-
PDF
- Split View
-
Views
-
Cite
Cite
Deepa Sasikumar, Baiju S Dharan, Priyadarshini Arunakumar, Arun Gopalakrishnan, Sivasubramonian Sivasankaran, Kavasseri M Krishnamoorthy, The outcome of mitral regurgitation after the repair of anomalous left coronary artery from the pulmonary artery in infants and older children, Interactive CardioVascular and Thoracic Surgery, Volume 27, Issue 2, August 2018, Pages 238–242, https://doi.org/10.1093/icvts/ivy022
Close - Share Icon Share
Abstract
Mitral regurgitation (MR) in the majority of infants with an anomalous left coronary artery from the pulmonary artery (ALCAPA) has been shown to improve without concomitant mitral valve repair. However, the outcome of MR in older children with ALCAPA is unclear. The purpose of this study was to compare the outcome of MR following the ALCAPA repair in infants and older children.
Forty-six patients (34 were younger than 1 year and 12 were aged 1–12 years) underwent the repair for ALCAPA in our institution from June 2006 to June 2016. Baseline and follow-up data were collected from records, and the latest echocardiogram was performed for all surviving patients from June 2017 to August 2017.
Of the 34 infants, 82% had moderate-to-severe ventricular dysfunction, and 47% had significant MR at presentation. Fifty-seven percent of the older age group had MR, though none of them had ventricular dysfunction. Two infants and 3 older children underwent concomitant mitral valve repair. There were 2 early deaths in the infantile group. On follow-up, ventricular function normalized in 88% of infants; 12.5% of the infants had moderate-to-severe MR on follow-up, and 50% of the older children had moderate-to-severe MR on follow-up.
The ALCAPA repair has excellent survival outcomes in all age groups. MR improves in the majority of infants with revascularization alone. MR worsens or persists in a significant number of older children following the ALCAPA repair, and they are more likely to require reinterventions for the mitral valve on follow-up.
INTRODUCTION
The anomalous origin of coronary artery from the pulmonary artery (ALCAPA) is a rare anomaly [1], which occurs in infancy with features of myocardial ischaemia, causing significant morbidity and mortality [2] if not promptly identified and surgically corrected. The adult population with ALCAPA has good collateral flow to the left coronary system, and hence, detection maybe incidental or they may present with chest pain, dyspnoea, effort intolerance, syncope, arrhythmias or as sudden cardiac death [3–5]. Surgical options have evolved over the years, with the majority of the patients now being treated with direct reimplantation of the left coronary artery (LCA) button to the aorta [6]. This surgical technique has proved to have excellent long-term outcomes [7, 8]. The rare subsets that are not suitable for coronary reimplantation are managed by the Takeuchi procedure and the LCA ligation with or without coronary artery bypass grafting [9–12].
Mitral regurgitation (MR) occurs in a significant subset of these patients as a result of annular dilatation following ventricular dysfunction or due to papillary muscle dysfunction caused by ischaemia. In the majority of the cases occurring in infancy, in whom the MR is likely to be predominantly due to annular dilatation, the MR has been shown to improve after coronary reimplantation without the need for concomitant mitral valve repair or replacement [13, 14]. However, with regard to ALCAPA in older children (beyond infancy), in whom long-standing ischaemia-related papillary muscle dysfunction may contribute to MR, the outcome is less clear. We studied the outcome of MR following the ALCAPA repair between infancy and older children.
METHODS
All patients younger than 12 years who underwent surgical repair of ALCAPA with or without concomitant mitral valve repair from June 2006 to June 2016 were included in the study. This study had the institutional ethics committee approval. The patients were analysed in 2 groups based on the age at surgery: (i) less than 1 year and (ii) 1–12 years. The median follow-up was 4.5 years (1–10 years). Clinical and demographic data were collected from case records. The degree of MR and ventricular dysfunction at presentation, prior to discharge from hospital after surgery, at 1 month and at 1 year were noted from the case records. The latest follow-up echocardiogram was obtained prospectively, by a single echocardiographer, from June 2017 to August 2017. Left ventricular dysfunction [15] was termed as severe if ejection fraction (EF) was <30%, moderate if EF was 30–39%, mild if EF was 40–49% and normal if EF was >50%. MR was graded based on vena contracta width and ratio of MR area/left atrial area to none (0), trivial (1+), mild (2+), moderate (3+) and severe (4+), based on current guidelines [16]. Early mortality was defined as death within 30 days of surgery or before hospital discharge. Outcomes were analysed in terms of survival, persistent ventricular dysfunction, presence of moderate-to-severe MR and need for any reintervention.
Surgery
ALCAPA was repaired by direct coronary reimplantation of the LCA to the aorta in all patients. In our institution, concomitant mitral valve repair in ALCAPA patients is done (i) in all patients irrespective of age who had severe MR at presentation, (ii) in patients who had significant restriction of posterior leaflet movement or (iii) if anatomical abnormalities of the valve-like mitral valve prolapse or cleft are present. Transoesophageal echocardiogram was used during all surgeries, and perioperative assessment of the mitral valve was done to decide on the need for mitral valve repair. Mitral valve repair consisted of posterior annuloplasty with augmentation with autologous-treated pericardium in all patients. Two patients with posterior mitral leaflet tethering were treated by the release of tethered PML chords, which improved the mobility and coaptation of mitral leaflets.
Statistics
Continuous variables are reported as medians with minimum and maximum for skewed data or means with standard deviations for data with normal distribution. Categorical variables are reported as frequencies with percentages and were analysed using the Fisher’s exact test. Independent continuous variables were compared by the unpaired Student’s t-test for normally distributed data, and the Mann–Whitney U-test was used for the comparison of parameters that did not exhibit a normal distribution. A P-value <0.05 was considered statistically significant. All analyses were performed with the Statistical Package for the Social Sciences 21.0.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
During the period from June 2006 to June 2016, 46 patients underwent surgical repair of ALCAPA; 34 were infants younger than 1 year at the time of surgery (median age 4 months; range 2–11 months), and 12 were children aged between 1 and 12 years (median age 5.5 years; range 1.5–12 years) (Table 1). None of the patients older than 1 year had ventricular dysfunction (defined as EF <50%), whereas the majority of the infants with ALCAPA (82%) had moderate-to-severe ventricular dysfunction at presentation. The median EF in the less than 1-year group was 30% (range 15–49%), whereas that of the older age group was 62% (range 51–80%). Significant (moderate-to-severe) MR was present in 47% of infants and in 57% of children aged 1–12 years.
| Characteristics . | Age <1 year . | Age 1-12 years . |
|---|---|---|
| Age at repair | 4 months (2–11) | 5.5 years (1.5–12) |
| Body surface area | 0.28 (0.22–0.36) | 0.64 (0.39–1.0) |
| Ventricular dysfunction | ||
| Normal to mild | 6 | 12 |
| Moderate | 13 | 0 |
| Severe | 15 | 0 |
| Mitral regurgitation | ||
| None to mild | 17 | 5 |
| Moderate | 13 | 6 |
| Severe | 2 | 1 |
| CPB (min) | 180 (133–358) | 190 (110–311) |
| ACC (min) | 89.5 (64–142) | 96 (67–199) |
| Mitral valve repair | 2 | 3 |
| Characteristics . | Age <1 year . | Age 1-12 years . |
|---|---|---|
| Age at repair | 4 months (2–11) | 5.5 years (1.5–12) |
| Body surface area | 0.28 (0.22–0.36) | 0.64 (0.39–1.0) |
| Ventricular dysfunction | ||
| Normal to mild | 6 | 12 |
| Moderate | 13 | 0 |
| Severe | 15 | 0 |
| Mitral regurgitation | ||
| None to mild | 17 | 5 |
| Moderate | 13 | 6 |
| Severe | 2 | 1 |
| CPB (min) | 180 (133–358) | 190 (110–311) |
| ACC (min) | 89.5 (64–142) | 96 (67–199) |
| Mitral valve repair | 2 | 3 |
ACC: aortic cross-clamp; CPB: cardiopulmonary bypass time.
| Characteristics . | Age <1 year . | Age 1-12 years . |
|---|---|---|
| Age at repair | 4 months (2–11) | 5.5 years (1.5–12) |
| Body surface area | 0.28 (0.22–0.36) | 0.64 (0.39–1.0) |
| Ventricular dysfunction | ||
| Normal to mild | 6 | 12 |
| Moderate | 13 | 0 |
| Severe | 15 | 0 |
| Mitral regurgitation | ||
| None to mild | 17 | 5 |
| Moderate | 13 | 6 |
| Severe | 2 | 1 |
| CPB (min) | 180 (133–358) | 190 (110–311) |
| ACC (min) | 89.5 (64–142) | 96 (67–199) |
| Mitral valve repair | 2 | 3 |
| Characteristics . | Age <1 year . | Age 1-12 years . |
|---|---|---|
| Age at repair | 4 months (2–11) | 5.5 years (1.5–12) |
| Body surface area | 0.28 (0.22–0.36) | 0.64 (0.39–1.0) |
| Ventricular dysfunction | ||
| Normal to mild | 6 | 12 |
| Moderate | 13 | 0 |
| Severe | 15 | 0 |
| Mitral regurgitation | ||
| None to mild | 17 | 5 |
| Moderate | 13 | 6 |
| Severe | 2 | 1 |
| CPB (min) | 180 (133–358) | 190 (110–311) |
| ACC (min) | 89.5 (64–142) | 96 (67–199) |
| Mitral valve repair | 2 | 3 |
ACC: aortic cross-clamp; CPB: cardiopulmonary bypass time.
All patients underwent a direct LCA reimplantation to the aorta. The LCA was from the left posterior sinus of the pulmonary artery in all but 1 case, in whom the LCA was from the left anterior sinus. One patient had a separate origin of the left anterior descending and left circumflex artery from the left posterior sinus. Mean cardiopulmonary bypass time and aortic cross-clamp times were similar for both age groups (Table 1). Hospital stay was significantly longer for the infantile group than for the older age group (15.3 ± 9.4 days vs 6.8 ± 1.2 days; P = 0.023) (Table 2).
| Outcomes . | Age <1 year . | Age 1–12 years . |
|---|---|---|
| Hospital stay (days), mean (standard deviation) | 15.3 (9.4) | 6.8 (1.2) |
| Deaths, n (%) | 2 (5.8) | 0 |
| Ventricular dysfunction | ||
| None to mild | 31 | 12 |
| Moderate | 1 | 0 |
| Severe | 0 | 0 |
| Mitral regurgitation | ||
| None to mild | 28 | 6 |
| Moderate | 4 | 5 |
| Severe | 0 | 1 |
| Outcomes . | Age <1 year . | Age 1–12 years . |
|---|---|---|
| Hospital stay (days), mean (standard deviation) | 15.3 (9.4) | 6.8 (1.2) |
| Deaths, n (%) | 2 (5.8) | 0 |
| Ventricular dysfunction | ||
| None to mild | 31 | 12 |
| Moderate | 1 | 0 |
| Severe | 0 | 0 |
| Mitral regurgitation | ||
| None to mild | 28 | 6 |
| Moderate | 4 | 5 |
| Severe | 0 | 1 |
| Outcomes . | Age <1 year . | Age 1–12 years . |
|---|---|---|
| Hospital stay (days), mean (standard deviation) | 15.3 (9.4) | 6.8 (1.2) |
| Deaths, n (%) | 2 (5.8) | 0 |
| Ventricular dysfunction | ||
| None to mild | 31 | 12 |
| Moderate | 1 | 0 |
| Severe | 0 | 0 |
| Mitral regurgitation | ||
| None to mild | 28 | 6 |
| Moderate | 4 | 5 |
| Severe | 0 | 1 |
| Outcomes . | Age <1 year . | Age 1–12 years . |
|---|---|---|
| Hospital stay (days), mean (standard deviation) | 15.3 (9.4) | 6.8 (1.2) |
| Deaths, n (%) | 2 (5.8) | 0 |
| Ventricular dysfunction | ||
| None to mild | 31 | 12 |
| Moderate | 1 | 0 |
| Severe | 0 | 0 |
| Mitral regurgitation | ||
| None to mild | 28 | 6 |
| Moderate | 4 | 5 |
| Severe | 0 | 1 |
Survival
Two infants died prior to hospital discharge: 1 infant due to sepsis on 22nd postoperative day and 1 baby died on the first postoperative day due to intractable ventricular arrhythmias. All patients in the 1–12-year age group survived. There were no late deaths in either groups during a median follow-up period of 4.5 years (range 1–10 years).
Management of mitral regurgitation
Two patients in the infantile group and 1 patient in the 1–12-year age group had severe MR, and both underwent concomitant mitral valve repair in the form of posterior mitral annuloplasty. Of the 4 patients in the 1–12-year age group who had moderate MR at presentation, 2 had posterior mitral leaflet tethering with resultant prolapse of anterior mitral leaflet, and they underwent concomitant mitral valve repair (posterior mitral annuloplasty and partial release of posterior mitral leaflet chordae). The patients who underwent concomitant mitral valve repair had significantly longer aortic cross-clamp times when compared with patients who underwent coronary reimplantation only (126 ± 17.4 vs 92.2 ± 22.2; P = 0.007), but the length of hospital stay was similar for the patients with and without concomitant mitral valve repair.
Recovery of ventricular function
None of the patients in the older age group had ventricular dysfunction on follow-up. Eighty-eight percent of the patients in the infantile group had good ventricular function on the last follow-up. Mean time to recovery of ventricular function was 3 months (range 0–12 months). Only 1 patient continued to have moderate ventricular dysfunction, and 3 had mild dysfunction on follow-up. Regional wall motion abnormality persisted in none (of the 4 who had regional wall motion abnormality) in the 1–12-year age group and in 1 out of 14 who had regional wall motion abnormality in the infantile group.
Outcome of mitral valve regurgitation on follow-up
Moderate-to-severe MR on the last follow-up was observed in only 12% in the less than 1-year age group (Fig. 1) when compared with 50% of the 1–12-year age group (P = 0.034) (Fig. 2). MR remained trivial in 2 patients who had preoperative trivial MR in the older age group. Among the 3 patients who had mild MR in this age group, 2 patients worsened to moderate MR on follow-up. Of the 6 patients who had preoperative moderate MR in the older age group, 2 underwent concomitant mitral valve repair, and they had mild MR on follow-up. Of the remaining 4 patients who did not have concomitant mitral valve repair in this group, 3 continued to have moderate MR and 1 worsened to severe MR on follow-up. The child in the older age group who had severe preoperative MR underwent concomitant mitral valve repair and had only mild MR on follow-up. Thus, the grade of MR worsened on follow-up in 3 of 12 patients in the 1–12-year age group (MR worsened from mild to moderate in 2 and from moderate to severe in 1) and in only 1 of 32 patients (mild to moderate) in the infantile group. None of the variables such as pre-existing ventricular dysfunction or MR, presence of regional wall motion abnormality or duration of hospital stay were predictive of worsening MR on follow-up. None of the patients with concomitant mitral valve repair had significant MR on follow-up.
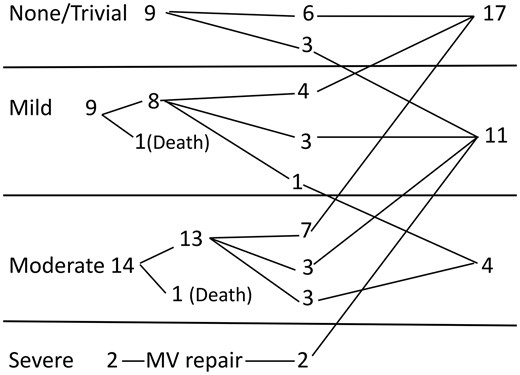
Outcome of mitral regurgitation on follow-up in the less than 1-year age group. MV: mitral valve.
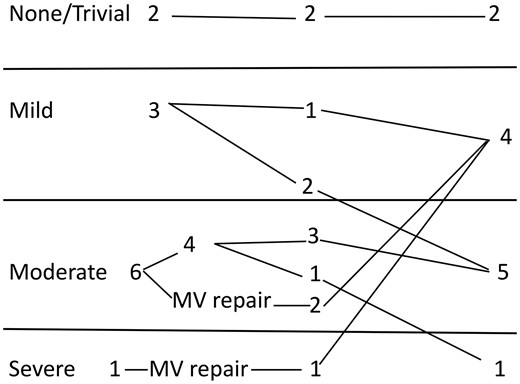
Outcome of mitral regurgitation on follow-up in the 1–12-year age group. MV: mitral valve.
DISCUSSION
Establishment of dual coronary system in ALCAPA by direct coronary reimplantation has been proved to have excellent long-term outcomes in terms of survival and recovery of ventricular function [17, 18]. Infantile form of ALCAPA is characterized by a poor collateral supply to the LCA territory, and hence, the patients are significantly symptomatic at presentation. The infants were much sicker than the older age group in our study, with 82% having moderate-to-severe ventricular dysfunction at presentation. The infants had significantly more hospital stays than the older children, but the overall survival and outcome in terms of recovery of ventricular function were excellent and comparable with the older age group. In our study, early mortality (death within 30 days of surgery) was noted only in the infantile group (2 deaths). One baby succumbed to intractable ventricular arrhythmias, and 1 baby died of sepsis. Ventricular assist device or extracorporeal membrane oxygenation support were not available in our institute at the time of study. There were no late deaths. Ventricular function normalized in 88% of these patients on follow-up with mean period of recovery of 3 months after surgery. The rapid improvement in ventricular function following surgery in this group points to reversible ischaemia in the form of stunning and hibernation as the predominant pathophysiological mechanism. None of the variables such as age at presentation, severity of ventricular dysfunction at presentation, severity of MR, aortic cross-clamp/cardiopulmonary bypass time or need for concomitant mitral valve repair were predictive of persistent ventricular dysfunction on follow-up.
The 1–12-year age group had better ventricular function at presentation, likely due to the development of adequate collaterals. There were no early or late deaths in this group. All of them continued to have good ventricular function on follow-up.
Outcome of mitral regurgitation
The question of whether to address the MR during coronary reimplantation for ALCAPA is still a controversial one, with variable institutional policies, varying from centres advocating a conservative policy of not repairing the mitral valve concomitantly [19], to centres that recommend routine mitral valve repair [20]. We keep a relatively higher threshold for concomitant mitral valve repair in the infantile age group, with repair being done only in the presence of severe MR or in patients with structural anomalies of the mitral valve. We have noted, in our experience, that the infants with preoperative severe MR tend to have a more stormy postoperative course, and hence, concomitant mitral valve repair is done for such patients. Hence, the 2 infants who had severe MR underwent concomitant mitral valve repair, whereas the infants (<1 year) with moderate MR were managed using coronary reimplantation alone. On follow-up, only 4 of the 32 infants who survived (12%) continued to have moderate MR. So, concomitant mitral valve repair may not be indicated in most of the patients in this age group, as MR has been shown to improve spontaneously with correction of the coronary anomaly in the majority of the infants. Other studies have concurred with our findings, with most of the centres now repairing only structurally abnormal valves [19, 21–23].
Outcome of MR in ALCAPA is different in the older population. In a study [24] that analysed the outcome of the ALCAPA repair in the 10–50-year age group (n = 10), concomitant mitral valve replacement was done in 4 (40%) patients. The 2 patients in that study who had unrepaired moderate MR at the time of surgery continued to have moderate MR on follow-up, and the authors have concluded that moderate-to-severe MR may be better addressed by concomitant valve repair/replacement, in this age group [24]. The outcome of MR in ALCAPA is less clear in the older children past the stage of infancy. In our study, we noted that the older age group (1–12 years), when compared with the infantile group, had worse outcomes in terms of MR. In this age group, as for the infantile group, there was a relatively higher threshold for performing concomitant mitral valve repair, in the expectation that spontaneous resolution of MR may occur with the establishment of dual-coronary system and correction of ischaemia. However, 50% of the older age group (vs 12% of infants) continued to have more than mild MR on follow-up (P = 0.034). The 3 patients in this age group who underwent concomitant mitral valve repair had mild MR on follow-up. Six of 9 patients who did not have mitral valve repair progressed (worsening MR grade, n = 3) or continued (n = 3) to have significant MR. Though no mitral valve intervention was performed in any of these children at the time of this study, longer follow-up is likely to show increased rate of reoperations for the mitral valve in this group. We postulate, from our data, that children older than 1 year may have significant papillary muscle dysfunction and tethering due to long-standing ischaemia, and hence, the MR is less likely to recover fully with revascularization alone. Though it is difficult to draw definite conclusions from the small number of patients studied, it may be reasonable to perform concomitant mitral valve repair with significant MR in an older child, particularly if associated valve tethering or papillary muscle scarring is present, to delay or prevent the need for future mitral valve reinterventions. Concomitant mitral valve repair, though associated with significantly higher cross-clamp time, was not associated with increased hospital stay, persistent ventricular dysfunction or poor survival in our study. As ALCAPA is a very rare disease, and ALCAPA in older children is even rarer, a meta-analysis of this group of patients from various studies is needed to formulate guidelines on the management of MR in this subset.
CONCLUSIONS
Direct coronary reimplantation of the LCA has good survival outcomes across all ages. The need to repair the mitral valve at the time of the ALCAPA surgery is still a matter of debate and has to be weighed against the risks of excess morbidity of an additional procedure and prolonged cardiac bypass time in the presence of ventricular dysfunction. MR improves in the majority of the infants after coronary reimplantation and concomitant mitral repair may not be indicated in this age group. Older children with unrepaired MR have significant non-resolution or progression or of preoperative MR with time and are more likely than infants to require reinterventions on follow-up.
Conflict of interest: none declared.




