-
PDF
- Split View
-
Views
-
Cite
Cite
Mette Løkeland, Tone Bjørge, Ole-Erik Iversen, Rupali Akerkar, Line Bjørge, Implementing medical abortion with mifepristone and misoprostol in Norway 1998–2013, International Journal of Epidemiology, Volume 46, Issue 2, April 2017, Pages 643–651, https://doi.org/10.1093/ije/dyw270
Close - Share Icon Share
Abstract
Background: Medical abortion with mifepristone and misoprostol was introduced in Norway in 1998, and since then there has been an almost complete change from predominantly surgical to medical abortions. We aimed to describe the medical abortion implementation process, and to compare characteristics of women obtaining medical and surgical abortion.
Methods: Information from all departments of obstetrics and gynaecology in Norway on the time of implementation of medical abortion and abortion procedures in use up to 12 weeks of gestation was assessed by surveys in 2008 and 2012. We also analysed data from the National Abortion Registry comprising 223 692 women requesting abortion up to 12 weeks of gestation during 1998–2013.
Results: In 2012, all hospitals offered medical abortion, 84.4% offered medical abortion at 9–12 weeks of gestation and 92.1% offered home administration of misoprostol. The use of medical abortion increased from 5.9% of all abortions in 1998 to 82.1% in 2013. Compared with women having a surgical abortion, women obtaining medical abortion had higher odds for undergoing an abortion at 4–6 weeks (adjusted OR 2.33; 95% confidence interval 2.28-2.38). Waiting time between registered request for an abortion until termination was reduced from 11.3 days in 1998 to 7.3 days in 2013.
Conclusions: Norwegian women have gained access to more treatment modalities and simplified protocols for medical abortion. At the same time they obtained abortions at an earlier gestational age and the waiting time has been reduced.
Introduction
Termination of pregnancy is one of the most common procedures in reproductive health. At the same time it is one of the more controversial and politically contentious procedures in medicine.1 The abortion rate in the world is declining, but the proportion of unsafe abortions is increasing.2 In Norway the abortion rate has been relatively stable, ranging from 12.5–14.5 per 1000 women aged 15–49 between 1995 and 2013 (14).3 Misoprostol used for clandestine abortions is associated with lower risk of maternal mortality and morbidity than unsafe surgical abortions, but there is a lack of knowledge about the correct use for pregnancy termination.2 Increased knowledge and the combined use of mifepristone and misoprostol could help reduce maternal deaths, particularly in areas with limited numbers of health professionals and low access to health services in both legal and illegal settings.
Norway began offering medical abortion with mifepristone and misoprostol in 1998. Due to a dispute in Parliament over a planned clinical trial of mifepristone in 1989 (Figure 1), the pharmaceutical company producing mifepristone withdrew their application to register mifepristone in Norway.4 In 1998, mifepristone was introduced in Norway as a drug with exemption from registration. Mifepristone was registered for use in Norway in 2001.5 Norway has a public health system and every department of obstetrics and gynaecology in the country is obliged to perform abortions completely free of charge. Only physicians are entitled to perform abortions, but delegation to other health professionals under supervision is not prohibited.6 Doctors always undertake surgical abortions, whereas medical abortions very often are allocated to nurses. No abortions are performed outside the public health system.
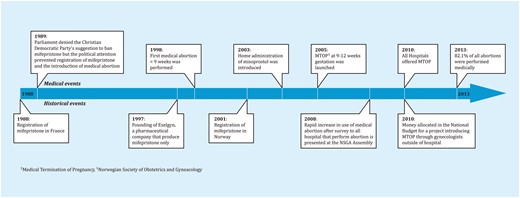
Historical timeline of the implementation of medical abortion in Norway.
Since the registration of mifepristone in France in 1988, medical abortion with mifepristone and misoprostol has been available, is thoroughly documented for use up to 9 weeks of gestation and was in 2016 approved for use up to 70 days by the US Food and Drug Administration.7,8 Over the past 25 years, the treatment procedures have been modified and introduced for use in both late first trimester and second trimester abortions, and it has become available in a growing number of countries.9–11 Medical abortion requires fewer human and economic resources and can be more cost-effective than surgical abortion, especially if the number of visits for treatment and follow-up are reduced.12,13 Medical abortion was included in the Norwegian national guidelines for abortion treatment up to 9 weeks of gestation in 2004. The recommended treatment protocol was 200–600 mg mifepristone, admission to hospital and administration of 800 µg misoprostol after 42–48 h.14 In 2009, the guidelines were altered to recommend self-administration of misoprostol vaginally at home and to extend the gestational limit of medical abortion from 9 to 12 weeks of gestation.15
Some critics have feared that increased access to medical abortion would increase the number of abortions.4
From the introduction of medical abortion with mifepristone and misoprostol in Norway, there has been an almost complete change in abortion procedures from close to 100% surgical abortions in 1997 to 82.1% of all abortions being performed medically in 2013.3 Approximately 95% of all abortions are performed within 12 weeks of gestation.3 There is some knowledge on why some women prefer medical abortion whereas others opt for surgical abortion,16 but little is known about possible differences in characteristics between these two populations in Norway.
This study describes the implementation process of medical abortion in Norway over the first 15 years after the introduction in 1998 (Figure 1) and the current abortion practice at Norwegian hospitals based on a facility survey sent to all hospitals providing abortion services at the two time points, 2008 and 2012. Data from the Abortion Registry are used to describe the proportion of abortions that were undertaken medically or surgically from 1998 to 2013 and to compare the characteristics of women who chose medical versus surgical abortions. We also evaluated if the almost complete change in abortion practices influenced the waiting time from request for an abortion until termination.
Methods
Study design and material
First, this is a review of the practice and implementation of medical abortion in Norway through a survey sent to all hospitals offering termination of pregnancy at two time points, in 2008 and 2012. Second, it is a study of 223 692 women in the Abortion Registry who requested abortion and terminated a pregnancy up to 12 weeks of gestation in the years 1998 to 2013.
Hospital surveys
In 2008, a questionnaire was elaborated by the research group and sent by mail to all 40 departments of obstetrics and gynaecology performing abortions in Norway [helseadresser.no] with the purpose of mapping the prevalence and distribution of medical abortion and treatment protocols. The survey was repeated in 2012 after a rapid increase in medical abortion was reported by the Abortion Registry.3 Due to merging of closely located clinics, the number of hospitals was reduced to 38. Information about the existing treatment portfolio was obtained through the questions: do you offer medical abortion up to 9 weeks of gestation, medical abortion with home administration of misoprostol, and medical abortion between 9 to 12 weeks of gestation; and in which years were the different treatment options introduced. In addition, dosages of mifepristone (200 mg, 400 mg, or 600 mg), route of administration of misoprostol (oral or vaginal), and follow-up regimen used ([serum-human chorionic gonadotropin (s-hCG); urine-hCG; ultrasound/clinical or no control] were requested.
Abortion Registry
The Abortion Registry was established in 1979 and is a population-based, de-identified registry. Data are recorded in a standard form using check boxes with specific alternatives, at the hospital performing the abortion, and are then sent to the registry. The woman’s name and personal identification number are removed before the form leaves the hospital. Hence, it is not possible to link the registry to other health registries nor to follow one particular woman’s abortion history.
The following variables in the Abortion Registry were available for this study: year of termination, year of birth, age, marital status (married, cohabiting, single, divorced/widowed, not registered); employment status (full-time and studying, full-time, part-time and studying, part-time and applying for jobs, part-time and on social welfare, part-time, student, unemployed, social welfare, other); educational level (primary, secondary, college/university, other); previous pregnancies; number of children; previous terminations; date of registered request for abortion and method used (medical, surgical).
The standard abortion form has changed three times during this time period, in 1995, 1999 and 2006. Medical abortion as a specific method of termination was first included in 2006. In the forms used before 2006, one could register ‘injection of abortifacient’ or ‘local application of prostaglandin’. For data collected before 2006, the registry has defined medical abortion as the use of one of these methods, and at the same time the absence of surgery. Information on educational level was also first introduced in 2006. Information on whether misoprostol has been administered in hospital or outside hospital, mifepristone dosage, route of administration of misoprostol and control regimen are not included in the form.
A total of 311 (0.1%) women lacked information on method and were excluded from the analyses of medical and surgical abortion. Data with extreme measures were excluded from the analyses: gestational age below 4 weeks of gestation (342); number of previously born children higher than 12 (3); women older than 54 years (2); and number of previous abortions above 12 (11). Abortions on request that were undergone after 12 weeks of gestation were also excluded.
Statistical analyses
All abortions were subdivided and compared according to method used (medical, surgical). Frequencies, univariate and multivariate logistic regression analyses were used to compare medical and surgical abortions, according to characteristics of the study population (woman’s age, gestational age, previous abortions, parity, level of education, occupational status and marital status). We adjusted for woman's age, gestational age and year of the abortion in multivariable logistic regressions comparing characteristics of women undergoing medical versus surgical abortions. The analyses were performed using Statistical Package for Social Sciences 20 (SPSS) and R.
Ethical approval
The Committee for Medical and Health Research Ethics, Western Norway (number 2009/738) and the Norwegian Social Science Data Services (number 34010) approved the study.
Results
Hospital surveys
Response rates for the two surveys, performed in 2008 and 2012, were both 100%. The surveys revealed an increase in the percentage of hospitals in Norway offering medical abortion, from nil in 1997 to 50% in 2001 and 100% in 2010. In 2012, a total of 84.4% offered medical abortion at 9–12 weeks of gestation and 92.1% of all hospitals offered home administration of misoprostol (Figure 2). Table 1 demonstrates the different treatment practices in the country. The most frequent mifepristone dosage administered was 200 mg (83.3% in 2008 and 94.7% in 2012). Two (5.3%) hospitals chose 400 mg of mifepristone for their medical abortions and one (3.0%) hospital used 600 mg for medical abortion at 9–12 weeks of gestation in 2012. The vaginal route was the most common administration method for misoprostol both in 2008 (85.7%) and in 2012 (94.2%). For home use of misoprostol, the oral route was chosen by 14.3% of the hospitals in 2012. The use of u-hCG as follow-up procedure increased between 2008 and 2012, and was in 2012 the most frequently used method (45.5-51.4%), dependent on protocol.

Percentage of hospitals offering medical abortion treatments in 1998-2012. Based on data from the 2012 survey.
Description of treatment methods for medical abortion in Norway, 2008 and 2012
| . | Up to 63 days of gestation in hospital . | Home administration of misoprostol up to 63 days of gestation . | 9-12 weeks of gestation in hospital . | |||
|---|---|---|---|---|---|---|
| Clinics providing abortion . | 2008 . | 2012 . | 2008 . | 2012 . | 2008 . | 2012 . |
| N = 40 (%) . | N = 38 (%) . | N = 40 (%) . | N = 38 (%) . | N = 40 (%) . | N = 38 (%) . | |
| Clinics offering medical abortion | 36 (90) | 38 (100) | 9 (22.5) | 35 (92.1) | 7 (17.5) | 32 (84.2) |
| missing | 0 | 0 | 0 | 0 | 0 | 2 |
| Mifepristone dose | 36 | 38 | 9 | 35 | 7 | 33 |
| 200 mg | 30 (83.3) | 36 (94.7) | 8 (88.9) | 33 (94.2) | 7 (100) | 31 (93.9) |
| 400 mg | 2 (5.6) | 2 (5.3) | 1 (11.1) | 2 (5.8) | 0 | 1 (3.0) |
| 600 mg | 4 (11.1) | 0 | 0 | 0 | 0 | 1 (3.0) |
| missing | 0 | 0 | 0 | 0 | 0 | 5 |
| Misoprostol route of administration | 34 | 38 | 8 | 35 | 7 | 32 |
| vaginal | 32 (94.1) | 32 (94.2) | 8 (100) | 30 (85.7) | 7 (100) | 29 (90.6) |
| oral | 2 (5.9) | 6 (5.8) | 0 | 5 (14.3) | 0 | 3 (9.4) |
| missing | 2 | 0 | 1 | 0 | 0 | 0 |
| Control regimen | 35 | 38 | 9 | 35 | 6 | 33 |
| u-hCG | 10 (28.6) | 19 (50.0) | 3 (33.3) | 18 (51.4) | 3 (50.0) | 15 (45.5) |
| s-hCG | 9 (25.7) | 13 (34.2) | 5 (55.6) | 13 (37.1) | 2 (33.3) | 9 (27.3) |
| ultrasound | 12 (34.3) | 4 (10.5) | 1 (11.1) | 2 (5.7) | 1 (17.7) | 9 (27.3) |
| no control | 4 (11·4) | 2 (5·3) | 0 | 2 (5·7) | 0 | 0 |
| missing | 1 | 0 | 0 | 0 | 1 | 5 |
| . | Up to 63 days of gestation in hospital . | Home administration of misoprostol up to 63 days of gestation . | 9-12 weeks of gestation in hospital . | |||
|---|---|---|---|---|---|---|
| Clinics providing abortion . | 2008 . | 2012 . | 2008 . | 2012 . | 2008 . | 2012 . |
| N = 40 (%) . | N = 38 (%) . | N = 40 (%) . | N = 38 (%) . | N = 40 (%) . | N = 38 (%) . | |
| Clinics offering medical abortion | 36 (90) | 38 (100) | 9 (22.5) | 35 (92.1) | 7 (17.5) | 32 (84.2) |
| missing | 0 | 0 | 0 | 0 | 0 | 2 |
| Mifepristone dose | 36 | 38 | 9 | 35 | 7 | 33 |
| 200 mg | 30 (83.3) | 36 (94.7) | 8 (88.9) | 33 (94.2) | 7 (100) | 31 (93.9) |
| 400 mg | 2 (5.6) | 2 (5.3) | 1 (11.1) | 2 (5.8) | 0 | 1 (3.0) |
| 600 mg | 4 (11.1) | 0 | 0 | 0 | 0 | 1 (3.0) |
| missing | 0 | 0 | 0 | 0 | 0 | 5 |
| Misoprostol route of administration | 34 | 38 | 8 | 35 | 7 | 32 |
| vaginal | 32 (94.1) | 32 (94.2) | 8 (100) | 30 (85.7) | 7 (100) | 29 (90.6) |
| oral | 2 (5.9) | 6 (5.8) | 0 | 5 (14.3) | 0 | 3 (9.4) |
| missing | 2 | 0 | 1 | 0 | 0 | 0 |
| Control regimen | 35 | 38 | 9 | 35 | 6 | 33 |
| u-hCG | 10 (28.6) | 19 (50.0) | 3 (33.3) | 18 (51.4) | 3 (50.0) | 15 (45.5) |
| s-hCG | 9 (25.7) | 13 (34.2) | 5 (55.6) | 13 (37.1) | 2 (33.3) | 9 (27.3) |
| ultrasound | 12 (34.3) | 4 (10.5) | 1 (11.1) | 2 (5.7) | 1 (17.7) | 9 (27.3) |
| no control | 4 (11·4) | 2 (5·3) | 0 | 2 (5·7) | 0 | 0 |
| missing | 1 | 0 | 0 | 0 | 1 | 5 |
Description of treatment methods for medical abortion in Norway, 2008 and 2012
| . | Up to 63 days of gestation in hospital . | Home administration of misoprostol up to 63 days of gestation . | 9-12 weeks of gestation in hospital . | |||
|---|---|---|---|---|---|---|
| Clinics providing abortion . | 2008 . | 2012 . | 2008 . | 2012 . | 2008 . | 2012 . |
| N = 40 (%) . | N = 38 (%) . | N = 40 (%) . | N = 38 (%) . | N = 40 (%) . | N = 38 (%) . | |
| Clinics offering medical abortion | 36 (90) | 38 (100) | 9 (22.5) | 35 (92.1) | 7 (17.5) | 32 (84.2) |
| missing | 0 | 0 | 0 | 0 | 0 | 2 |
| Mifepristone dose | 36 | 38 | 9 | 35 | 7 | 33 |
| 200 mg | 30 (83.3) | 36 (94.7) | 8 (88.9) | 33 (94.2) | 7 (100) | 31 (93.9) |
| 400 mg | 2 (5.6) | 2 (5.3) | 1 (11.1) | 2 (5.8) | 0 | 1 (3.0) |
| 600 mg | 4 (11.1) | 0 | 0 | 0 | 0 | 1 (3.0) |
| missing | 0 | 0 | 0 | 0 | 0 | 5 |
| Misoprostol route of administration | 34 | 38 | 8 | 35 | 7 | 32 |
| vaginal | 32 (94.1) | 32 (94.2) | 8 (100) | 30 (85.7) | 7 (100) | 29 (90.6) |
| oral | 2 (5.9) | 6 (5.8) | 0 | 5 (14.3) | 0 | 3 (9.4) |
| missing | 2 | 0 | 1 | 0 | 0 | 0 |
| Control regimen | 35 | 38 | 9 | 35 | 6 | 33 |
| u-hCG | 10 (28.6) | 19 (50.0) | 3 (33.3) | 18 (51.4) | 3 (50.0) | 15 (45.5) |
| s-hCG | 9 (25.7) | 13 (34.2) | 5 (55.6) | 13 (37.1) | 2 (33.3) | 9 (27.3) |
| ultrasound | 12 (34.3) | 4 (10.5) | 1 (11.1) | 2 (5.7) | 1 (17.7) | 9 (27.3) |
| no control | 4 (11·4) | 2 (5·3) | 0 | 2 (5·7) | 0 | 0 |
| missing | 1 | 0 | 0 | 0 | 1 | 5 |
| . | Up to 63 days of gestation in hospital . | Home administration of misoprostol up to 63 days of gestation . | 9-12 weeks of gestation in hospital . | |||
|---|---|---|---|---|---|---|
| Clinics providing abortion . | 2008 . | 2012 . | 2008 . | 2012 . | 2008 . | 2012 . |
| N = 40 (%) . | N = 38 (%) . | N = 40 (%) . | N = 38 (%) . | N = 40 (%) . | N = 38 (%) . | |
| Clinics offering medical abortion | 36 (90) | 38 (100) | 9 (22.5) | 35 (92.1) | 7 (17.5) | 32 (84.2) |
| missing | 0 | 0 | 0 | 0 | 0 | 2 |
| Mifepristone dose | 36 | 38 | 9 | 35 | 7 | 33 |
| 200 mg | 30 (83.3) | 36 (94.7) | 8 (88.9) | 33 (94.2) | 7 (100) | 31 (93.9) |
| 400 mg | 2 (5.6) | 2 (5.3) | 1 (11.1) | 2 (5.8) | 0 | 1 (3.0) |
| 600 mg | 4 (11.1) | 0 | 0 | 0 | 0 | 1 (3.0) |
| missing | 0 | 0 | 0 | 0 | 0 | 5 |
| Misoprostol route of administration | 34 | 38 | 8 | 35 | 7 | 32 |
| vaginal | 32 (94.1) | 32 (94.2) | 8 (100) | 30 (85.7) | 7 (100) | 29 (90.6) |
| oral | 2 (5.9) | 6 (5.8) | 0 | 5 (14.3) | 0 | 3 (9.4) |
| missing | 2 | 0 | 1 | 0 | 0 | 0 |
| Control regimen | 35 | 38 | 9 | 35 | 6 | 33 |
| u-hCG | 10 (28.6) | 19 (50.0) | 3 (33.3) | 18 (51.4) | 3 (50.0) | 15 (45.5) |
| s-hCG | 9 (25.7) | 13 (34.2) | 5 (55.6) | 13 (37.1) | 2 (33.3) | 9 (27.3) |
| ultrasound | 12 (34.3) | 4 (10.5) | 1 (11.1) | 2 (5.7) | 1 (17.7) | 9 (27.3) |
| no control | 4 (11·4) | 2 (5·3) | 0 | 2 (5·7) | 0 | 0 |
| missing | 1 | 0 | 0 | 0 | 1 | 5 |
Abortion Registry
The percentage of abortions performed medically with mifepristone and misoprostol increased from 5.9% of all abortions in 1998 to 82.1% in 2013 (Figure 3), and the percentage of all abortions undertaken within 9 weeks of gestation increased from 44.0% in 1998 to 77.8% in 2013. The percentage of requests for an abortion that ended in a termination decreased steadily from 92.3% in 1998 to 88.5% in 2013.

Percentage of medical and surgical abortions 1998-2013, based on 223 692 abortions.
A comparison of medical and surgical abortion according to characteristics of the study population is shown in Table 2. There was a higher number of women using a medical approach to a termination under 7 weeks of gestation than women having a surgical abortion [adjusted odds ratio (OR) 2.11; 95% confidence interval (CI) 2.06-2.16), and a slightly reduced likelihood of undergoing a medical abortion among women with previous abortion experience (adjusted OR 0.87; 95% CI 0.85-0.90). The odds for undergoing a medical procedure in comparison with surgery increased with increasing level of education and decreased with increasing parity (Table 2). There were no differences in age, occupational or marital status between the two groups.
Frequencies, crude and adjusted odds ratios (ORs) of medical in comparison with surgical abortion according to characteristics of the study population: 223 692 women requesting abortion up to 12 weeks of gestation in Norway, 1998-20131
| . | Medical (n = 100605) . | Surgical (n = 122776) . | Crude . | Adjusted2 . | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) . | OR (95% CI) . | |||||||
| N . | % . | Median (range) . | N . | % . | Median (range) . | . | . | |
| Age (years) | 26 (12-52) | 26 (12-51) | ||||||
| ≤ 19 | 13596 | 13.5 | 21161 | 17.2 | 0.74 (0.72-0.76) | 0.85 (0.82-0.87) | ||
| 20-24 | 28209 | 28.0 | 32542 | 26.5 | 1.00 Reference | 1.00 Reference | ||
| 25-29 | 22811 | 22.7 | 26259 | 21.4 | 1.00 (0.98-1.03) | 0.99 (0.97-1.02) | ||
| 30-34 | 17744 | 17.6 | 21819 | 17.8 | 0.94 (0.91-0.96) | 0.98 (0.95-1.01) | ||
| 35-39 | 12911 | 12.8 | 15139 | 12.3 | 0.98 (0.96-1.01) | 0.99 (0.96-1.03) | ||
| 40-44 | 4944 | 4.9 | 5336 | 4.3 | 1.07 (1.03-1.11) | 1.00 (0.95-1.05) | ||
| ≥ 45 | 384 | 0.4 | 408 | 0.3 | 1.09 (0.94-1.25) | 0.96 (0.81-1.15) | ||
| Missing | 6 | 0 | 112 | 0.1 | ||||
| Gestational age (weeks) | 7 (4-12) | 8 (4-12) | ||||||
| 4-6 | 41874 | 41.6 | 20522 | 16.7 | 2.34 (2.29-2.39) | 2.11 (2.06-2.16) | ||
| 7-8 | 46682 | 46.4 | 53454 | 43.5 | 1.00 Reference | 1.00 Reference | ||
| 9-10 | 8893 | 8.8 | 36304 | 29.6 | 0.28 (0.27-0.29) | 0.22 (0.22-0.23) | ||
| 11-12 | 2881 | 2.9 | 12429 | 10.1 | 0.27 (0.25-0.28) | 0.19 (0.18-0.20) | ||
| Missing | 275 | 0.3 | 67 | 0 | ||||
| Previous abortions | 0 (0-11) | 0 (0-12) | ||||||
| 0 | 54750 | 54.4 | 55388 | 45.1 | 1.00 Reference | 1.00 Reference | ||
| 1 | 23859 | 23.7 | 29382 | 23.9 | 0.82 (0.80-0.84) | 0.87 (0.85-0.90) | ||
| ≥ 2 | 10771 | 10.7 | 13200 | 10.8 | 0.83 (0.80-0.85) | 0.74 (0.71-0.76) | ||
| Missing | 11225 | 11.2 | 24806 | 20.2 | ||||
| Parity | 1 (0-11) | 1 (0-10) | ||||||
| 0 | 42661 | 42.4 | 44765 | 36.5 | 1.00 Reference | 1.00 Reference | ||
| 1 | 18728 | 18.6 | 23021 | 18.8 | 0.85 (0.83-0.87) | 0.91 (0.88-0.94) | ||
| 2 | 18869 | 18.8 | 22469 | 18.3 | 0.88 (0.86-0.90) | 0.89 (0.86-0.92) | ||
| ≥ 3 | 10555 | 10.5 | 13735 | 11.2 | 0.81 (0.78-0.83) | 0.84 (0.81-0.88) | ||
| Missing | 9792 | 9.7 | 18786 | 15.3 | ||||
| Level of education3 | ||||||||
| Elementary/secondary school | 13001 | 12.9 | 8428 | 6.9 | 0.74 (0.71-0.76) | 0.78 (0.75-0.81) | ||
| High school/upper secondary | 34200 | 34.0 | 16315 | 13.3 | 1.00 Reference | 1.00 Reference | ||
| Collage/universityMissing | 19176 | 19.1 | 7074 | 5.8 | 1.29 (1.25-1.34) | 1.19 (1.15-1.24) | ||
| 34228 | 34.0 | 90959 | 74.1 | |||||
| Occupational status | ||||||||
| Full time | 41499 | 41.2 | 46920 | 38.2 | 1.00 Reference | 1.00 Reference | ||
| Part time | 15413 | 15.3 | 14781 | 12.0 | 1.18 (1.15-1.21) | 1.18 (1.15-1.21) | ||
| Student | 21762 | 21.6 | 28043 | 22.8 | 0.88 (0.86-0.90) | 0.88 (0.86-0.90) | ||
| Out of work | 6352 | 6.3 | 8675 | 7.0 | 0.83 (0.80-0.86) | 0.83 (0.80-0.86) | ||
| Other | 9248 | 9.2 | 17321 | 14.1 | 0.60 (0.59-0.62) | 0.60 (0.59-0.62) | ||
| Missing | 6331 | 6.3 | 7036 | 5.7 | ||||
| Marital status | ||||||||
| Married | 18193 | 18.1 | 23396 | 19.1 | 0.94 (0.92-0.96) | 0.89 (0.86-0.92) | ||
| Cohabiting | 26388 | 26.2 | 28978 | 23.6 | 1.10 (1.07-1.12) | 1.09 (1.07-1.12) | ||
| Single | 47058 | 46.8 | 56667 | 46.2 | 1.00 Reference | 1.00 Reference | ||
| Divorced/widowed | 4270 | 4.2 | 5436 | 4.4 | 0.95 (0.91-0.99) | 0.96 (0.91-1.02) | ||
| Missing | 4696 | 4.7 | 8299 | 6.8 | ||||
| . | Medical (n = 100605) . | Surgical (n = 122776) . | Crude . | Adjusted2 . | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) . | OR (95% CI) . | |||||||
| N . | % . | Median (range) . | N . | % . | Median (range) . | . | . | |
| Age (years) | 26 (12-52) | 26 (12-51) | ||||||
| ≤ 19 | 13596 | 13.5 | 21161 | 17.2 | 0.74 (0.72-0.76) | 0.85 (0.82-0.87) | ||
| 20-24 | 28209 | 28.0 | 32542 | 26.5 | 1.00 Reference | 1.00 Reference | ||
| 25-29 | 22811 | 22.7 | 26259 | 21.4 | 1.00 (0.98-1.03) | 0.99 (0.97-1.02) | ||
| 30-34 | 17744 | 17.6 | 21819 | 17.8 | 0.94 (0.91-0.96) | 0.98 (0.95-1.01) | ||
| 35-39 | 12911 | 12.8 | 15139 | 12.3 | 0.98 (0.96-1.01) | 0.99 (0.96-1.03) | ||
| 40-44 | 4944 | 4.9 | 5336 | 4.3 | 1.07 (1.03-1.11) | 1.00 (0.95-1.05) | ||
| ≥ 45 | 384 | 0.4 | 408 | 0.3 | 1.09 (0.94-1.25) | 0.96 (0.81-1.15) | ||
| Missing | 6 | 0 | 112 | 0.1 | ||||
| Gestational age (weeks) | 7 (4-12) | 8 (4-12) | ||||||
| 4-6 | 41874 | 41.6 | 20522 | 16.7 | 2.34 (2.29-2.39) | 2.11 (2.06-2.16) | ||
| 7-8 | 46682 | 46.4 | 53454 | 43.5 | 1.00 Reference | 1.00 Reference | ||
| 9-10 | 8893 | 8.8 | 36304 | 29.6 | 0.28 (0.27-0.29) | 0.22 (0.22-0.23) | ||
| 11-12 | 2881 | 2.9 | 12429 | 10.1 | 0.27 (0.25-0.28) | 0.19 (0.18-0.20) | ||
| Missing | 275 | 0.3 | 67 | 0 | ||||
| Previous abortions | 0 (0-11) | 0 (0-12) | ||||||
| 0 | 54750 | 54.4 | 55388 | 45.1 | 1.00 Reference | 1.00 Reference | ||
| 1 | 23859 | 23.7 | 29382 | 23.9 | 0.82 (0.80-0.84) | 0.87 (0.85-0.90) | ||
| ≥ 2 | 10771 | 10.7 | 13200 | 10.8 | 0.83 (0.80-0.85) | 0.74 (0.71-0.76) | ||
| Missing | 11225 | 11.2 | 24806 | 20.2 | ||||
| Parity | 1 (0-11) | 1 (0-10) | ||||||
| 0 | 42661 | 42.4 | 44765 | 36.5 | 1.00 Reference | 1.00 Reference | ||
| 1 | 18728 | 18.6 | 23021 | 18.8 | 0.85 (0.83-0.87) | 0.91 (0.88-0.94) | ||
| 2 | 18869 | 18.8 | 22469 | 18.3 | 0.88 (0.86-0.90) | 0.89 (0.86-0.92) | ||
| ≥ 3 | 10555 | 10.5 | 13735 | 11.2 | 0.81 (0.78-0.83) | 0.84 (0.81-0.88) | ||
| Missing | 9792 | 9.7 | 18786 | 15.3 | ||||
| Level of education3 | ||||||||
| Elementary/secondary school | 13001 | 12.9 | 8428 | 6.9 | 0.74 (0.71-0.76) | 0.78 (0.75-0.81) | ||
| High school/upper secondary | 34200 | 34.0 | 16315 | 13.3 | 1.00 Reference | 1.00 Reference | ||
| Collage/universityMissing | 19176 | 19.1 | 7074 | 5.8 | 1.29 (1.25-1.34) | 1.19 (1.15-1.24) | ||
| 34228 | 34.0 | 90959 | 74.1 | |||||
| Occupational status | ||||||||
| Full time | 41499 | 41.2 | 46920 | 38.2 | 1.00 Reference | 1.00 Reference | ||
| Part time | 15413 | 15.3 | 14781 | 12.0 | 1.18 (1.15-1.21) | 1.18 (1.15-1.21) | ||
| Student | 21762 | 21.6 | 28043 | 22.8 | 0.88 (0.86-0.90) | 0.88 (0.86-0.90) | ||
| Out of work | 6352 | 6.3 | 8675 | 7.0 | 0.83 (0.80-0.86) | 0.83 (0.80-0.86) | ||
| Other | 9248 | 9.2 | 17321 | 14.1 | 0.60 (0.59-0.62) | 0.60 (0.59-0.62) | ||
| Missing | 6331 | 6.3 | 7036 | 5.7 | ||||
| Marital status | ||||||||
| Married | 18193 | 18.1 | 23396 | 19.1 | 0.94 (0.92-0.96) | 0.89 (0.86-0.92) | ||
| Cohabiting | 26388 | 26.2 | 28978 | 23.6 | 1.10 (1.07-1.12) | 1.09 (1.07-1.12) | ||
| Single | 47058 | 46.8 | 56667 | 46.2 | 1.00 Reference | 1.00 Reference | ||
| Divorced/widowed | 4270 | 4.2 | 5436 | 4.4 | 0.95 (0.91-0.99) | 0.96 (0.91-1.02) | ||
| Missing | 4696 | 4.7 | 8299 | 6.8 | ||||
A total of 311 (0.1%) of the women had no record of method.
Adjusted for gestational age, the woman’s age and year of the abortion.
Level of education was not registered prior to 2006.
Frequencies, crude and adjusted odds ratios (ORs) of medical in comparison with surgical abortion according to characteristics of the study population: 223 692 women requesting abortion up to 12 weeks of gestation in Norway, 1998-20131
| . | Medical (n = 100605) . | Surgical (n = 122776) . | Crude . | Adjusted2 . | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) . | OR (95% CI) . | |||||||
| N . | % . | Median (range) . | N . | % . | Median (range) . | . | . | |
| Age (years) | 26 (12-52) | 26 (12-51) | ||||||
| ≤ 19 | 13596 | 13.5 | 21161 | 17.2 | 0.74 (0.72-0.76) | 0.85 (0.82-0.87) | ||
| 20-24 | 28209 | 28.0 | 32542 | 26.5 | 1.00 Reference | 1.00 Reference | ||
| 25-29 | 22811 | 22.7 | 26259 | 21.4 | 1.00 (0.98-1.03) | 0.99 (0.97-1.02) | ||
| 30-34 | 17744 | 17.6 | 21819 | 17.8 | 0.94 (0.91-0.96) | 0.98 (0.95-1.01) | ||
| 35-39 | 12911 | 12.8 | 15139 | 12.3 | 0.98 (0.96-1.01) | 0.99 (0.96-1.03) | ||
| 40-44 | 4944 | 4.9 | 5336 | 4.3 | 1.07 (1.03-1.11) | 1.00 (0.95-1.05) | ||
| ≥ 45 | 384 | 0.4 | 408 | 0.3 | 1.09 (0.94-1.25) | 0.96 (0.81-1.15) | ||
| Missing | 6 | 0 | 112 | 0.1 | ||||
| Gestational age (weeks) | 7 (4-12) | 8 (4-12) | ||||||
| 4-6 | 41874 | 41.6 | 20522 | 16.7 | 2.34 (2.29-2.39) | 2.11 (2.06-2.16) | ||
| 7-8 | 46682 | 46.4 | 53454 | 43.5 | 1.00 Reference | 1.00 Reference | ||
| 9-10 | 8893 | 8.8 | 36304 | 29.6 | 0.28 (0.27-0.29) | 0.22 (0.22-0.23) | ||
| 11-12 | 2881 | 2.9 | 12429 | 10.1 | 0.27 (0.25-0.28) | 0.19 (0.18-0.20) | ||
| Missing | 275 | 0.3 | 67 | 0 | ||||
| Previous abortions | 0 (0-11) | 0 (0-12) | ||||||
| 0 | 54750 | 54.4 | 55388 | 45.1 | 1.00 Reference | 1.00 Reference | ||
| 1 | 23859 | 23.7 | 29382 | 23.9 | 0.82 (0.80-0.84) | 0.87 (0.85-0.90) | ||
| ≥ 2 | 10771 | 10.7 | 13200 | 10.8 | 0.83 (0.80-0.85) | 0.74 (0.71-0.76) | ||
| Missing | 11225 | 11.2 | 24806 | 20.2 | ||||
| Parity | 1 (0-11) | 1 (0-10) | ||||||
| 0 | 42661 | 42.4 | 44765 | 36.5 | 1.00 Reference | 1.00 Reference | ||
| 1 | 18728 | 18.6 | 23021 | 18.8 | 0.85 (0.83-0.87) | 0.91 (0.88-0.94) | ||
| 2 | 18869 | 18.8 | 22469 | 18.3 | 0.88 (0.86-0.90) | 0.89 (0.86-0.92) | ||
| ≥ 3 | 10555 | 10.5 | 13735 | 11.2 | 0.81 (0.78-0.83) | 0.84 (0.81-0.88) | ||
| Missing | 9792 | 9.7 | 18786 | 15.3 | ||||
| Level of education3 | ||||||||
| Elementary/secondary school | 13001 | 12.9 | 8428 | 6.9 | 0.74 (0.71-0.76) | 0.78 (0.75-0.81) | ||
| High school/upper secondary | 34200 | 34.0 | 16315 | 13.3 | 1.00 Reference | 1.00 Reference | ||
| Collage/universityMissing | 19176 | 19.1 | 7074 | 5.8 | 1.29 (1.25-1.34) | 1.19 (1.15-1.24) | ||
| 34228 | 34.0 | 90959 | 74.1 | |||||
| Occupational status | ||||||||
| Full time | 41499 | 41.2 | 46920 | 38.2 | 1.00 Reference | 1.00 Reference | ||
| Part time | 15413 | 15.3 | 14781 | 12.0 | 1.18 (1.15-1.21) | 1.18 (1.15-1.21) | ||
| Student | 21762 | 21.6 | 28043 | 22.8 | 0.88 (0.86-0.90) | 0.88 (0.86-0.90) | ||
| Out of work | 6352 | 6.3 | 8675 | 7.0 | 0.83 (0.80-0.86) | 0.83 (0.80-0.86) | ||
| Other | 9248 | 9.2 | 17321 | 14.1 | 0.60 (0.59-0.62) | 0.60 (0.59-0.62) | ||
| Missing | 6331 | 6.3 | 7036 | 5.7 | ||||
| Marital status | ||||||||
| Married | 18193 | 18.1 | 23396 | 19.1 | 0.94 (0.92-0.96) | 0.89 (0.86-0.92) | ||
| Cohabiting | 26388 | 26.2 | 28978 | 23.6 | 1.10 (1.07-1.12) | 1.09 (1.07-1.12) | ||
| Single | 47058 | 46.8 | 56667 | 46.2 | 1.00 Reference | 1.00 Reference | ||
| Divorced/widowed | 4270 | 4.2 | 5436 | 4.4 | 0.95 (0.91-0.99) | 0.96 (0.91-1.02) | ||
| Missing | 4696 | 4.7 | 8299 | 6.8 | ||||
| . | Medical (n = 100605) . | Surgical (n = 122776) . | Crude . | Adjusted2 . | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) . | OR (95% CI) . | |||||||
| N . | % . | Median (range) . | N . | % . | Median (range) . | . | . | |
| Age (years) | 26 (12-52) | 26 (12-51) | ||||||
| ≤ 19 | 13596 | 13.5 | 21161 | 17.2 | 0.74 (0.72-0.76) | 0.85 (0.82-0.87) | ||
| 20-24 | 28209 | 28.0 | 32542 | 26.5 | 1.00 Reference | 1.00 Reference | ||
| 25-29 | 22811 | 22.7 | 26259 | 21.4 | 1.00 (0.98-1.03) | 0.99 (0.97-1.02) | ||
| 30-34 | 17744 | 17.6 | 21819 | 17.8 | 0.94 (0.91-0.96) | 0.98 (0.95-1.01) | ||
| 35-39 | 12911 | 12.8 | 15139 | 12.3 | 0.98 (0.96-1.01) | 0.99 (0.96-1.03) | ||
| 40-44 | 4944 | 4.9 | 5336 | 4.3 | 1.07 (1.03-1.11) | 1.00 (0.95-1.05) | ||
| ≥ 45 | 384 | 0.4 | 408 | 0.3 | 1.09 (0.94-1.25) | 0.96 (0.81-1.15) | ||
| Missing | 6 | 0 | 112 | 0.1 | ||||
| Gestational age (weeks) | 7 (4-12) | 8 (4-12) | ||||||
| 4-6 | 41874 | 41.6 | 20522 | 16.7 | 2.34 (2.29-2.39) | 2.11 (2.06-2.16) | ||
| 7-8 | 46682 | 46.4 | 53454 | 43.5 | 1.00 Reference | 1.00 Reference | ||
| 9-10 | 8893 | 8.8 | 36304 | 29.6 | 0.28 (0.27-0.29) | 0.22 (0.22-0.23) | ||
| 11-12 | 2881 | 2.9 | 12429 | 10.1 | 0.27 (0.25-0.28) | 0.19 (0.18-0.20) | ||
| Missing | 275 | 0.3 | 67 | 0 | ||||
| Previous abortions | 0 (0-11) | 0 (0-12) | ||||||
| 0 | 54750 | 54.4 | 55388 | 45.1 | 1.00 Reference | 1.00 Reference | ||
| 1 | 23859 | 23.7 | 29382 | 23.9 | 0.82 (0.80-0.84) | 0.87 (0.85-0.90) | ||
| ≥ 2 | 10771 | 10.7 | 13200 | 10.8 | 0.83 (0.80-0.85) | 0.74 (0.71-0.76) | ||
| Missing | 11225 | 11.2 | 24806 | 20.2 | ||||
| Parity | 1 (0-11) | 1 (0-10) | ||||||
| 0 | 42661 | 42.4 | 44765 | 36.5 | 1.00 Reference | 1.00 Reference | ||
| 1 | 18728 | 18.6 | 23021 | 18.8 | 0.85 (0.83-0.87) | 0.91 (0.88-0.94) | ||
| 2 | 18869 | 18.8 | 22469 | 18.3 | 0.88 (0.86-0.90) | 0.89 (0.86-0.92) | ||
| ≥ 3 | 10555 | 10.5 | 13735 | 11.2 | 0.81 (0.78-0.83) | 0.84 (0.81-0.88) | ||
| Missing | 9792 | 9.7 | 18786 | 15.3 | ||||
| Level of education3 | ||||||||
| Elementary/secondary school | 13001 | 12.9 | 8428 | 6.9 | 0.74 (0.71-0.76) | 0.78 (0.75-0.81) | ||
| High school/upper secondary | 34200 | 34.0 | 16315 | 13.3 | 1.00 Reference | 1.00 Reference | ||
| Collage/universityMissing | 19176 | 19.1 | 7074 | 5.8 | 1.29 (1.25-1.34) | 1.19 (1.15-1.24) | ||
| 34228 | 34.0 | 90959 | 74.1 | |||||
| Occupational status | ||||||||
| Full time | 41499 | 41.2 | 46920 | 38.2 | 1.00 Reference | 1.00 Reference | ||
| Part time | 15413 | 15.3 | 14781 | 12.0 | 1.18 (1.15-1.21) | 1.18 (1.15-1.21) | ||
| Student | 21762 | 21.6 | 28043 | 22.8 | 0.88 (0.86-0.90) | 0.88 (0.86-0.90) | ||
| Out of work | 6352 | 6.3 | 8675 | 7.0 | 0.83 (0.80-0.86) | 0.83 (0.80-0.86) | ||
| Other | 9248 | 9.2 | 17321 | 14.1 | 0.60 (0.59-0.62) | 0.60 (0.59-0.62) | ||
| Missing | 6331 | 6.3 | 7036 | 5.7 | ||||
| Marital status | ||||||||
| Married | 18193 | 18.1 | 23396 | 19.1 | 0.94 (0.92-0.96) | 0.89 (0.86-0.92) | ||
| Cohabiting | 26388 | 26.2 | 28978 | 23.6 | 1.10 (1.07-1.12) | 1.09 (1.07-1.12) | ||
| Single | 47058 | 46.8 | 56667 | 46.2 | 1.00 Reference | 1.00 Reference | ||
| Divorced/widowed | 4270 | 4.2 | 5436 | 4.4 | 0.95 (0.91-0.99) | 0.96 (0.91-1.02) | ||
| Missing | 4696 | 4.7 | 8299 | 6.8 | ||||
A total of 311 (0.1%) of the women had no record of method.
Adjusted for gestational age, the woman’s age and year of the abortion.
Level of education was not registered prior to 2006.
The mean number of waiting days between registered requests for abortion until termination decreased from 11.3 in 1998 to 7.3 days in 2013. The decline in waiting days for medical abortion was from 12.3 days in 1998 to 6.6 days in 2013, in comparison with a decline from 11.3 to 10.1 days for surgical termination, respectively.
Discussion
To the best of our knowledge, this is the first complete countrywide report on all registered legal abortions from a 15-year introductory period of medical abortion. We present full figures from all hospitals performing abortions and all abortions conducted during this period. Norway experienced an almost complete change in the use of abortion methods from surgical to medical abortion. In the same period, an increasing percentage of all abortions were performed within 9 weeks of gestation and there was a reduction in waiting time from the request for an abortion to termination.
The percentage of all abortions undergone medically increased from 5.9% to 82.1% between 1998 and 2013. In the same time period, the number of abortions remained stable with a slight decrease in abortion rates.3 Thus, in spite of concerns that a non-surgical method would increase the total number of abortions, this did not happen. A similar trend in use of medical abortion and abortion rates are found in the other Scandinavian countries and Scotland, where most abortions are done within the National Health Services (NHS).17,18 We identified an increase in abortions undergone before 9 weeks of gestation. This is also in line with changes observed in Scotland, Portugal and other Scandinavian countries.17–19 The majority of hospitals in our study followed recommended guidelines for mifepristone dose and vaginal administration of misoprostol for all gestational ages. In contrast, a similar development could not be revealed in a national Dutch study where 45.7% of the institutions used either misoprostol or mifepristone as a single agent for termination of pregnancy.20
After 2008, the Abortion Registry reported on a rapid increase in the percentage of abortions undergone medically.3 This prompted the repeat survey in 2012 where we found a rapid increase in the percentage of all hospitals offering home administration of misoprostol and medical abortion at 9–12 weeks after 2008 (Figure 2). Subsequently, the percentage of all abortions performed medically exceeded 50% (Figure 3). The increased use of medical abortion followed the rapid scaling up of access to home administration of misoprostol. Since most women prefer one single visit when having an abortion, the introduction of home administration of misoprostol with the possibility of one single consultation could have been an important factor.21,22 On the other hand, experience with medical abortion had accumulated in Norway by 2008. Medical abortion requires fewer resources, is more cost-efficient and enables re-allocation of services to other patient groups. This makes it a good alternative to surgical abortion for the hospitals.12,13 The annual report from the Abortion Registry for 2015 describes a frequent use of medical abortion (range 60.9-100%) in Norwegian hospitals.3 The increase could be driven by both women’s and provider preference. In places where unsafe abortions are abundant and health services and personnel are lacking, these aspects make medical abortion particularly important in increasing access to abortion.
In our surveys we found u-hCG tests for follow-up after abortion to be the most frequently used method in Norway. The surveys did not differentiate between low- and high-sensitive u-hCG tests nor included information on at what time follow-up was planned. Most medical abortion protocols regularly include a follow-up procedure. Several studies have found self-assessment and u-hCG in combination with a telephone interview to be a good alternative to s-hCG and ultrasound, as these simplify access and reduce the resources needed.13,23,24 Self-assessment combined with u-hCG is another promising approach, but still there is a need for more sensitive and simpler tests to reduce errors both in use and in interpretation of results.13
A reduced waiting time from 11.3 days in 1998 to 7.3 days in 2013 between a registered request for an abortion to having the abortion was found. A study from the UK has earlier retrieved a similar reduction in waiting time after introduction of medical abortion.25 Several countries have included compulsory waiting time in their abortion legislation under the argument that women ideally should have a window to reconsider.26,27 The percentage of requests being provided dropped from 92.3% in 1998 to 88.5% in 2013, whereas access to abortion was not reduced in the same period. This reduction indicates that women are getting enough time to re-evaluate their decisions.
In our study, women who underwent medical abortion had a higher level of education than those treated with surgical abortion. This is in line with other studies.28,29,30 Unfortunately, educational attainment was not registered before 2006, with a high percentage of missing data in our material as a result.
The major strengths of this study are the population-based design comprising all abortions conducted in Norway during 1998–2013, and a 100% response rate in surveys from all the hospitals performing abortions in Norway. There might be a bias in recalling exactly when the hospitals implemented medical abortion for the period 1998–2008. The number of clinics registered as performing the different treatments in 2008 and 2012, on the other hand, should not be subject to error. The types of variables recorded in the Abortion Registry are fairly similar over the years. Since information is de-identified, data quality control is not possible through linkage of the registry with other databases or studies. On the other hand, the Abortion Registry shares data management personnel, routines and strategies with the Norwegian Medical Birth Registry, a registry that through multiple validation studies has been found to have high validity of data.31,32 As information on previous abortions and deliveries, education level, marital status and employment status are self-reported parameters, the likelihood of information bias must be taken into account when interpreting the results. Possible stigma could influence the women’s information. The registry has also had a delay in including changes in abortion practice into their standard registration form. We chose to use two different data sources to try to broaden the information about access and quality of medical abortion care beyond what was available from only one source. By using two different sources we obtained information on both a population and an institutional level. We found that the two different data sources complemented each other in describing and explaining the implementation process. Large data registries like the Abortion Registry are very often delayed in including new clinical treatment options into their checkboxes. This is for instance the case regarding home administration of misoprostol in Norway. Without the facility survey, the role of home administration of misoprostol could not have been addressed in this study. Neither does the Abortion Registry include information on follow-up procedures after an abortion.
Our study revealed that Norwegian hospitals offer a variety of different treatment protocols for medical abortion, anchored in international guidelines. There seems to be a trend towards simplification of the treatment process. The major findings after the introduction of medical abortion have been access to abortion at an earlier gestational age, and reduced waiting time for women. Medical abortion needs fewer resources than surgical abortion and, as a consequence of the shift in treatment, local and national health services have been able to release capacity that could be reallocated to other treatment groups without compromising the needs of women with unwanted pregnancies.
Funding
This work was supported by the Faculty of Medicine and Dentistry, University of Bergen, Norway. The funders had no role: in the study design; in the collection, analysis or interpretation of data; in the writing of the report; nor in the decision to submit for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author contributions
M.L. contributed to the study design, data sampling, data analysis and interpretation, and drafting of the report. T.B. contributed to the study design, data analysis and interpretation, and drafting of the report. O.E.I. contributed to the study design and commented on the draft of the report. R.A. contributed to the data analysis and interpretation and commented on the draft of the report. L.B. contributed to the study design, data analysis and drafting of the report. All contributors have read and approved the final version.
Conflict of interest: None declared.
Key messages
There has been an almost complete change in abortion treatment in Norway from predominantly surgical abortion in 1998 to medical abortion in 2013.
Norwegian hospitals follow national and international guidelines.
After the introduction of medical abortion, women access abortion at an earlier gestational age and waiting time from the request of an abortion to termination has been reduced.
A total of 311 (0.1%) of the women had no record of method.
Adjusted for gestational age, the woman’s age and year of the abortion
Level of education was not registered prior to 2006
References
Lovdata (Norwegian laws). Lov om svangerskapsavbrudd. [Law on pregnancy termination]



