinary committee has defined roles and responsibilities for medication management that are in line with legislation and applicable regulations’. carriage return -The process of assessment includes evaluation against each standard criterion. For example, with medication management, the surveyors would seek evidence that ‘Pharmacists collaborate with clients and interprofessional clinical teams to provide care using evidence-informed care activities associated with improved client and system outcomes’. -Surveyor qualification typically includes practicing physicians, nurses, therapists, pharmacists and administrators with a demonstrated experience in quality and safety. Since 2019 patient surveyors have been incorporated into the surveyor teams. Patient surveyors focus on people-centered care criteria. Surveyors use a combination of methods to assess medication management criteria (e.g. direct observation, patient and provider interviews, chart review, etc.). -The on-site assessment enables a review of the evidence that the standards have been achieved and/or where gaps are identified as noted in performance measures such as medication error rates and evidence of collaboration. -Upon conclusion of the on-site assessment, the surveyor team recommends an accreditation decision based on results, assessment of risk and accreditation decision guidelines. | -To support the selection, tailoring and development of the action plan, client organizations assess/identify any barriers or knowledge needed in order to meet the standards. AccreditationPro includes a resource library that consists of a variety of resources including direct links to external websites, policies, procedures and templates to assist client organizations to reduce any barriers that they may find in meeting the requirements of the standards. Each resource can be linked directly to the specific indicator/criteria within AccreditationPro which provides the client organization with instant access to resources to support them in meeting the indicators/standards. -AGPAL provides a direct support for the implementation interventions/strategies by offering education and training to client organizations to assist them to overcome knowledge barriers related to the standards or processes required to meet the standards. The types of education and training activities range from face-to-face workshops, webinars and online modules. -Throughout the on-site survey, surveyors/assessors rate compliance with the standards. Findings are collated into a final report, and these data are intended to assist organizations identify where further improvement is required. -AGPAL requires the collection of outcomes related to the use of the standards. The use of the NSQHS Standards have the following outcomes: • Decreased rates of healthcare-associated infections. • Decreased in-hospital cardiac arrests. • Increased documentation of adverse drug reactions and medication histories. • Decreased prescribing of antibiotics due to improvements in antibiotic stewardship. -The AGPAL decision-making framework states decisions will be timely and made within a fair and transparent decision-making framework. The client organization has the opportunity to respond to the draft before the final accreditation decision. -The principles of decision-making incorporate natural justice, transparency and independence (no conflict of interest and impartiality). -Decision process: Decision-makers rely substantially on the information supplied by the assessment team including the assessment report, assessor comments, the corrective actions taken by the client organization and the accredited organization’s assessment history. -Accreditation report: The accreditation report is provided to the client organization within specified timeframes with the expectation that it will be used to continue to make necessary improvements and maintain the improvements made. | |
| -The final accreditation decision is conferred by an independent body, the Accreditation Decision Committee (ADC). They review results, summarize findings and prepare a report within 3 weeks of the on-site assessment. -Organizations that successfully complete the Accreditation Canada Qmentum program are issued an accreditation award and are eligible to receive the Accreditation Canada banner and seal. -Organizations that are unsuccessful in their accreditation may undergo a supplementary survey within 5 months of the original ADC decision. | ||
| Sustain standards use | - To ensure continuous quality improvement, Accreditation Canada is evolving assessments to sequential assessments, whereby organizations and health systems receive targeted surveys on fewer standards every 18–24 months. -Client organizations are encouraged to submit to HSO’s https://healthstandards.org/leading-practices/, a good example of how the program enables the spread of evidence-based practice and innovations across the country. A leading practice is a practice carried out by a health and/or social service organization that has demonstrated a positive change and is people-centered, safe and efficient. This further reinforces quality improvement and recognizes organizations and health systems. -Accreditation Canada offers ongoing education and training aligned to standards to support client organizations. | -All the follow-up mechanisms provide ongoing maintenance of an accredited organization’s progress against the standards and assist them in preparing for the next accreditation cycle, i.e. supports ongoing standard implementation and maintenance via continuous self- evaluation. The follow-up mechanisms include annual and mid-cycle quality improvement plans, mid-cycle on-site assessment, short notice assessment and ongoing support including online resources, webinars, face-to-face training and newsletters. -AGPAL’s ongoing provision of education and training for client organizations also contributes to sustaining of the standards. -Twelve months prior to accredited organizations’ accreditation expiry, contacts via email and phone calls are made with client organizations at 3-month intervals to assist accredited organizations with preparation for their next accreditation survey. |
| Knowledge to action component . | Illustrative example from the Accreditation Canada Qmentum Program [The medication management standard is used as an example]: carriage return www.accreditation.ca Accreditation Canada is a not-for-profit organization established in the 1950s as a provider of health services accreditation. Clients include healthcare organizations across the continuum from home and community to acute care and palliative care. . | Illustrative example from the AGPAL Accreditation Organization applying the National Safety and Quality Health Service (NSQHS) Standards www.agpal.com.au Australian General Practice Accreditation Limited (AGPAL) is a leading not-for-profit organization, established in 1997 as a provider for general practice accreditation and quality improvement services within Australia. . |
|---|---|---|
| Knowledge/standards creation | ||
| Knowledge/standards, products/tools | -Based on the best evidence and input from patients, providers, product users, researchers and policymakers, the medication management standard for acute care organizations specifies organizational-level requirements that prevent and reduce patient safety incidents involving medications carriage return.—The standard addresses all aspects of the medication management process (e.g. ‘ensuring the people managing medications are educated and competent; managing client and medication information’).—The standard incorporates required (mandatory) organizational practices (ROPs) such as antimicrobial stewardship and medication reconciliation to ensure evidence-based practices are embedded in care delivery.—The standards are regularly reviewed, and where needed based on changes in evidence, revised every 5 years to remain relevant and applicable. | -The NSQHS Standards have numerous requirements for health services to be consistent with evidence-based practices including: 5.13 Clinicians use processes for shared decision-making to develop and document a comprehensive and individualized plan that: f. Is consistent with best practice and evidence -As standards are developed, the evidence required for each indicator is determined and from where this evidence can be obtained, e.g. document review, interview or observation. -The NSQHS Standards are owned by the Australian Commission on Safety and Quality in Health Care. The Commission has a process for keeping the standards up to date with the emerging evidence. The Commission also has a ‘live literature searches’ function on their website that can be used to find evidence to support best practice in line with the NSQHS Standards. The Commission provides accrediting agencies with NSQHS Standards Advisories as a formal communication from the Commission to provide guidance and direction on the interpretation and/or assessment of the NSQHS Standards. The NSQHS Standards advisories are routinely reviewed to ensure they remain current and supported by available evidence. |
| Action cycle | ||
| Elements include: determine the standards/practice–achievement gap, customize operationalization of standards to the local context, assess barriers/facilitators to standards use (meeting the standards), select, tailor and activate implementation strategies (action plan), monitor standards use and evaluate outcomes | - Organizations use this standard to conduct self-assessments across acute care units (e.g. emergency department, critical care, etc.), typically a year before an on-site survey visit although they are encouraged to self-assess on a more regular schedule as well, e.g. carriage return annually. -The self-assessment results are used by organizations to identify areas for improvement and provide the foundation to collaboratively develop an action plan. -Accredited organizations are required to conduct surveys using instruments (e.g. patient experience, governance, patient safety culture, worklife ‘pulse’ assessment of the environment for staff and physicians). -Self-assessments and surveys are completed using a secure online client portal that allows the client organization to view the standard criterion, guidance, survey instruments and their results. -The accreditation process encourages formal self-assessment as well as third-party assessment of facilitators and barriers organizations may experience in their effort to meet the standards. It allows organizations to have a clear understanding of how well they meet each criterion within a standard and to monitor trends over time. | -All accredited organizations undertake self-assessment via online self-assessment software. This self-assessment process using AccreditationPro enables the active involvement of individual staff or teams, engaging the whole organization in the self-assessment process and preparation for accreditation. -Each indicator or criterion is rated as ‘met’ or ‘not met’. If rated as ‘not met’, the client organizations can then develop an action plan for that specific indicator which includes: • The action that needs to occur • Progress notes • Person responsible • Due date • Completion -Outstanding actions or improvements must be completed before the self-assessment can be submitted. The self-assessment process via AccreditationPro cannot be submitted until all indicators/criteria have been rated as met. This forcing factor ensures that client organizations address each indicator. If any indicators are rated as ‘not met’, the client organization is directed to complete all indicators as met before the self-assessment can be submitted. When a client organization rates an indicator a ‘not met’, they commence an action plan for that indicator. Not until all actions within the action plan have been completed can the client organization confirm that the indicator has now been ‘met’ and submission of AccreditationPro is then able to occur. |
| -The results of accredited organizations’ survey data and their respective action plans are reviewed by the survey team and discussed as part of the on-site visit. For example, poor results on a patient experience survey may lead to a further inquiry on the processes used for patient and family engagement, staff and physician training and assessment of patient/family advisory committees. Furthermore, the assessment team would explore what interventions the accredited organization has implemented to address the results and evaluate progress made. This helps to inform whether accredited organizations are successfully meeting the standards. -Accreditation Canada offers education and training aligned to these standards to support client organizations. -Upon conclusion of the on-site assessment, the surveyor team recommends an accreditation decision based on results, assessment of risk and accreditation decision guidelines. Surveyor inputs and observations are vital components. -Survey instrument data and respective action plans are reviewed by the survey team and discussed as part of the on-site visit. -Client organizations may submit relevant information (e.g. evidence that demonstrate a criterion is being met) in advance of an on-site visit. One medication management example is ‘The interdisciplinary committee has defined roles and responsibilities for medication management that are in line with legislation and applicable regulations’. carriage return -The process of assessment includes evaluation against each standard criterion. For example, with medication management, the surveyors would seek evidence that ‘Pharmacists collaborate with clients and interprofessional clinical teams to provide care using evidence-informed care activities associated with improved client and system outcomes’. -Surveyor qualification typically includes practicing physicians, nurses, therapists, pharmacists and administrators with a demonstrated experience in quality and safety. Since 2019 patient surveyors have been incorporated into the surveyor teams. Patient surveyors focus on people-centered care criteria. Surveyors use a combination of methods to assess medication management criteria (e.g. direct observation, patient and provider interviews, chart review, etc.). -The on-site assessment enables a review of the evidence that the standards have been achieved and/or where gaps are identified as noted in performance measures such as medication error rates and evidence of collaboration. -Upon conclusion of the on-site assessment, the surveyor team recommends an accreditation decision based on results, assessment of risk and accreditation decision guidelines. | -To support the selection, tailoring and development of the action plan, client organizations assess/identify any barriers or knowledge needed in order to meet the standards. AccreditationPro includes a resource library that consists of a variety of resources including direct links to external websites, policies, procedures and templates to assist client organizations to reduce any barriers that they may find in meeting the requirements of the standards. Each resource can be linked directly to the specific indicator/criteria within AccreditationPro which provides the client organization with instant access to resources to support them in meeting the indicators/standards. -AGPAL provides a direct support for the implementation interventions/strategies by offering education and training to client organizations to assist them to overcome knowledge barriers related to the standards or processes required to meet the standards. The types of education and training activities range from face-to-face workshops, webinars and online modules. -Throughout the on-site survey, surveyors/assessors rate compliance with the standards. Findings are collated into a final report, and these data are intended to assist organizations identify where further improvement is required. -AGPAL requires the collection of outcomes related to the use of the standards. The use of the NSQHS Standards have the following outcomes: • Decreased rates of healthcare-associated infections. • Decreased in-hospital cardiac arrests. • Increased documentation of adverse drug reactions and medication histories. • Decreased prescribing of antibiotics due to improvements in antibiotic stewardship. -The AGPAL decision-making framework states decisions will be timely and made within a fair and transparent decision-making framework. The client organization has the opportunity to respond to the draft before the final accreditation decision. -The principles of decision-making incorporate natural justice, transparency and independence (no conflict of interest and impartiality). -Decision process: Decision-makers rely substantially on the information supplied by the assessment team including the assessment report, assessor comments, the corrective actions taken by the client organization and the accredited organization’s assessment history. -Accreditation report: The accreditation report is provided to the client organization within specified timeframes with the expectation that it will be used to continue to make necessary improvements and maintain the improvements made. | |
| -The final accreditation decision is conferred by an independent body, the Accreditation Decision Committee (ADC). They review results, summarize findings and prepare a report within 3 weeks of the on-site assessment. -Organizations that successfully complete the Accreditation Canada Qmentum program are issued an accreditation award and are eligible to receive the Accreditation Canada banner and seal. -Organizations that are unsuccessful in their accreditation may undergo a supplementary survey within 5 months of the original ADC decision. | ||
| Sustain standards use | - To ensure continuous quality improvement, Accreditation Canada is evolving assessments to sequential assessments, whereby organizations and health systems receive targeted surveys on fewer standards every 18–24 months. -Client organizations are encouraged to submit to HSO’s https://healthstandards.org/leading-practices/, a good example of how the program enables the spread of evidence-based practice and innovations across the country. A leading practice is a practice carried out by a health and/or social service organization that has demonstrated a positive change and is people-centered, safe and efficient. This further reinforces quality improvement and recognizes organizations and health systems. -Accreditation Canada offers ongoing education and training aligned to standards to support client organizations. | -All the follow-up mechanisms provide ongoing maintenance of an accredited organization’s progress against the standards and assist them in preparing for the next accreditation cycle, i.e. supports ongoing standard implementation and maintenance via continuous self- evaluation. The follow-up mechanisms include annual and mid-cycle quality improvement plans, mid-cycle on-site assessment, short notice assessment and ongoing support including online resources, webinars, face-to-face training and newsletters. -AGPAL’s ongoing provision of education and training for client organizations also contributes to sustaining of the standards. -Twelve months prior to accredited organizations’ accreditation expiry, contacts via email and phone calls are made with client organizations at 3-month intervals to assist accredited organizations with preparation for their next accreditation survey. |
References
More About Knowledge Translation at CIHR. Canadian Institutes of Health Research, Government of Canada. http://www.cihr-irsc.gc.ca



