-
PDF
- Split View
-
Views
-
Cite
Cite
Mitsuro Chiba, Hajime Ishii, Masato Sageshima, Akira Iwabuchi, Appendiceal Orifice Inflammation in Severe Ulcerative Colitis and Its Resolution With Infliximab and Plant-based Diet as First-line Therapy, Inflammatory Bowel Diseases, Volume 27, Issue 11, November 2021, Pages e138–e139, https://doi.org/10.1093/ibd/izab168
Close - Share Icon Share
Lay Summary
Appendiceal orifice inflammation, which is often observed in mild or moderate distal ulcerative colitis, was observed in a case of severe UC. Appendiceal orifice inflammation resolved after new induction therapy for severe UC: infliximab and a plant-based diet as first-line therapy.
To the Editor:
Appendiceal orifice inflammation (AOI) is observed as a skip lesion in mild or moderate distal ulcerative colitis (UC).1–3 Generally, the skipped AOI is correlated with the activity in the distal colon. Appendiceal orifice inflammation in severe UC is scarcely reported. It seems that some endoscopists do not insert the colonoscope proximally to the cecum in patients with severe UC due to a fear of perforation risk.3 Nowadays, many skillful endoscopists can observe the whole colon while exercising caution to prevent untoward events.
Severe UC is a potentially life-threatening disease, with a 1% mortality rate.4 First-line therapy in the current guidelines is intravenous corticosteroids. Infliximab or cyclosporine is used as rescue second-line treatment for patients unresponsive to the corticosteroids.4 Even though steroids are effective in the induction phase, steroid dependence or surgical intervention occurs in nearly half of such patients within 1 year. Because of this critical problem associated with steroids, we replaced steroids with infliximab together with a plant-based diet (PBD) for severe UC.5 This new therapy, infliximab and PBD as first-line (IPF) therapy, achieved high remission rates compared with those of the current standard. We observed AOI in a case of severe UC, and the AOI resolved with IPF therapy. The present case is 1 of 17 severe cases reported in the literature.5
A 65-year-old man with a 2-month history of bloody diarrhea (7–8 times/day) visited us. Colonoscopy revealed diffuse inflammation, erosions, and edema of the distal colon, in addition to skipped areas of inflammation in the transverse and ascending colons. Slightly swollen mucosa with white spots was observed in the appendix orifice (Figure 1A, B). Microscopically, lymphocyte and neutrophil infiltration, goblet cell depletion, and mild cryptitis were found (Figure 1C). He was ultimately diagnosed with a severe type of UC with AOI. Infliximab and PBD as first-line therapy was initiated on the fifth hospital day, after which symptoms and laboratory data gradually improved (Table 1). He was discharged after the standard third infliximab infusion. At week 6 after initiation of IPF therapy, a streak of blood still persisted. Endoscopy confirmed AOI resolution (Figure 1D), but it revealed shallow linear ulcers in the sigmoid colon. After discharge, hematochezia disappeared—clinical remission was achieved.
| Item (reference range) . | 1st . | 3rd . | 5th . | 8th . | 15th . | 23rd . | 31st . | 36th . | 44th . |
|---|---|---|---|---|---|---|---|---|---|
| White blood cell (4,000-9,000/mm3) | 18900 | 13100 | 12000 | 11100 | 5900 | 8700 | 9600 | 7900 | 7200 |
| Hemoglobin (12.6-16.0 g/dL) | 12.9 | 11.6 | 11.3 | 10.5 | 10.7 | 11.7 | 11.7 | 11.4 | 11.5 |
| Platelets (13.0-32.0 x 104/mm3) | 69.4 | 57.5 | 64.4 | 56.1 | 45.7 | 39.7 | 45.7 | 40.6 | 37.0 |
| Albumin (3.5-5.0 g/dL) | 2.6 | 1.9 | 2.4 | 2.2 | 2.4 | 2.8 | 3.2 | 2.7 | 3.0 |
| CRP (equal or less than 0.14 mg/dL) | 15.33 | 14.31 | 8.51 | 2.09 | 0.65 | 0.25 | 0.12 | 0.06 | 0.08 |
| ESR (equal or less than 16 mm/h) | 58 | 38 | 46 | 33 | 34 |
| Item (reference range) . | 1st . | 3rd . | 5th . | 8th . | 15th . | 23rd . | 31st . | 36th . | 44th . |
|---|---|---|---|---|---|---|---|---|---|
| White blood cell (4,000-9,000/mm3) | 18900 | 13100 | 12000 | 11100 | 5900 | 8700 | 9600 | 7900 | 7200 |
| Hemoglobin (12.6-16.0 g/dL) | 12.9 | 11.6 | 11.3 | 10.5 | 10.7 | 11.7 | 11.7 | 11.4 | 11.5 |
| Platelets (13.0-32.0 x 104/mm3) | 69.4 | 57.5 | 64.4 | 56.1 | 45.7 | 39.7 | 45.7 | 40.6 | 37.0 |
| Albumin (3.5-5.0 g/dL) | 2.6 | 1.9 | 2.4 | 2.2 | 2.4 | 2.8 | 3.2 | 2.7 | 3.0 |
| CRP (equal or less than 0.14 mg/dL) | 15.33 | 14.31 | 8.51 | 2.09 | 0.65 | 0.25 | 0.12 | 0.06 | 0.08 |
| ESR (equal or less than 16 mm/h) | 58 | 38 | 46 | 33 | 34 |
Abbreviations: CRP, C-reactive protein; ESR, erythrocyte sedimentation rate
| Item (reference range) . | 1st . | 3rd . | 5th . | 8th . | 15th . | 23rd . | 31st . | 36th . | 44th . |
|---|---|---|---|---|---|---|---|---|---|
| White blood cell (4,000-9,000/mm3) | 18900 | 13100 | 12000 | 11100 | 5900 | 8700 | 9600 | 7900 | 7200 |
| Hemoglobin (12.6-16.0 g/dL) | 12.9 | 11.6 | 11.3 | 10.5 | 10.7 | 11.7 | 11.7 | 11.4 | 11.5 |
| Platelets (13.0-32.0 x 104/mm3) | 69.4 | 57.5 | 64.4 | 56.1 | 45.7 | 39.7 | 45.7 | 40.6 | 37.0 |
| Albumin (3.5-5.0 g/dL) | 2.6 | 1.9 | 2.4 | 2.2 | 2.4 | 2.8 | 3.2 | 2.7 | 3.0 |
| CRP (equal or less than 0.14 mg/dL) | 15.33 | 14.31 | 8.51 | 2.09 | 0.65 | 0.25 | 0.12 | 0.06 | 0.08 |
| ESR (equal or less than 16 mm/h) | 58 | 38 | 46 | 33 | 34 |
| Item (reference range) . | 1st . | 3rd . | 5th . | 8th . | 15th . | 23rd . | 31st . | 36th . | 44th . |
|---|---|---|---|---|---|---|---|---|---|
| White blood cell (4,000-9,000/mm3) | 18900 | 13100 | 12000 | 11100 | 5900 | 8700 | 9600 | 7900 | 7200 |
| Hemoglobin (12.6-16.0 g/dL) | 12.9 | 11.6 | 11.3 | 10.5 | 10.7 | 11.7 | 11.7 | 11.4 | 11.5 |
| Platelets (13.0-32.0 x 104/mm3) | 69.4 | 57.5 | 64.4 | 56.1 | 45.7 | 39.7 | 45.7 | 40.6 | 37.0 |
| Albumin (3.5-5.0 g/dL) | 2.6 | 1.9 | 2.4 | 2.2 | 2.4 | 2.8 | 3.2 | 2.7 | 3.0 |
| CRP (equal or less than 0.14 mg/dL) | 15.33 | 14.31 | 8.51 | 2.09 | 0.65 | 0.25 | 0.12 | 0.06 | 0.08 |
| ESR (equal or less than 16 mm/h) | 58 | 38 | 46 | 33 | 34 |
Abbreviations: CRP, C-reactive protein; ESR, erythrocyte sedimentation rate
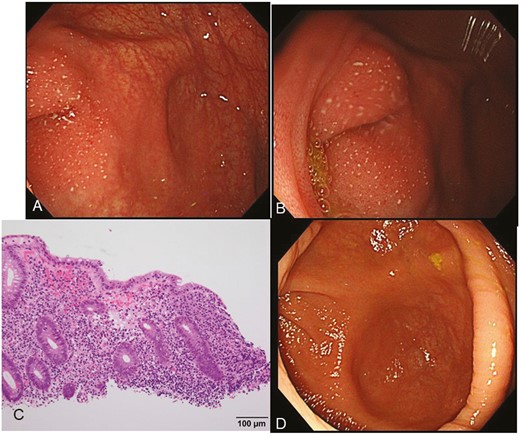
Endoscopic images of the cecum at the initial visit (A, B) and on the 43rd hospital day after infliximab and plant-based diet as first-line (IPF) therapy (D). Microscopic image (C) of appendiceal orifice inflammation (AOI). On the left side, slightly protrusive inflamed mucosa with white spots was observed in the appendix orifice. A vascular pattern is seen in the background (A). Inflammation is limited to the site of the appendiceal orifice (B). Lymphocyte and neutrophil infiltration, goblet cell depletion, and mild cryptitis are observed (C). After IPF treatment, the inflammation in the appendiceal orifice resolved (D).
In this case, severe inflammation was observed in the rectosigmoid colon. Appendiceal orifice inflammation was typical in the sense that it was associated with distal colitis, but it was associated with severe UC.
References



