-
PDF
- Split View
-
Views
-
Cite
Cite
Yazan Abu Omar, Phillip Gu, Maia Kayal, Nicholas Tedesco, Manjeet Goyal, Shrinivas Bishu, Shirley Cohen-Mekelburg, Allen Lee, Ryan Stidham, Akbar Waljee, Peter Higgins, Jeffrey Berinstein, USING LONGITUDINAL C-REACTIVE PROTEIN MEASUREMENTS THROUGHOUT HOSPITALIZATION TO ASSESS COLECTOMY RISK IN PATIENTS WITH ACUTE SEVERE ULCERATIVE COLITIS, Inflammatory Bowel Diseases, Volume 31, Issue Supplement_1, February 2025, Page S43, https://doi.org/10.1093/ibd/izae282.099
Close - Share Icon Share
Abstract
Acute severe ulcerative colitis (ASUC) is a life-threatening presentation of ulcerative colitis requiring prompt treatment. The Oxford (Travis) Index, developed in 1996, is the most widely used scoring system for identifying patients at risk of failing steroid therapy and requiring colectomy or second-line medical therapy in patients with ASUC. The Oxford Index, which was developed based on a retrospective case series of 48 patients, demonstrated that a stool frequency >8 bowel movements (BMs) per day or a stool frequency of 3-8 BMs per day in combination with a C-reactive protein (CRP) > 45 mg/L after 72 hours of corticosteroid treatment was associated with an 85% chance of requiring colectomy. Using an absolute CRP cutoff, as in the case of the Oxford Index, does not accurately consider the heterogeneity in admission CRPs and rate of improvement that exist among ASUC patients. We aim to determine the optimal timepoint and threshold of CRP for identifying patients with ASUC at risk for colectomy.
We performed a cohort study of adult patients hospitalized with ASUC between 01/2014 – 04/2024 at a single academic hospital. Latent class analysis was employed to identify distinct patient subgroups based on admission CRP levels. Univariable logistic regression was used to identify associations between 90-day colectomy and absolute CRP value and rate of CRP change from Day 0 to Day 3. Model performance was assessed using area under the receiver operator characteristic (auROC) curve.
Between 01/2014 – 04/2024, 880 patients were admitted with ASUC. Latent class analysis identified 4 distinct CRP subgroups: CRP non-producers (admission CRP < 1.0mg/dL; n=162), CRP Low (admission CRP 1.0 to 3.3mg/dL; n=321), CRP Intermediate (admission CRP 3.4 to 9.4; n=221), and CRP High (admission CRP ≥ 9.5mg/dL; n=176) Table 1 provides demographic and outcome data. Figure 1 provides longitudinal CRP trend according to admission CRP subgroup and 90-day colectomy status. Our analysis demonstrated that only an absolute Day 3 CRP [Odds Ratio (OR) 1.07; 95% confidence interval (CI) 1.02 to 1.13; p =0.008; auROC 0.684] and Day 0 to Day 3 rate of CRP change (OR 1.16; 95% CI 1.02 to 1.34; p =0.29; auROC 0.62) was associated with 90-day colectomy in the High CRP group. Absolute CRP and Day 0 to Day 3 rate of CRP change was not associated with 90-day colectomy in the Low CRP or Intermediate CRP subgroup.
Absolute day 3 CRP value and Day 0 to Day 3 rate of CRP change were identified as a significant predictor of 90-day colectomy in patients with ASUC in the High CRP subgroup; No association between CRP and 90-day colectomy were observed in the Low or High CRP subgroups. These data suggest that using an absolute CRP cutoff to determine the risk of requiring colectomy or second-line therapy may not be appropriate for all patients with ASUC.
Table 1: Demographic Characteristics and Clinical Outcomes Stratified by Admission C-reactive Protein Subgroup
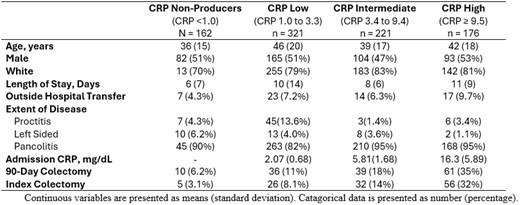
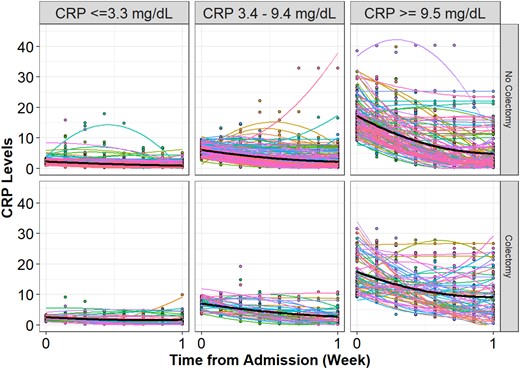
Figure 1: Longitudinal CRP Value and Trend on Each Day of Admission
- adrenal corticosteroids
- colectomy
- defecation
- ulcerative colitis
- glucocorticoids
- heterogeneity
- adult
- complex regional pain syndromes
- demography
- feces
- inpatients
- c-reactive protein
- c-reactive protein measurement
- mineralocorticoids
- treatment outcome
- metallic stents
- steroid therapy
- c-reactive protein, increased
- second line treatment
- medical management
- area under the roc curve
- latent class analysis



