-
PDF
- Split View
-
Views
-
Cite
Cite
Stephanie Kim, Nghiem Ha, Kendall Beck, FRAILTY IS ASSOCIATED WITH HIGHER RISK OF MORTALITY AND DISCHARGE TO REHABILITATION FACILITIES IN ELDERLY IBD PATIENTS HOSPITALIZED FOR GASTROINTESTINAL BLEEDS, IRRESPECTIVE OF IBD TYPE AND SEVERITY, Inflammatory Bowel Diseases, Volume 31, Issue Supplement_1, February 2025, Pages S41–S42, https://doi.org/10.1093/ibd/izae282.094
Close - Share Icon Share
Abstract
Frailty in patients with inflammatory bowel disease (IBD) is associated with increased risk for hospitalizations and mortality, particularly among older adults. We aimed to evaluate the association between frailty and clinical outcomes in elderly IBD patients hospitalized for gastrointestinal bleeds.
Included were adults ≥ 55 years with IBD who were hospitalized for upper/lower gastrointestinal bleeds between 1/2015 and 6/2023 at a single quaternary medical center. Frailty was defined using the validated Hospital Frailty Risk Score (HFRS) derived from International Classification of Disease (ICD-9/10) diagnostic codes. High-risk for frailty was defined as HFRS score ≥ 5. Univariable and multivariable logistic regression were constructed to evaluate 12-month mortality.
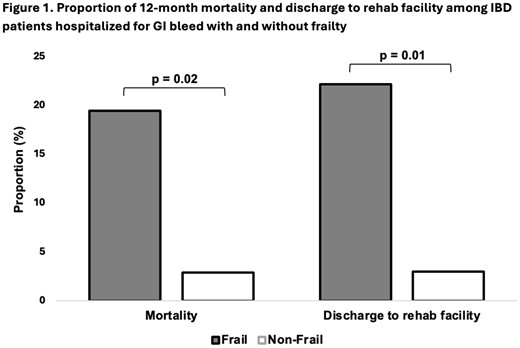
Among 111 patients, 55% were men and 60% were White with a mean age of 69 years. The majority (58%) had ulcerative colitis, while 40% had Crohn’s disease; disease activity was absent/mild in 59% and moderate/severe in 41% of patients, with 25-29% on biological therapy at the time of hospitalization. Frail patients were older than non-frail patients (mean age 71 vs 66 years, p=0.02), but did not differ significantly in terms of IBD severity, IBD-related medication, IBD-related surgical history, number of co-morbidities, or anticoagulation use prior to admission. However, a greater proportion of IBD patients with frailty were discharged to rehabilitation facilities following hospitalization (22.2% vs 3.0%, p=0.01) and experienced higher 12-month mortality (19.5% vs 2.9%, p=0.02) as compared to non-frail patients (Figure 1). Additionally, more frail patients received blood products (58.4% vs 35.3%, p=0.03), required ICU care (18.2% vs 5.9%, p=0.09), and had longer hospital stays (9 vs 7 days, p=0.60). In univariable logistic regression, frailty was significantly associated with 12-month mortality (OR 7.99, 95% CI 1.01 – 63.13) and remained significant after adjusting for age, sex, co-morbidities and IBD severity (OR 8.49, 95% CI 1.04 - 69.09); moreover, frailty was also associated with requiring discharge to rehabilitation facility when adjusting for the same factors (OR 8.73, 95% CI 1.06 – 71.55).
Frailty is associated with increased mortality and greater likelihood of discharge to a rehabilitation facility in elderly IBD patients hospitalized for GI bleeds. Assessing frailty is therefore essential for risk stratification and guiding clinical decisions to improve outcomes in this vulnerable patient population.
- anticoagulation
- crohn's disease
- inflammatory bowel disease
- ulcerative colitis
- frailty
- hemorrhagic fever with renal syndrome
- adult
- biological therapy
- frail elderly
- inpatients
- intensive care unit
- rehabilitation centers
- morbidity
- mortality
- treatment outcome
- international classification of diseases
- surgical history
- blood products
- older adult
- stratification
- diagnosis coding
- vulnerable personality



