-
PDF
- Split View
-
Views
-
Cite
Cite
Michelle Lockhart, Aminul Islam, Stephen Graves, Stan Fenwick, John Stenos, Detecting and measuring small numbers of viable Coxiella burnetii, FEMS Immunology & Medical Microbiology, Volume 64, Issue 1, February 2012, Pages 61–65, https://doi.org/10.1111/j.1574-695X.2011.00898.x
Close - Share Icon Share
Abstract
Coxiella burnetii is an acidophilic, intracellular bacterium that causes the human disease Q fever. In some studies, it is important to distinguish between viable and nonviable C. burnetii. We compared four methods for detecting and measuring viable C. burnetii in biological samples as follows: growth in two different cell culture lines, infection of severe combined immunodeficient (SCID) mice (leading to death) and infection of SCID mice with detection of C. burnetii in their spleen (after euthanasia at day 50 postinfection). Two isolates of C. burnetii were used (‘Henzerling’ and ‘Arandale’). Our in-house qPCR assay for C. burnetii DNA was used as a control. SCID mouse inoculation was more sensitive than cell culture. The assay that detected C. burnetii in SCID mouse spleens was slightly more sensitive than SCID mice deaths alone. Approximately one viable C. burnetii cell could be detected by this method, making it suitable for determining the viability of C. burnetii in a sample.
Introduction
In studies on the pathogenesis of the post-Q fever fatigue syndrome, our laboratory has found it necessary to distinguish between very small numbers of viable Coxiella burnetii and very low concentrations of DNA from nonviable C. burnetii, in both patient samples and samples from experimentally infected animals (Marmion et al., 2009; Sukocheva et al., 2010). Polymerase chain reaction (PCR), including the very sensitive real-time variety (qPCR), detects and quantifies DNA but does not distinguish between DNA from viable and nonviable C. burnetii. Hence, we needed an assay that was extremely sensitive and measured only viable C. burnetii. To this end, we compared cell culture with mouse inoculation, using our in-house qPCR assay for C. burnetii detection as a control. Two different isolates of C. burnetii were studied, ‘Henzerling’ (from Italy) and ‘Arandale’ (from Australia). VERO (monkey kidney) and DH82 (canine macrophages) cell cultures were utilised. Severe combined immunodeficient (SCID) mice were inoculated and compared using two different endpoint titrations; death, between days 30–50 postinfection, and the presence of C. burnetii DNA in the spleen of the healthy, euthanised mice (day 50, postinfection). These mice are known to be very susceptible to C. burnetii (Andoh et al., 2003, 2007).
Our results showed that the greatest sensitivity for detection of viable C. burnetii (one viable cell) was obtained with SCID mouse inoculation. Euthanasia at day 50 postinfection and subsequent detection of splenic C. burnetii DNA by qPCR were slightly more sensitive than death as an endpoint.
Materials and methods
Coxiella burnetii isolates
The ‘Henzerling’ isolate, originally obtained from a patient in Italy (Ransom & Huebner, 1951), was available as a homogenate of infected egg yolk sac, kindly provided by CSL Biotherapies, Australia. The ‘Arandale’ isolate, originally from a patient with acute Q fever in Australia, was available as a homogenate of SCID mice spleens. Both were expected to be of high titre. Tenfold dilutions (to 10−12) were made in Hank's balanced salt solution (HBSS; Gibco, Australia), to provide the starting material for the various titrations.
qPCR
DNA was extracted from 100 µL of each dilution (cell culture and SCID mice spleen homogenates) using the Qiagen Extraction Kit (Qiagen, Germany) following the manufacturers instructions. Each 50-µL eluant was analysed with our in-house C. burnetii specific com1 qPCR assay (Lockhart et al., 2011). As the DNA was eluted into a volume of 50 µL and of which 5 µL was analysed in each reaction, this was effectively one-tenth of the bacterial DNA in the original starting suspension. The Ct results of positive qPCR tests were used to calculate the approximate copy numbers in each dilution and to produce a standard curve (Fig. 1). This method was also used with harvested cell culture monolayers (after 50 days of incubation) and homogenised SCID mice spleens (after 50 days of infection) to determine the presence of C. burnetii by the methods described later.
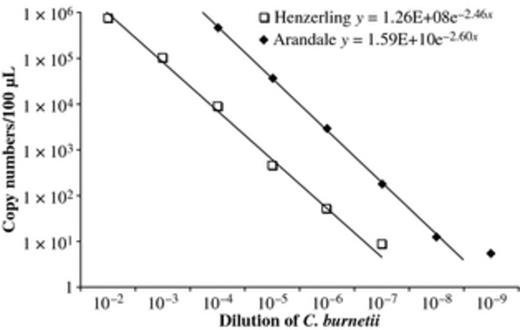
Copy numbers of Coxiella burnetii (Henzerling and Arandale isolates) present in 10-fold dilutions of suspensions, as detected by com1 qPCR. The equation of these standard curves was then used to calculate the number of copies in the dilution where 50% were positive.
Cell culture
VERO (African green monkey epithelial) and DH82 (canine macrophage) cell lines were maintained by continuous passage in RPMI 1640 medium supplemented with 10% newborn/foetal calf serum and 1% glutamine (Gibco). Cells were inoculated into 24-well trays and when confluent inoculated (in duplicate) with 100 µL of each specified dilution of the C. burnetii suspensions. These cultures were grown at 35 °C, with 5% CO2, for 50 days before harvest and analysis of the monolayer for C. burnetii DNA by qPCR.
SCID mice inoculations
Each dilution of C. burnetii suspension (100 µL) was inoculated intraperitoneally into a group of four adult female NOD.CB17-prkdcscid/JAsmu (SCID) mice (Monash University Animal Services, Australia). Mice were housed in a Techniplast cage unit (2IS012) and kept at 22 °C with food and water provided ad libitum for 50 days. The cages were fully enclosed, with Hepa filters on the exit air and under negative pressure (Techniplast, Italy), so cross-infection between mice groups was prevented. The cages were kept in an ABSL — 3 laboratory, at the Division of Microbiology, Pathology North — Hunter, John Hunter Hospital, Newcastle, Australia. The animal experiments were approved by the ‘Animal Care and Ethics Committee’ of the Australian Rickettsial Reference Laboratory. Infected mice were observed daily for 50 days. If a mouse was terminally unwell, it was euthanased immediately (ethics requirement) and this day was recorded as its day of death. Sometimes a mouse died overnight, and its day of death was recorded as the day of detection. All dead mice were removed from the cage using a biosafety cabinet (class 2) to protect the laboratory air and autoclaved immediately. Only mice that died after day 30 postinfection were considered to be deaths as a result of C. burnetii infection (based on early experiments and titrations, data not shown).
Mice that were still alive at day 50 postinfection were euthanased and their spleens removed aseptically. Each spleen was homogenised in 10-mL Hanks balanced salt solution and DNA extracted as described earlier (qPCR) but with an extended extraction time of 48 h. Samples were adjusted to a volume representing a one-hundredth sample of the whole spleen and assayed by qPCR.
Data analysis
The Spearman–Kärber method (Anellis & Werkowski, 1968) was used to calculate the dilution of the C. burnetii suspension that was 50% positive in each assay: tissue culture infectious dose 50 [TCID50]; lethal dose 50 [LD50], infectious dose ID50, and PCR detection dose 50 [DD50] were calculated. These values were then converted into copy numbers using the standard curve (Fig. 1).
Results
qPCR
Each dilution of both C. burnetii suspensions (100 µL) was tested in triplicate by the com1 qPCR assay. Results (Fig. 1) show copy number in 100 µL of each suspension dilution. The ‘Arandale’ suspension [DD501.5 × 108] was 10× more concentrated than the ‘Henzerling’ suspension [DD501.5 × 107] in total C. burnetii DNA.
Cell culture
For the ‘Arandale’ isolate, the TCID50 was 1.5 × 1010 in VERO cell culture, which was more sensitive than the DH82 cell culture (data not shown). For the ‘Henzerling’ isolate, the TCID50 was 3.2 × 106 in DH82 cell culture, which was more sensitive than VERO cell culture (data not shown) (Table 1).
Detection of DNA in suspensions of Coxiella burnetii by qPCR targeting the com1 gene (triplicate assays)
| Positive/total | ||
| C. burnetii suspension dilution | ‘Arandale’ isolate of C. burnetii | ‘Henzerling’ isolate of C. burnetii |
| 10−5 | 3/3 | |
| 10−6 | 3/3 | |
| 10−7 | 3/3 | 2/3 |
| 10−8 | 1/3 | 0/3 |
| 10−9 | 1/3 | 0/3 |
| 10−10 | 0/3 | 0/3 |
| 10−11 | 0/3 | |
| 10−12 | 0/3 | |
| DD50 | 1.5 × 108 | 1.5 × 107 |
| Positive/total | ||
| C. burnetii suspension dilution | ‘Arandale’ isolate of C. burnetii | ‘Henzerling’ isolate of C. burnetii |
| 10−5 | 3/3 | |
| 10−6 | 3/3 | |
| 10−7 | 3/3 | 2/3 |
| 10−8 | 1/3 | 0/3 |
| 10−9 | 1/3 | 0/3 |
| 10−10 | 0/3 | 0/3 |
| 10−11 | 0/3 | |
| 10−12 | 0/3 | |
| DD50 | 1.5 × 108 | 1.5 × 107 |
DD50, qPCR detection dose 50.
Detection of DNA in suspensions of Coxiella burnetii by qPCR targeting the com1 gene (triplicate assays)
| Positive/total | ||
| C. burnetii suspension dilution | ‘Arandale’ isolate of C. burnetii | ‘Henzerling’ isolate of C. burnetii |
| 10−5 | 3/3 | |
| 10−6 | 3/3 | |
| 10−7 | 3/3 | 2/3 |
| 10−8 | 1/3 | 0/3 |
| 10−9 | 1/3 | 0/3 |
| 10−10 | 0/3 | 0/3 |
| 10−11 | 0/3 | |
| 10−12 | 0/3 | |
| DD50 | 1.5 × 108 | 1.5 × 107 |
| Positive/total | ||
| C. burnetii suspension dilution | ‘Arandale’ isolate of C. burnetii | ‘Henzerling’ isolate of C. burnetii |
| 10−5 | 3/3 | |
| 10−6 | 3/3 | |
| 10−7 | 3/3 | 2/3 |
| 10−8 | 1/3 | 0/3 |
| 10−9 | 1/3 | 0/3 |
| 10−10 | 0/3 | 0/3 |
| 10−11 | 0/3 | |
| 10−12 | 0/3 | |
| DD50 | 1.5 × 108 | 1.5 × 107 |
DD50, qPCR detection dose 50.
SCID mice inoculation
In the ‘Arandale’ C. burnetii titration, four mice died before day 30 (days 3, 5, 16 and 22), and it was assumed that they died of a cause other than C. burnetii infection. All other mice died between days 34 and 49 postinfection, in a time sequence consistent with the C. burnetii suspension dilution inoculated (Table 2). The lower the inoculum, the longer it took for mice to die. Some mice remained well and were euthanased on day 50 postinfection with their spleens being tested for the presence of C. burnetii DNA (Table 2).
SCID mouse death (or euthanasia) after inoculation with 10-fold dilutions (0.1 mL) of a suspension of Coxiella burnetii (‘Arandale’ and ‘Henzerling’ isolates): day post-infection of death
+: spleen from surviving mouse positive by qPCR for C. burnetii.
−: spleen from surviving mouse negative by qPCR for C. burnetii.
ND: Average not calculated as fewer than two of the four mice died due to presumed C. burnetii infection.
Mice died before day 30 and death was considered not to be due to C. burnetii (data not used in calculations).
SCID mouse death (or euthanasia) after inoculation with 10-fold dilutions (0.1 mL) of a suspension of Coxiella burnetii (‘Arandale’ and ‘Henzerling’ isolates): day post-infection of death
+: spleen from surviving mouse positive by qPCR for C. burnetii.
−: spleen from surviving mouse negative by qPCR for C. burnetii.
ND: Average not calculated as fewer than two of the four mice died due to presumed C. burnetii infection.
Mice died before day 30 and death was considered not to be due to C. burnetii (data not used in calculations).
The LD50 of the ‘Arandale’ isolate suspension of C. burnetii was 3.2 × 109 and that of the ‘Henzerling’ isolate suspension 1.8 × 108 (Table 3), indicating the former contained approximately 10× the concentration of virulent C. burnetii than the latter.
Detection of viable Coxiella burnetii by: (a) Growth in cell culture; (b) SCID mouse inoculation (end-point: death between day 30–50 post-infection); (c) SCID mouse inoculation (end-point: spleen PCR positivity at day 50 post-infection)
No surviving mice at day 50 post-infection available for spleen PCR examination.
Detection of viable Coxiella burnetii by: (a) Growth in cell culture; (b) SCID mouse inoculation (end-point: death between day 30–50 post-infection); (c) SCID mouse inoculation (end-point: spleen PCR positivity at day 50 post-infection)
No surviving mice at day 50 post-infection available for spleen PCR examination.
With the ‘Henzerling’ isolate, the SCID mouse death assay (most dilute positive suspension 10−9) was significantly more sensitive than the cell culture assay (most dilute positive suspension 10−7) for detecting viable C. burnetii. However, with the ‘Arandale’ isolate, the two assays had similar sensitivities (most dilute positive suspension 10−10). This discrepancy has not been explained.
When examining the spleens of surviving mice (day 50) for C. burnetii DNA (as a marker of viable C. burnetii originally inoculated into the mice), it is clear that this was the most sensitive assay, with an ID50 of 6.8 × 1010 (for ‘Arandale’) and 1.0 × 109 (for ‘Henzerling’) (Table 3). However, with both isolates, the most dilute positive suspension was the same, for ‘deaths’ and ‘spleen — PCR — positivity’, being 10−10 (‘Arandale’) and 10−9 (‘Henzerling’). So for all practical purposes, both assays were equally useful.
Discussion
The need to distinguish viable from nonviable C. burnetii had arisen during the course of our investigations into the pathogenesis of the post-Q fever fatigue syndrome. When DNA from C. burnetii was detected in patient specimens by PCR, there was the issue as to whether this represented a focus of viable C. burnetii located somewhere in the patient (the conventional view) or whether it was simply the persistence of DNA from C. burnetii that had already been killed by the patient's immune system but had not been adequately cleared from the patient (the unconventional view) when assays detecting viable C. burnetii were negative. There was always the concern that the assays were not sufficiently sensitive to detect very small numbers of viable microbes. Thus, we needed a very sensitive assay to detect viable C. burnetii. We decided to use cell culture and SCID mice inoculation (Russell-Lodrigue et al., 2009). Two cell culture lines were tested (VERO and DH82).
These cell culture and mouse inoculation assays were then compared using as a control in-house, com1 qPCR which we use for the routine diagnosis of acute (preseroconversion) diagnosis of Q fever (Stenos et al., 2010).
This work commenced before the publication of the axenic medium for growing C. burnetii (Omsland et al., 2009, 2011); otherwise, it would have been also included in the comparison for detecting viable C. burnetii. Future studies should compare this medium with SCID mice inoculation for comparative sensitivity detection of viable C. burnetii in clinical and experimental samples. Given that the SCID mouse inoculation and spleen examination by qPCR can detect one viable C. burnetii cell, the axenic medium can only equal (not surpass) this theoretical lower limit to sensitivity of detection. However, if it can also detect one viable (C. burnetii) cell in clinical material, axenic culture will be a much more convenient and cost-effective method than SCID mouse inoculation, which is very slow, very expensive, requires complex laboratory facilities and animal ethics approvals.
All C. burnetii isolates are not the same (Moos & Hackstadt, 1987; Kazar et al., 1993) so we decided to test two isolates from geographically diverse regions (‘Henzerling’ — Italy and ‘Arandale’ — Australia). The data showed some minor differences.
The ‘Arandale’ isolate killed SCID mice between days 34 and 37 postinfection, whereas the ‘Henzerling’ isolate killed SCID mice between days 35 and 49 postinfection (Table 2). Of the mice surviving by day 50, and being euthanased, 3/9 (‘Arandale’) and 3/9 (‘Henzerling’) mice contained C. burnetii DNA in their spleens, indicating that not all SCID mice succumb to C. burnetii and that this assay was equally sensitive for both C. burnetii isolates. Overall, 44 SCID mice were inoculated and 22 (50%) died of C. burnetii infection. Four died of some other (undetermined) cause, before day 30, and 18 were well at day 50. Of the 18 survivors, six (one-third) had C. burnetii DNA in their spleen but appeared to be perfectly well. Thus, some SCID mice can tolerate C. burnetii infection without symptoms or dying. Of the 28 mice that were definitely infected with C. burnetii, 22 died (79% mortality rate) and six survived. This strain of mouse is very susceptible to C. burnetii, but death was not inevitable (up to day 50 postinfection). SCID mice may have some functional B and T lymphocytes that assist in their survival (Bosma & Carroll, 1991).
qPCR is still considered to be the method of choice for routine diagnosis of clinical specimens. The methods outlined in this paper are applicable only to research studies where it is imperative to distinguish viable from nonviable C. burnetii in a quantitative manner.
Overall, with both C. burnetii isolates, SCID mouse inoculation, and testing of their spleens at day 50 postinoculation for C. burnetii DNA, was the most sensitive assay for detecting viable C. burnetii. The assay's sensitivity was one viable C. burnetii cell per inoculum.
By way of comparison, earlier studies in Hartley guinea pigs (Ormsbee et al., 1978) showed that only two viable C. burnetii (phase 1) cells would produce a fever, a similar sensitivity to the SCID mouse spleen assay.
We are currently comparing the ACCM-2 medium with VERO cultures, using routine clinical samples from patients with acute Q fever. Once this study is completed, and assuming the ACCM-2 medium is as sensitive (or more sensitive) than VERO cell culture, we will then compare the ACCM-2 medium with SCID mice inoculation.
Acknowledgements
This work was supported by the Mason Foundation for research into Chronic Fatigue Syndrome. Drs J. Ferguson and R. Givney are thanked for financial assistance.
References
Author notes
Editor: Gilbert Greub



