-
PDF
- Split View
-
Views
-
Cite
Cite
Fatime Arenliu Qosaj, Margaret Bourdeaux, Health policy developments in the Western Balkan Countries 2000–19: towards European Health and Health Care Policies, European Journal of Public Health, Volume 34, Issue 3, June 2024, Pages 460–466, https://doi.org/10.1093/eurpub/ckae045
Close - Share Icon Share
Abstract
Albania, Bosnia and Herzegovina, Kosovo, Montenegro, North Macedonia and Serbia have committed to becoming European Union (EU) member states. This, among others, implies that candidate/potential candidate states adopt legally authorized EU policies, including health. The study aims to identify the main country-specific health policy areas critical to the EU accession health policy dimension and present the change in associated selected health indicators from 2000 to 2019.
The study draws on published reports and analyses of official statistics over time and cross-country. Health care policy adherence to the European Commission’s recommended country-specific health actions was classified into five health policy areas: financing, payment, organization, regulation and persuasion. Key health policy areas for Western Balkan countries (WBCs) were identified. Health progress or lack thereof in catching up to the EU15 population health, health expenditure and the number of health professionals are measured.
The European Commission prioritized financing and regulation for all WBCs in the five policy areas. Nine of the 18 analyzed selected health indicators showed divergence, and the other nine converged towards the EU15 averages. WBCs continue to face diverse public health challenges in improving life expectancy at birth, death rates caused by circulatory system diseases, malignant neoplasms, traffic accidents, psychoactive substance use, tuberculosis incidence, tobacco smoking prevalence and public-sector health expenditure.
By 2019, there is limited evidence of WBCs catching up to the average EU15 health levels and health care policies. Closer attention towards EU health and health care policies would be favourable.
Introduction
All Western Balkan countries (WBCs), namely Albania, Bosnia and Herzegovina, Kosovo, Montenegro, North Macedonia and Serbia, have decided to join the European Union (EU). While Kosovo is considered a potential candidate, all other WBCs are candidate countries.1 Besides the membership benefits, joining the EU implies certain obligations and responsibilities for the WBCs, such as harmonizing national laws with the EU acquis communautaire, a set of rights and obligations constituting the body of EU laws applicable in EU states. States that apply for EU membership are expected to accept the acquis communautaire.2 The progress of the WBCs toward EU state membership is monitored by the European Commission (EC) and reported annually in country-specific reports, publicly known as ‘progress reports’.3–8 These reports are part of the EC’s Communication on EU Enlargement Policy. ‘Progress reports’ reflect the WBC’s annual sectoral reform developments and identify challenges to be addressed, followed by recommended clear-cut actions for the way forward. Chapter 28 of these reports focus on the health dimension of the EU accession, which aims to promote ‘consumer and health protection’.3–8
Like many other transitioning countries, each WBC has experienced political, economic and social changes reflected in its health system performance and outcomes. There is an increasing number of published comparative reports based on well-established international reporting mechanisms that emphasize attention to the different aspects of the health system performance, including those of the WBCs. These reports offer relevant data on morbidity and mortality, risk factors, health expenditures/financing and quality of care.9,10 They propose selected targets and indicators to track the WBCs' progress on achieving Sustainable Development Goal 3 and a road map of priority actions for closing the health gap with the EU at the country level.11 As the data become available, a limited number of published research articles focus on different aspects of health system performance in WBCs, such as health policies,12–14 resource allocation strategies,15 health care financing sustainability, and the impoverishing effects of out-of-pocket health care expenditures16 and informal payments.17
To the best of our knowledge, in the context of governmental health policies, no published research studies quantify the change in the WBCs' public health indicators over time by measuring their convergence or divergence towards the EU15 average. In the absence of such studies, this study aims to present an overview of the main country-specific health policy areas recommended by the EC to the WBCs’ governments and present the change of relevant public health indicators towards the average of the EU15 from 2000 to 2019.
Methods
This study draws from the key EC-recommended public health actions for the WBCs,3–8 structured into five policy areas: health system financing, payment, organization, regulation and persuasion in behaviour change, referred to as means or ‘control knobs’,18 according to the Control Knob Framework. This framework is an analytical, conceptual tool that allows the adjustment of structural health system performance actions into five ‘control knobs’ that can be used as a means to control and achieve the final health system performance goals (improving health status, citizen satisfaction and financial risk protection) through intermediate goals (access, quality and efficiency of health care services).18,19 The five ‘control knobs’ in this framework, as means to improve public health through health system performance, are denoted in this study as ‘policy areas’ and are presented in table 1.
European Commission’s main recommended health policy areas with country-specific actions critical to the health policy dimension of EU accession
| Policy areas . | Country-specific recommended actions . | |||||
|---|---|---|---|---|---|---|
| Albania . | Bosnia and Herzegovina . | Kosovo . | Montenegro . | North Macedonia . | Serbia . | |
| Financing | Increase the financial/human resources in the sector, in particular in Primary Health Care. | NA | Increase financial/human resources for health sector reforms and electronic health information systems, notably for Roma and Ashkali communities. | NA | Ensure funding and specialized knowledge for the early detection of cancer and rare diseases. | Strengthen the financial sustainability of the public health insurance fund and of the authorities for consumer protection, market surveillance and sanitary inspection. |
| Payment | NA | NA | NA | NA | NA | NA |
| Organization | Strengthen all-hazard health emergency preparedness response and data quality; equal access/quality health services for vulnerable. | Strengthen health institutions in the provision of health services for Roma and Ashkali. | Implement the national programme on early detection of cancer. | Strengthen managerial sustainability of the public health insurance fund and of the relevant authorities for consumer protection, market surveillance and sanitary inspection. | ||
| Regulation | Align with the acquis on substances of human origin. medicines for human and veterinary use. and tobacco control and accede to the World Health Organization’s Framework Convention Protocol to eliminate illicit trade in tobacco products. | Adopt and enforce legislation prohibiting smoking in public places; protocol to eliminate illicit trade in tobacco; align with the acquis on: substances of human origin. and medicines for human use to ensure oversight/coordination; align with the acquis consumer protection laws and cross-border health threats including communicable diseases. | Further alignment of consumer protection law partly with EU acquis; ensure the rigorous implementation of tobacco control in line with the relevant EU acquis and international obligations. | Continue to align with the acquis on health protection. EU consumer protection, substances of human origin, tobacco control and patient’s rights, cross-border health care; adopt a new strategy for the development of the health care system; ensure administrative capacities to implement the health acquis. | Align with the acquis on consumer protection and relevant services; enhance tobacco control by effectively implementing the EU acquis on this and by ratifying the Protocol to Eliminate Illicit Trade in Tobacco Products. | Ensure the necessary institutional/administrative/technical capacity to implement the health acquis; further align EU acquis on substances of human origin on patients’ rights in cross-border health care on tobacco control and on medicines for human and veterinary use. |
| Persuasion | NA | NA | NA | NA | NA | NA |
| Policy areas . | Country-specific recommended actions . | |||||
|---|---|---|---|---|---|---|
| Albania . | Bosnia and Herzegovina . | Kosovo . | Montenegro . | North Macedonia . | Serbia . | |
| Financing | Increase the financial/human resources in the sector, in particular in Primary Health Care. | NA | Increase financial/human resources for health sector reforms and electronic health information systems, notably for Roma and Ashkali communities. | NA | Ensure funding and specialized knowledge for the early detection of cancer and rare diseases. | Strengthen the financial sustainability of the public health insurance fund and of the authorities for consumer protection, market surveillance and sanitary inspection. |
| Payment | NA | NA | NA | NA | NA | NA |
| Organization | Strengthen all-hazard health emergency preparedness response and data quality; equal access/quality health services for vulnerable. | Strengthen health institutions in the provision of health services for Roma and Ashkali. | Implement the national programme on early detection of cancer. | Strengthen managerial sustainability of the public health insurance fund and of the relevant authorities for consumer protection, market surveillance and sanitary inspection. | ||
| Regulation | Align with the acquis on substances of human origin. medicines for human and veterinary use. and tobacco control and accede to the World Health Organization’s Framework Convention Protocol to eliminate illicit trade in tobacco products. | Adopt and enforce legislation prohibiting smoking in public places; protocol to eliminate illicit trade in tobacco; align with the acquis on: substances of human origin. and medicines for human use to ensure oversight/coordination; align with the acquis consumer protection laws and cross-border health threats including communicable diseases. | Further alignment of consumer protection law partly with EU acquis; ensure the rigorous implementation of tobacco control in line with the relevant EU acquis and international obligations. | Continue to align with the acquis on health protection. EU consumer protection, substances of human origin, tobacco control and patient’s rights, cross-border health care; adopt a new strategy for the development of the health care system; ensure administrative capacities to implement the health acquis. | Align with the acquis on consumer protection and relevant services; enhance tobacco control by effectively implementing the EU acquis on this and by ratifying the Protocol to Eliminate Illicit Trade in Tobacco Products. | Ensure the necessary institutional/administrative/technical capacity to implement the health acquis; further align EU acquis on substances of human origin on patients’ rights in cross-border health care on tobacco control and on medicines for human and veterinary use. |
| Persuasion | NA | NA | NA | NA | NA | NA |
Notes: NA, not available.
Data source: European Commission. 2022.3–8
European Commission’s main recommended health policy areas with country-specific actions critical to the health policy dimension of EU accession
| Policy areas . | Country-specific recommended actions . | |||||
|---|---|---|---|---|---|---|
| Albania . | Bosnia and Herzegovina . | Kosovo . | Montenegro . | North Macedonia . | Serbia . | |
| Financing | Increase the financial/human resources in the sector, in particular in Primary Health Care. | NA | Increase financial/human resources for health sector reforms and electronic health information systems, notably for Roma and Ashkali communities. | NA | Ensure funding and specialized knowledge for the early detection of cancer and rare diseases. | Strengthen the financial sustainability of the public health insurance fund and of the authorities for consumer protection, market surveillance and sanitary inspection. |
| Payment | NA | NA | NA | NA | NA | NA |
| Organization | Strengthen all-hazard health emergency preparedness response and data quality; equal access/quality health services for vulnerable. | Strengthen health institutions in the provision of health services for Roma and Ashkali. | Implement the national programme on early detection of cancer. | Strengthen managerial sustainability of the public health insurance fund and of the relevant authorities for consumer protection, market surveillance and sanitary inspection. | ||
| Regulation | Align with the acquis on substances of human origin. medicines for human and veterinary use. and tobacco control and accede to the World Health Organization’s Framework Convention Protocol to eliminate illicit trade in tobacco products. | Adopt and enforce legislation prohibiting smoking in public places; protocol to eliminate illicit trade in tobacco; align with the acquis on: substances of human origin. and medicines for human use to ensure oversight/coordination; align with the acquis consumer protection laws and cross-border health threats including communicable diseases. | Further alignment of consumer protection law partly with EU acquis; ensure the rigorous implementation of tobacco control in line with the relevant EU acquis and international obligations. | Continue to align with the acquis on health protection. EU consumer protection, substances of human origin, tobacco control and patient’s rights, cross-border health care; adopt a new strategy for the development of the health care system; ensure administrative capacities to implement the health acquis. | Align with the acquis on consumer protection and relevant services; enhance tobacco control by effectively implementing the EU acquis on this and by ratifying the Protocol to Eliminate Illicit Trade in Tobacco Products. | Ensure the necessary institutional/administrative/technical capacity to implement the health acquis; further align EU acquis on substances of human origin on patients’ rights in cross-border health care on tobacco control and on medicines for human and veterinary use. |
| Persuasion | NA | NA | NA | NA | NA | NA |
| Policy areas . | Country-specific recommended actions . | |||||
|---|---|---|---|---|---|---|
| Albania . | Bosnia and Herzegovina . | Kosovo . | Montenegro . | North Macedonia . | Serbia . | |
| Financing | Increase the financial/human resources in the sector, in particular in Primary Health Care. | NA | Increase financial/human resources for health sector reforms and electronic health information systems, notably for Roma and Ashkali communities. | NA | Ensure funding and specialized knowledge for the early detection of cancer and rare diseases. | Strengthen the financial sustainability of the public health insurance fund and of the authorities for consumer protection, market surveillance and sanitary inspection. |
| Payment | NA | NA | NA | NA | NA | NA |
| Organization | Strengthen all-hazard health emergency preparedness response and data quality; equal access/quality health services for vulnerable. | Strengthen health institutions in the provision of health services for Roma and Ashkali. | Implement the national programme on early detection of cancer. | Strengthen managerial sustainability of the public health insurance fund and of the relevant authorities for consumer protection, market surveillance and sanitary inspection. | ||
| Regulation | Align with the acquis on substances of human origin. medicines for human and veterinary use. and tobacco control and accede to the World Health Organization’s Framework Convention Protocol to eliminate illicit trade in tobacco products. | Adopt and enforce legislation prohibiting smoking in public places; protocol to eliminate illicit trade in tobacco; align with the acquis on: substances of human origin. and medicines for human use to ensure oversight/coordination; align with the acquis consumer protection laws and cross-border health threats including communicable diseases. | Further alignment of consumer protection law partly with EU acquis; ensure the rigorous implementation of tobacco control in line with the relevant EU acquis and international obligations. | Continue to align with the acquis on health protection. EU consumer protection, substances of human origin, tobacco control and patient’s rights, cross-border health care; adopt a new strategy for the development of the health care system; ensure administrative capacities to implement the health acquis. | Align with the acquis on consumer protection and relevant services; enhance tobacco control by effectively implementing the EU acquis on this and by ratifying the Protocol to Eliminate Illicit Trade in Tobacco Products. | Ensure the necessary institutional/administrative/technical capacity to implement the health acquis; further align EU acquis on substances of human origin on patients’ rights in cross-border health care on tobacco control and on medicines for human and veterinary use. |
| Persuasion | NA | NA | NA | NA | NA | NA |
Notes: NA, not available.
Data source: European Commission. 2022.3–8
In addition to the above, we analyze the change or the absence of a change in the relevant health system performance outcomes through selected public health indicators and provide evidence for the convergence or divergence towards the average EU15 indicators across the six WBCs from 2000 to 2019.
Health data for this study are drawn from the World Health Organization Health for All Database (HFA-DB) for 2000 and 2019.20 When data were missing for those years, we took the closest data available, which is noted. In the absence of Kosovo’s data from the HFA-DB, the data are derived from the Kosovo Agency of Statistics,21 World Bank,22 Global Fund,23 published research24,25 and institutional reviews.26
Consulting the published literature,27 considering EC-recommended public health actions and the contextual pervasive socio-economic factors on health,3–8 we select 19 key relevant public health indicators. The indicators are grouped into four categories: population health indicators include general health indicators (life expectancy and neonatal deaths), mortality rates for common diseases and conditions (circulatory system diseases, malignant neoplasm, external causes, suicides), the incidence of infectious diseases (TB and AIDS) and primary prevention avoidable deaths (death rates caused by traffic accidents, respiratory system cancers, chronic liver diseases and smoking prevalence). Health expenditure indicators include public health expenditure as a percentage of gross domestic product (GDP), total health expenditure, and household out-of-pocket spending as a share of total health spending. While the number of health professionals includes the number of doctors and nurses per 100 000 population. On 18 of 19 selected indicators, σ convergence is measured using the coefficient of variation as the standard measure of dispersion for a quantitative chosen variable. The coefficient of variation is estimated as the standard deviation divided by the mean. Since standard deviation can overlook some forms of convergence, Plümper and Schneider28 recommend using the standard deviation alone, not divided by the mean. Therefore, in this paper, we present both measures. Convergence towards EU15 average selected morbidity and mortality indicators is shown when the difference between country-selected indicators’ coefficient of variation was minor in 2019 compared with 2000, and divergence when the latter was major.27 The EU15 member states represent the EU as the founding members before the enlargement, before May 2004, and EU27 after May 2004.20
No ethical approval was obtained since only data from publicly available sources were used.
Results
Towards European Health Care Policies
The health care reforms in WBCs aimed to create modern public health systems focusing on health promotion and prevention of non-communicable and communicable diseases within financially sustainable performing health systems.3–8 Table 1 presents the country-specific central EC-recommended public health actions structured into five health policy areas. Financing and regulation represent the bulk of EC-recommended health policy areas with specific activities relevant to the WBCs’ EU accession. In contrast, no particular activities were recommended for payment and persuasion. In the health financing policy area, Albania and Kosovo were recommended to increase public health financing and human resources, and Serbia was advised to strengthen the financial sustainability of its public health insurance fund. Regarding health system organization, Albania and Kosovo were urged to support health service provision for vulnerable groups, respectively, Roma and Ashkali. In terms of regulation, all WBCs were recommended to strengthen their capacities to align their legislation fully with the acquis. The EC urged the following aspects of public health protection for priority attention of the WBC governments: illicit tobacco trade, the safety of substances of human origin, humans and veterinary medicines, patients’ rights in cross-border health care, and cross-border health threats, including infectious diseases.3–8
Towards European Health Status
In 2000, WBCs shared common public health challenges such as lower life expectancy, higher neonatal death rates, increased deaths caused by injury and poisoning, and suicide rates (Kosovo data are missing). TB rates ranged from five times the EU15 average in Kosovo to the lowest 1.4 times reported in North Macedonia (table 2); TB incidence varied across the six countries, but none of the countries was uniformly better than the other five countries. Death rates caused by traffic accidents indicated increased trends in Albania and Kosovo, 2.4, respectively, 1.8 times the EU15 average. In the same period, Serbia showed a slight decrease, but death rates remained 1.4 times the EU15 average. All six countries were worse in most public health indicators. Namely, life expectancy at birth, SDR for circulatory diseases, malignant neoplasms including tracheal bronchus, and lung cancer, traffic accidents, psychoactive substance use, tuberculosis incidence, and tobacco smoking prevalence were worse than the EU15 average. The exceptions were for death rates caused by chronic liver disease, including cirrhosis, and external causes of injury and poisoning (table 2).
| . | Albania . | Bosnia and Herzegovina . | Kosovo . | Montenegro . | North Macedonia . | Serbia . | EU15a . | EU27 . |
|---|---|---|---|---|---|---|---|---|
| Selected general health indicators | ||||||||
| Life expectancy at birth (years) | 75.1/79.6b | 76.7b/76.3b | 74.0/79.0 | 74.1/79.3 | 73.2/76.7 | 71.7/76.1 | 78.8/81.8b | 77.4/81.5 |
| Male | 72.2/77.5b | NA/73.8b | 72.4/76.7 | 71.5/79.3 | 71.1/72.2 | 69.0/71.6 | 75.6/79.3b | 74.1/78.8b |
| Female | 78.2/b81.9 | NA/78.7b | 75.8/81.3 | 76.73/81.4b | 75.5/76.7 | 74.5/77.5 | 81.8/84.1b | 80.7/84.1b |
| Neonatal deaths per 1000 live births | 5.0/2.4b | 5.0b/4.7b | 27.6/8.3 | 7.3b/4.1b | 8.6/7.7b | 7.7/3.8 | 3.1/2.3b | 3.8/2.5 |
| SDR per 100 000 | ||||||||
| Disease of circulatory system | 475.4/353.1b | 426.6b/446.4b | 229.7b/221.7 | 516.1/175.7 | 614.6/346.8 | 657.0/373.8 | 245.3/134.7b | 310.8/167.2 |
| Malignant neoplasm | 124.6/91.0b | 156.8b/173.0b | NA/NA | 144.5/148.0 | 165.6/149.2 | 189.1/191.9 | 182.5/147.5b | 188.6/151.9 |
| External causes of injury/poisoning | 46.4/31.8b | 28.1b/26.4b | NA/NA | 40.2/23.6 | 38.4/20.0 | 49.2/30.4 | 39.1/30.4b | 46.2/32.7 |
| Suicide and self-inflicted injury | 2.0/5.6b | 0.1b/7.2b | NA/NA | 18.5b/4.7 | 7.6/4.6 | 17.9/10.4 | 10.4/8.5b | 12.0/8.9 |
| Infectious diseases | ||||||||
| TB incidence cases per 100 000 | 19.4/14.4 | 65.6/16.9 | 48.5b/33.8b | 25.0b/12.9 | 31.6/9.6 | 43.11b/15.8 | 11.57/6.7 | 20.23/9.4 |
| AIDS incidence cases per 100 000 | 0.1/1.4 | 0.1/0.2 | 0.17b/0.1b | 0.8/1.6 | 0.3/0.2b | 1.1/1.05 | 2.8/0.5 | 2.3/0.6 |
| Primary prevention | ||||||||
| SDR, motor vehicle/traffic accidents | 1.7/8.8b | 0.1b/0.1b | 10.1b/6.5 | 4.5b/1.5 | 5.3/1.8 | 7.0/5.1 | 10.1/3.6b | 11.0/4.2 |
| SDR, tracheal bronchus and lung cancer | 30.4/22.2b | 39.1b/39.4b | NA/NA | 43.3/34.5 | 33.1/33.9 | 42.0/48.4 | 37.3/31.8b | 39.3/32.7 |
| SDR, chronic liver disease and cirrhosis | 0.03b/6.6b | 7.63b/7.3b | NA/NA | 0.74/5.5 | 7.21/6.4 | 10.41/7.5 | 12.73/8.2b | 15.86/10.8 |
| SDR, Psychoactive substance use | 0.26/0.1 b | 1.53 b/1.6 b | NA/NA | 0.74/0.5 | 1.23/1.1 | 3.1/2.9 | 3,88/2,7 b | 3.73/2.9 |
| Tobacco prevalence smoking ≥15 years | 35.0/23.0 | 46.6/35.5 | NA/NA | 38.7/31.8 | NA/NA | 31.8/40.1 | 35.0/23.8 | 35.6/25.2 |
| Health expenditure | ||||||||
| Public HE as % of GDP | 2.3/2.9b | 4.0/6.8b | 3.0b/3.1 | 5.2/3.7b | 4.8/4.4b | 4.3/6.4b | 6.5/7.9b | 6.0/7.3b |
| Public HE as % of THE | 7.1/9.4b | 11.3/14.1b | NA/NA | 16.9/9.8b | 15.0/12.9b | 13.6/13.9b | 14.6/16.2b | 13.6/15.3b |
| OOP on health as % THE | 63.8/49.9b | 43.1/27.9b | 33.3b/28.9b | 29.0/42.8b | 43.8/36.7b | 29.5/36.6b | 15.6/14.9b | 17.6/16.7 |
| Health professionals | ||||||||
| Nurses per 100 000 | 506.2b/NA | 477.1b/559.3b | NA/552.6b | 530.9b/534.7b | 357.8/421.1b | 592.0b/628.8b | 837.2/934.8b | 779.4/867.6b |
| Physicians per 100 000 | 138.9/128.0b | 144.6/187.9b | NA/238.4 | 192.7b/234.3b | 219.9/280.0b | 274.7b/307.1b | 305.7/368.6b | 293.8/350.8b |
| . | Albania . | Bosnia and Herzegovina . | Kosovo . | Montenegro . | North Macedonia . | Serbia . | EU15a . | EU27 . |
|---|---|---|---|---|---|---|---|---|
| Selected general health indicators | ||||||||
| Life expectancy at birth (years) | 75.1/79.6b | 76.7b/76.3b | 74.0/79.0 | 74.1/79.3 | 73.2/76.7 | 71.7/76.1 | 78.8/81.8b | 77.4/81.5 |
| Male | 72.2/77.5b | NA/73.8b | 72.4/76.7 | 71.5/79.3 | 71.1/72.2 | 69.0/71.6 | 75.6/79.3b | 74.1/78.8b |
| Female | 78.2/b81.9 | NA/78.7b | 75.8/81.3 | 76.73/81.4b | 75.5/76.7 | 74.5/77.5 | 81.8/84.1b | 80.7/84.1b |
| Neonatal deaths per 1000 live births | 5.0/2.4b | 5.0b/4.7b | 27.6/8.3 | 7.3b/4.1b | 8.6/7.7b | 7.7/3.8 | 3.1/2.3b | 3.8/2.5 |
| SDR per 100 000 | ||||||||
| Disease of circulatory system | 475.4/353.1b | 426.6b/446.4b | 229.7b/221.7 | 516.1/175.7 | 614.6/346.8 | 657.0/373.8 | 245.3/134.7b | 310.8/167.2 |
| Malignant neoplasm | 124.6/91.0b | 156.8b/173.0b | NA/NA | 144.5/148.0 | 165.6/149.2 | 189.1/191.9 | 182.5/147.5b | 188.6/151.9 |
| External causes of injury/poisoning | 46.4/31.8b | 28.1b/26.4b | NA/NA | 40.2/23.6 | 38.4/20.0 | 49.2/30.4 | 39.1/30.4b | 46.2/32.7 |
| Suicide and self-inflicted injury | 2.0/5.6b | 0.1b/7.2b | NA/NA | 18.5b/4.7 | 7.6/4.6 | 17.9/10.4 | 10.4/8.5b | 12.0/8.9 |
| Infectious diseases | ||||||||
| TB incidence cases per 100 000 | 19.4/14.4 | 65.6/16.9 | 48.5b/33.8b | 25.0b/12.9 | 31.6/9.6 | 43.11b/15.8 | 11.57/6.7 | 20.23/9.4 |
| AIDS incidence cases per 100 000 | 0.1/1.4 | 0.1/0.2 | 0.17b/0.1b | 0.8/1.6 | 0.3/0.2b | 1.1/1.05 | 2.8/0.5 | 2.3/0.6 |
| Primary prevention | ||||||||
| SDR, motor vehicle/traffic accidents | 1.7/8.8b | 0.1b/0.1b | 10.1b/6.5 | 4.5b/1.5 | 5.3/1.8 | 7.0/5.1 | 10.1/3.6b | 11.0/4.2 |
| SDR, tracheal bronchus and lung cancer | 30.4/22.2b | 39.1b/39.4b | NA/NA | 43.3/34.5 | 33.1/33.9 | 42.0/48.4 | 37.3/31.8b | 39.3/32.7 |
| SDR, chronic liver disease and cirrhosis | 0.03b/6.6b | 7.63b/7.3b | NA/NA | 0.74/5.5 | 7.21/6.4 | 10.41/7.5 | 12.73/8.2b | 15.86/10.8 |
| SDR, Psychoactive substance use | 0.26/0.1 b | 1.53 b/1.6 b | NA/NA | 0.74/0.5 | 1.23/1.1 | 3.1/2.9 | 3,88/2,7 b | 3.73/2.9 |
| Tobacco prevalence smoking ≥15 years | 35.0/23.0 | 46.6/35.5 | NA/NA | 38.7/31.8 | NA/NA | 31.8/40.1 | 35.0/23.8 | 35.6/25.2 |
| Health expenditure | ||||||||
| Public HE as % of GDP | 2.3/2.9b | 4.0/6.8b | 3.0b/3.1 | 5.2/3.7b | 4.8/4.4b | 4.3/6.4b | 6.5/7.9b | 6.0/7.3b |
| Public HE as % of THE | 7.1/9.4b | 11.3/14.1b | NA/NA | 16.9/9.8b | 15.0/12.9b | 13.6/13.9b | 14.6/16.2b | 13.6/15.3b |
| OOP on health as % THE | 63.8/49.9b | 43.1/27.9b | 33.3b/28.9b | 29.0/42.8b | 43.8/36.7b | 29.5/36.6b | 15.6/14.9b | 17.6/16.7 |
| Health professionals | ||||||||
| Nurses per 100 000 | 506.2b/NA | 477.1b/559.3b | NA/552.6b | 530.9b/534.7b | 357.8/421.1b | 592.0b/628.8b | 837.2/934.8b | 779.4/867.6b |
| Physicians per 100 000 | 138.9/128.0b | 144.6/187.9b | NA/238.4 | 192.7b/234.3b | 219.9/280.0b | 274.7b/307.1b | 305.7/368.6b | 293.8/350.8b |
| . | Albania . | Bosnia and Herzegovina . | Kosovo . | Montenegro . | North Macedonia . | Serbia . | EU15a . | EU27 . |
|---|---|---|---|---|---|---|---|---|
| Selected general health indicators | ||||||||
| Life expectancy at birth (years) | 75.1/79.6b | 76.7b/76.3b | 74.0/79.0 | 74.1/79.3 | 73.2/76.7 | 71.7/76.1 | 78.8/81.8b | 77.4/81.5 |
| Male | 72.2/77.5b | NA/73.8b | 72.4/76.7 | 71.5/79.3 | 71.1/72.2 | 69.0/71.6 | 75.6/79.3b | 74.1/78.8b |
| Female | 78.2/b81.9 | NA/78.7b | 75.8/81.3 | 76.73/81.4b | 75.5/76.7 | 74.5/77.5 | 81.8/84.1b | 80.7/84.1b |
| Neonatal deaths per 1000 live births | 5.0/2.4b | 5.0b/4.7b | 27.6/8.3 | 7.3b/4.1b | 8.6/7.7b | 7.7/3.8 | 3.1/2.3b | 3.8/2.5 |
| SDR per 100 000 | ||||||||
| Disease of circulatory system | 475.4/353.1b | 426.6b/446.4b | 229.7b/221.7 | 516.1/175.7 | 614.6/346.8 | 657.0/373.8 | 245.3/134.7b | 310.8/167.2 |
| Malignant neoplasm | 124.6/91.0b | 156.8b/173.0b | NA/NA | 144.5/148.0 | 165.6/149.2 | 189.1/191.9 | 182.5/147.5b | 188.6/151.9 |
| External causes of injury/poisoning | 46.4/31.8b | 28.1b/26.4b | NA/NA | 40.2/23.6 | 38.4/20.0 | 49.2/30.4 | 39.1/30.4b | 46.2/32.7 |
| Suicide and self-inflicted injury | 2.0/5.6b | 0.1b/7.2b | NA/NA | 18.5b/4.7 | 7.6/4.6 | 17.9/10.4 | 10.4/8.5b | 12.0/8.9 |
| Infectious diseases | ||||||||
| TB incidence cases per 100 000 | 19.4/14.4 | 65.6/16.9 | 48.5b/33.8b | 25.0b/12.9 | 31.6/9.6 | 43.11b/15.8 | 11.57/6.7 | 20.23/9.4 |
| AIDS incidence cases per 100 000 | 0.1/1.4 | 0.1/0.2 | 0.17b/0.1b | 0.8/1.6 | 0.3/0.2b | 1.1/1.05 | 2.8/0.5 | 2.3/0.6 |
| Primary prevention | ||||||||
| SDR, motor vehicle/traffic accidents | 1.7/8.8b | 0.1b/0.1b | 10.1b/6.5 | 4.5b/1.5 | 5.3/1.8 | 7.0/5.1 | 10.1/3.6b | 11.0/4.2 |
| SDR, tracheal bronchus and lung cancer | 30.4/22.2b | 39.1b/39.4b | NA/NA | 43.3/34.5 | 33.1/33.9 | 42.0/48.4 | 37.3/31.8b | 39.3/32.7 |
| SDR, chronic liver disease and cirrhosis | 0.03b/6.6b | 7.63b/7.3b | NA/NA | 0.74/5.5 | 7.21/6.4 | 10.41/7.5 | 12.73/8.2b | 15.86/10.8 |
| SDR, Psychoactive substance use | 0.26/0.1 b | 1.53 b/1.6 b | NA/NA | 0.74/0.5 | 1.23/1.1 | 3.1/2.9 | 3,88/2,7 b | 3.73/2.9 |
| Tobacco prevalence smoking ≥15 years | 35.0/23.0 | 46.6/35.5 | NA/NA | 38.7/31.8 | NA/NA | 31.8/40.1 | 35.0/23.8 | 35.6/25.2 |
| Health expenditure | ||||||||
| Public HE as % of GDP | 2.3/2.9b | 4.0/6.8b | 3.0b/3.1 | 5.2/3.7b | 4.8/4.4b | 4.3/6.4b | 6.5/7.9b | 6.0/7.3b |
| Public HE as % of THE | 7.1/9.4b | 11.3/14.1b | NA/NA | 16.9/9.8b | 15.0/12.9b | 13.6/13.9b | 14.6/16.2b | 13.6/15.3b |
| OOP on health as % THE | 63.8/49.9b | 43.1/27.9b | 33.3b/28.9b | 29.0/42.8b | 43.8/36.7b | 29.5/36.6b | 15.6/14.9b | 17.6/16.7 |
| Health professionals | ||||||||
| Nurses per 100 000 | 506.2b/NA | 477.1b/559.3b | NA/552.6b | 530.9b/534.7b | 357.8/421.1b | 592.0b/628.8b | 837.2/934.8b | 779.4/867.6b |
| Physicians per 100 000 | 138.9/128.0b | 144.6/187.9b | NA/238.4 | 192.7b/234.3b | 219.9/280.0b | 274.7b/307.1b | 305.7/368.6b | 293.8/350.8b |
| . | Albania . | Bosnia and Herzegovina . | Kosovo . | Montenegro . | North Macedonia . | Serbia . | EU15a . | EU27 . |
|---|---|---|---|---|---|---|---|---|
| Selected general health indicators | ||||||||
| Life expectancy at birth (years) | 75.1/79.6b | 76.7b/76.3b | 74.0/79.0 | 74.1/79.3 | 73.2/76.7 | 71.7/76.1 | 78.8/81.8b | 77.4/81.5 |
| Male | 72.2/77.5b | NA/73.8b | 72.4/76.7 | 71.5/79.3 | 71.1/72.2 | 69.0/71.6 | 75.6/79.3b | 74.1/78.8b |
| Female | 78.2/b81.9 | NA/78.7b | 75.8/81.3 | 76.73/81.4b | 75.5/76.7 | 74.5/77.5 | 81.8/84.1b | 80.7/84.1b |
| Neonatal deaths per 1000 live births | 5.0/2.4b | 5.0b/4.7b | 27.6/8.3 | 7.3b/4.1b | 8.6/7.7b | 7.7/3.8 | 3.1/2.3b | 3.8/2.5 |
| SDR per 100 000 | ||||||||
| Disease of circulatory system | 475.4/353.1b | 426.6b/446.4b | 229.7b/221.7 | 516.1/175.7 | 614.6/346.8 | 657.0/373.8 | 245.3/134.7b | 310.8/167.2 |
| Malignant neoplasm | 124.6/91.0b | 156.8b/173.0b | NA/NA | 144.5/148.0 | 165.6/149.2 | 189.1/191.9 | 182.5/147.5b | 188.6/151.9 |
| External causes of injury/poisoning | 46.4/31.8b | 28.1b/26.4b | NA/NA | 40.2/23.6 | 38.4/20.0 | 49.2/30.4 | 39.1/30.4b | 46.2/32.7 |
| Suicide and self-inflicted injury | 2.0/5.6b | 0.1b/7.2b | NA/NA | 18.5b/4.7 | 7.6/4.6 | 17.9/10.4 | 10.4/8.5b | 12.0/8.9 |
| Infectious diseases | ||||||||
| TB incidence cases per 100 000 | 19.4/14.4 | 65.6/16.9 | 48.5b/33.8b | 25.0b/12.9 | 31.6/9.6 | 43.11b/15.8 | 11.57/6.7 | 20.23/9.4 |
| AIDS incidence cases per 100 000 | 0.1/1.4 | 0.1/0.2 | 0.17b/0.1b | 0.8/1.6 | 0.3/0.2b | 1.1/1.05 | 2.8/0.5 | 2.3/0.6 |
| Primary prevention | ||||||||
| SDR, motor vehicle/traffic accidents | 1.7/8.8b | 0.1b/0.1b | 10.1b/6.5 | 4.5b/1.5 | 5.3/1.8 | 7.0/5.1 | 10.1/3.6b | 11.0/4.2 |
| SDR, tracheal bronchus and lung cancer | 30.4/22.2b | 39.1b/39.4b | NA/NA | 43.3/34.5 | 33.1/33.9 | 42.0/48.4 | 37.3/31.8b | 39.3/32.7 |
| SDR, chronic liver disease and cirrhosis | 0.03b/6.6b | 7.63b/7.3b | NA/NA | 0.74/5.5 | 7.21/6.4 | 10.41/7.5 | 12.73/8.2b | 15.86/10.8 |
| SDR, Psychoactive substance use | 0.26/0.1 b | 1.53 b/1.6 b | NA/NA | 0.74/0.5 | 1.23/1.1 | 3.1/2.9 | 3,88/2,7 b | 3.73/2.9 |
| Tobacco prevalence smoking ≥15 years | 35.0/23.0 | 46.6/35.5 | NA/NA | 38.7/31.8 | NA/NA | 31.8/40.1 | 35.0/23.8 | 35.6/25.2 |
| Health expenditure | ||||||||
| Public HE as % of GDP | 2.3/2.9b | 4.0/6.8b | 3.0b/3.1 | 5.2/3.7b | 4.8/4.4b | 4.3/6.4b | 6.5/7.9b | 6.0/7.3b |
| Public HE as % of THE | 7.1/9.4b | 11.3/14.1b | NA/NA | 16.9/9.8b | 15.0/12.9b | 13.6/13.9b | 14.6/16.2b | 13.6/15.3b |
| OOP on health as % THE | 63.8/49.9b | 43.1/27.9b | 33.3b/28.9b | 29.0/42.8b | 43.8/36.7b | 29.5/36.6b | 15.6/14.9b | 17.6/16.7 |
| Health professionals | ||||||||
| Nurses per 100 000 | 506.2b/NA | 477.1b/559.3b | NA/552.6b | 530.9b/534.7b | 357.8/421.1b | 592.0b/628.8b | 837.2/934.8b | 779.4/867.6b |
| Physicians per 100 000 | 138.9/128.0b | 144.6/187.9b | NA/238.4 | 192.7b/234.3b | 219.9/280.0b | 274.7b/307.1b | 305.7/368.6b | 293.8/350.8b |
All WBCs spent fewer public shares of their GDPs than the EU15 average, except for Bosnia and Herzegovina and Serbia, which were comparable to the EU15. All countries reported decreased out-of-pocket health spending shares except for Serbia and Montenegro. Out-of-pocket health spending in all WBCs remained higher as compared with EU15 shares.
The number of nurses and physicians during the study period has increased in all WBCs. However, the number of physicians and nurses remains low compared with the EU15 levels.
From 2000 to 2019, nine out of 18 analyzed selected public health indicators showed divergence (Supplementary Appendix table S1), and the other nine indicators showed convergence to the EU15 averages (Supplementary Appendix table S2). TB incidence, bronchus, trachea and lung cancer SDR, and health expenditure as a percentage of GDP, are the health indicators with the most divergent coefficients of variation (CV) between 2000 and 2019 (figure 1). Meanwhile, the number of health professionals (physicians and nurses) and SDR from external causes of injury/poisoning are the health indicators with the most convergent CV during the study period (figure 2).
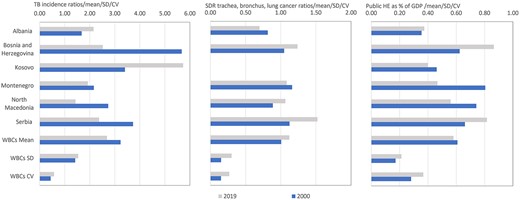
The WBC ratios to the EU15 public health indicators with the three most divergent CV, 2000 and 2019. Note: EU15, the 15 Member States of the European Union prior to the May 2004 enlargement; HE, health expenditure; SDR, standard mortality rate per 100 000. Missing bars, data not available.
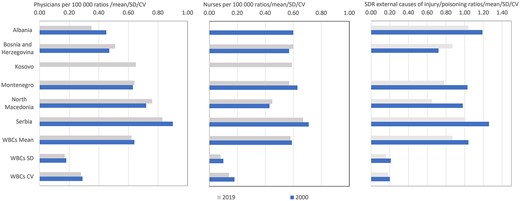
The WBC ratios to the EU15 public health indicators with the three most convergent CV, 2000 and 2019. Note: EU15—the 15 Member States of the European Union prior to the May 2004 enlargement; SDR, standard mortality rate per 100 000. Missing bars, data not available.
Discussion
A decade before the study period, the WBCs were faced with a series of severe conflicts in the region. In the aftermath of these conflicts, during the study period, WBCs focused on macroeconomic stabilization and growth, prioritizing employment generation, efficiency, and sustainability of public spending to improve health and well-being.16 To this end, health system reforms in WBCs faced similar challenges, resulting in broadly similar health systems with particular requirements. Our study documents that to fulfil the EC health policy’s required stipulations, each WBC is expected to follow considerable, clear-cut, specific EC-recommended actions, primarily focusing on health financing and regulation. The findings of this study offer an alternative descriptive analytical approach to the limited published literature on measuring the change in WBCs’ health outcomes in the light of EC-recommended health policy areas relevant to EU accession.
Although the data for this study are drawn from sources considered accurate and reliable, they should be interpreted only as indicative of general trends and major differences across WBCs and those of the EU15 member states rather than providing precise quantitative difference measures. To this end, the study results indicate additional attention in further improving life expectancy, reducing neonatal deaths, prioritizing primary prevention programmes in reducing death rates from circulatory diseases and malignant neoplasms, including trachea bronchus and lung cancer, traffic accidents, psychoactive substance use, tuberculosis incidence, and tobacco smoking prevalence. This is in line with the critical actions recommended by the EC.3–8 Further, this descriptive-analytical study findings demonstrate that the implementation of the EC-recommended priority health policy areas/actions could also be followed by readily available selected health indicators evaluating catch-up to the EU15 average levels, easily understandable for national policymakers, academia and other relevant stakeholders including the citizens of the WBCs.
Evidence from this study indicates that from 2000 to 2019, WBCs’ citizens paid more, and their governments paid less for health care. Albania, Kosovo, Montenegro, and North Macedonia governments spent less than at least the recommended 5% of their GDPs on health.29 The exception was the Bosnia and Herzegovina government, which reached the second-best-at least recommended level (6–7%) for public-sector expenditure as a percentage of GDP.30 Private households' out-of-pocket payments on health as % of total health expenditure indicated a catch-up to the EU15 average; however, this percentage for all WBCs remained higher than WHO recommended 15–20% when aiming to reduce catastrophic health expenditure at a negligible level.31 To this end, the study findings concur with the country-specific EC recommendations to improve health financing levels and systems in the WBCs.3,5,8
Although our study indicates an increasing trend in health care professional rates and, subsequently, convergence towards the EU15 levels, this finding deserves special attention. First, the number of health care professionals remains lower than the EU15 average. Second, this may be exacerbated by the latest increased health care workforce migration from the WBCs, mainly to the EU countries and Switzerland, the USA and Canada.32 Published data indicate that health and elderly care professions are becoming more in demand, and most of the health professionals from the accession states are likely to be relatively young and educationally well qualified.33 Learning from the previous regional experiences,34 WBCs as ‘source’ and EU countries as ‘destination’ may want to manage health workforce migration at national organizational and international levels so that both parties win, or at least one does not exclusively lose. Therefore, in line with the EC recommentations3,5 and the sustainable development agenda,35 addressing an increase in health human resources in WBCs, particularly for Albania and Kosovo, deserves attention.
There is mixed evidence of the WBCs’ progress towards EU health and health care policies. From 2000 to 2019, in WBCs, nine out of 18 analyzed selected public health indicators showed divergence, while the other nine indicators converged to the EU15 averages. The study findings suggest that desired progress remains elusive in both domains. This underscores the importance of closely monitoring the main country-specific selected health indicators associated with EC-recommended health policy areas critical to the EU accession health policy dimension.
Supplementary data
Supplementary data are available at EURPUB online.
Acknowledgements
The authors thank Prof. Rachel Vincente for her valuable comments on the paper.
Funding
This work did not receive specific funding.
Conflicts of interest: None declared.
Author contributions
F.A.Q. and M.B. jointly developed and agreed on the concept for this paper. F.A.Q. was responsible for data analysis and led writing; both authors reviewed and edited drafts, finalized the manuscript, and approved it for submission.
Data availability
The authors confirm that all data supporting the findings of this study are publicly available.3–8,20–26 The datasets used and analyzed for this study are available from the corresponding author upon reasonable request.
For all WBCs, financing and regulation are the key priority areas for the health policy dimension of the EU accession.
Nine of 18 analyzed selected health indicators showed divergence, and the other nine converged towards the EU15 averages.
Despite some progress towards EU health and health care policies, WBCs continue facing diverse public health challenges. Desired progress remains challenging in both domains.
Measuring the WBCs’ progress or lack of progress in catching up to the EU15 average health levels represents an alternative monitoring approach towards EU health and health care policies.
References
United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. Available at: https://sdgs.un.org/2030agenda (3 April 2024, date last accessed).
- cancer
- traffic accidents
- albania
- bosnia-herzegovina
- cardiovascular system
- european union
- health expenditures
- health personnel
- health policy
- health status
- life expectancy
- macedonia (republic)
- persuasive communication
- public sector
- tuberculosis
- european continental ancestry group
- mortality
- public health medicine
- substance use disorders
- catching
- population health
- serbia
- tobacco smoking




Comments