-
PDF
- Split View
-
Views
-
Cite
Cite
Salman Haider, Daryl Ramai, Saira Shah, Asad Ur Rahman, Moazzam Hussain, Iyad Al-Bustami, Praneeth Bandaru, Denzil Etienne, ASSOCIATION OF INFLAMMATORY BOWEL DISEASE AND AUTOIMMUNE PRIMARY ADRENAL INSUFFICIENCY, Inflammatory Bowel Diseases, Volume 30, Issue Supplement_1, February 2024, Page S29, https://doi.org/10.1093/ibd/izae020.066
Close - Share Icon Share
Abstract
To assess the prevalence and association of inflammatory bowel disease (IBD) with autoimmune primary adrenal insufficiency (APAI).
Patients with inflammatory bowel disease are at risk for developing other immune mediated diseases (IMD). There is a paucity of data on the association of IBD with autoimmune primary adrenal insufficiency/ autoimmune adrenalitis. To date, only small series have been published in the literature and well-designed population-based studies have not yet examined this association.
We identified patients from the Healthcare Cost and Utilization Project - National Inpatient Sample between the years 2016 to 2020. Our cohort included IBD patients of all ages, and our control group consisted of non-IBD patients. The study's primary outcome was to evaluate the association of APAI in the study group compared to the control group. Secondary outcomes included demographics of IBD patients with APAI. ICD-10 diagnostic codes were used to identify patients.
During the study period, a total of 1,652,070 IBD patients were identified. Of these, 3,699 had a concurrent diagnosis of APAI, yielding an overall prevalence rate of 0.22%. In the non-IBD cohort, the total number of patients were 173,000,000 and the prevalence of APAI was 0.06%. Patients with IBD who had APAI were 70% females, and 90% were of white ethnic background. Among IBD patients, Crohn’s disease had a higher prevalence of APAI than Ulcerative Colitis, 0.27% vs. 0.14 %, respectively (p<0.001). Patients with IBD-APAI also had other coexisting IMDs, with asthma having the highest prevalence (13.11%), followed by rheumatoid arthritis (10.41%) and type-1 diabetes mellitus (2.57%). On multivariable logistic regression analysis, patients with IBD had 3.04 times higher odds of having a concurrent APAI diagnosis than patients without IBD (OR 3.046, CI: 2.796- 3.318, P<0.001). Women were 1.59 times more likely to have APAI than men (OR 1.590, CI: 1.539 - 1.643, p<0.001). On subgroup analysis, patients with CD had 1.9 times higher odds of having APAI than UC (OR: 1.901 CI: 1.579 - 2.290, p<0.001).
Patients with IBD, especially women of white ethnic background, have a higher association of APAI than non-IBD patients. CD patients are more likely to develop APAI than UC. Further studies are needed to understand the association and overlapping pathologic mechanisms between IMDs which may help further understand IBD-related comorbidities.
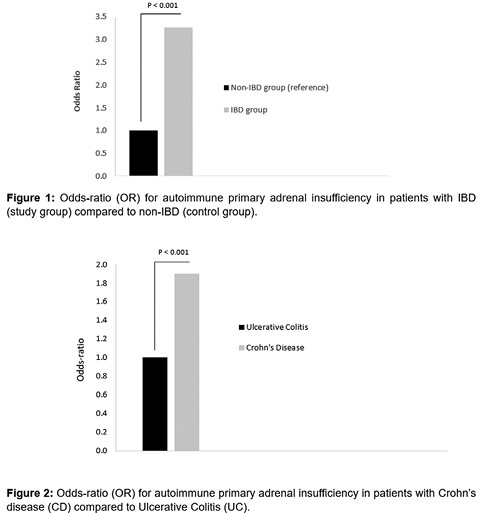
Figure
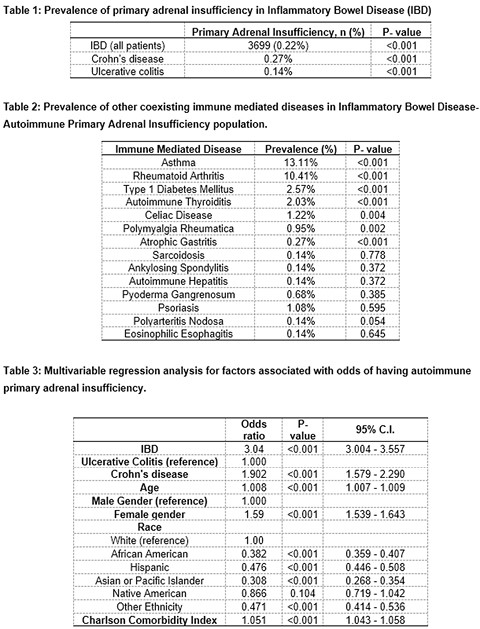
Table
- addison's disease
- rheumatoid arthritis
- diabetes mellitus
- asthma
- crohn's disease
- inflammatory bowel disease
- ulcerative colitis
- autoimmunity
- comorbidity
- demography
- ethnic group
- health care costs
- inpatients
- diagnosis
- international classification of diseases
- diagnosis coding
- ecological study
- autoimmune adrenalitis
- primary outcome measure



