-
PDF
- Split View
-
Views
-
Cite
Cite
Bin Bao, Youyuan Wang, Pavl Boudreau, Xinyang Song, Meng Wu, Xi Chen, Izabel Patik, Ying Tang, Jodie Ouahed, Chuan Wu, Emily Balskus, Jay Thiagarajah, Jian Liu, Michael Wessels, Wayne Lencer, Dennis Kasper, Dingding An, Bruce Horwitz, Scott Snapper, BACTERIAL SPHINGOLIPIDS EXACERBATE COLITIS BY INHIBITING ILC3-DERIVED IL-22 PRODUCTION, Inflammatory Bowel Diseases, Volume 30, Issue Supplement_1, February 2024, Page S63, https://doi.org/10.1093/ibd/izae020.133
Close - Share Icon Share
Abstract
Commensal bacteria of the Bacteroidetes phylum are the primary producers of sphingolipids in the gut lumen. These lipids serve dual roles as bacterial virulence factors and regulators of the host mucosal immune system, including regulatory T cells and invariant natural killer T cells (iNKT). Sphingolipid composition is significantly altered in fecal samples of patients with inflammatory bowel disease (IBD). However, the specific mechanisms by which bacterial sphingolipids modulate mucosal homeostasis and regulate intestinal inflammation remain unclear. In this study, we investigated the impact of bacterial sphingolipids on intestinal inflammation by mono-colonizing mice with Bacteroides fragilis strains that either express or lack sphingolipids during DSS-induced colitis. We discovered that B. fragilis sphingolipids exacerbate intestinal inflammation. Mice mono-colonized with B. fragilis lacking sphingolipids exhibited less severe DSS-induced colitis. This amelioration of colitis was associated with increased production of interleukin-22 (IL-22) by innate lymphoid cell type 3 (ILC3). Consistent with the inhibitory effect of sphingolipids on IL-22 production, mice colonized with B. fragilis lacking sphingolipids showed enhanced epithelial STAT3 activity, intestinal cell proliferation, and antimicrobial peptide production following DSS treatment compared to those colonized with B. fragilis producing sphingolipids. Additionally, colitis severity in mice colonized with B. fragilis lacking sphingolipids was exacerbated upon IL-22 blockade. Furthermore, our study reveals that bacterial sphingolipids restrict epithelial IL-18 production following DSS treatment and interfere with IL-22 production by a subset of ILC3 cells expressing both the interleukin-18 receptor (IL-18R) and major histocompatibility complex class II (MHC II). These findings indicate that B. fragilis-derived sphingolipids exacerbate mucosal inflammation by impeding epithelial IL-18 expression, resulting in compromised production of IL-22 by ILC3 cells.
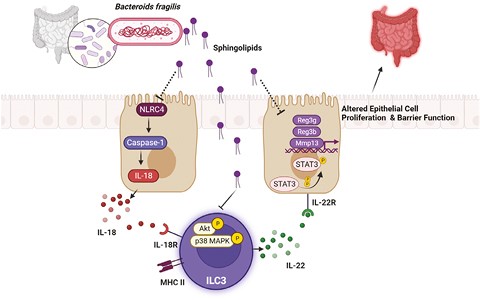
Work Model
- inflammation
- cell proliferation
- inflammatory bowel disease
- epithelium
- homeostasis
- bacteroides fragilis
- colitis
- histocompatibility antigens class ii
- infectious mononucleosis
- interleukin-18
- intestines
- sphingolipids
- bacteria
- lipids
- mice
- mucous membrane
- virulence factors
- interleukin-22
- mucositis
- regulatory t-lymphocytes
- mucosal immune system
- microbial colonization
- stat3 protein
- stool specimen
- natural killer t-cells
- symptom aggravating factors
- bacteroidetes
- antimicrobial peptide
- innate lymphoid cells



