-
PDF
- Split View
-
Views
-
Cite
Cite
Majd Al Deen Alhuarrat, Sumant Pargaonkar, Kusha Rahgozar, Israel Safiriyu, Xiadong Zhang, Robert T Faillace, Luigi Di Biase, Comparison of in-hospital outcomes and complications of left atrial appendage closure with the Watchman device between males and females, EP Europace, Volume 25, Issue 9, September 2023, euad228, https://doi.org/10.1093/europace/euad228
Close - Share Icon Share
Abstract
Left atrial appendage occlusion (LAAO) with WATCHMAN device is being used for patients with atrial fibrillation (AFB) and, as an off-label use, atrial flutter (AFL) who can't comply with long-term anticoagulation. We aim to study the differences in outcomes between sexes in patients undergoing Watchman device implantation.
The National Inpatient Sample was queried between 2016 and 2019 using ICD-10 clinical modification codes I48x for AFB and AFL. Patients who underwent LAAO were identified using the procedural code 02L73DK. Comorbidities and complications were identified using ICD procedure and diagnosis codes. Differences in primary outcomes were analyzed using multivariable regression and propensity score matching.
38 105 admissions were identified, of which 16 795 (44%) were females (76 ± 7.6 years) and 21 310 (56%) were males (75 ± 8 years). Females were more likely to have cardiac (frequencies: 5.8% vs 3.75%, aOR: 1.5 [1.35-1.68], p1 day inpatient (1.79 [1.67-1.93], P < 0.01) and be discharged to a facility (1.54 [1.33-1.80], P < 0.01).
Females are more likely to develop cardiac, renal, bleeding, pulmonary and TEE-related complications following LAAO procedure, while concurrently showing higher mortality, length of stay and discharge to facilities.
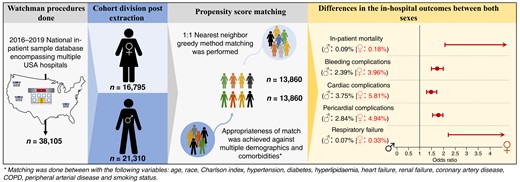
Figure summarizing the most important methodology and result points of our research.
Introduction
Traditionally, oral anticoagulation (OAC) has been the mainstay of stroke prevention among atrial fibrillation (AFB) patients with high CHA2DS2-VASc scores. However, a considerable number of patients are not appropriate candidates for long-term OAC.1 Accordingly, the percutaneous left atrial appendage occlusion (LAAO) procedure has emerged as an alternative for stroke prevention among a specific sample of such patients.2 Certain cardiac procedures have been associated with higher complications in females compared to males.3 For the LAAO procedure, the initial PROTECT-AF trial had a high complication rate, which decreased during the subsequent PREVAIL-AF trial. In both studies, subgroup analysis did not reveal differences in composite endpoints of efficacy and stroke reduction between the two sexes.4,5 However, differences in periprocedural complications were not studied. Later, a subanalysis of the Amulet IDE trial was able to show a higher incidence of major in-hospital adverse events in women driven by major bleeding and pericardial effusion requiring intervention.6 In this research, we sought to utilize a large national database to provide the latest data on sex differences in periprocedural outcomes among patients undergoing LAAO in the USA.
Methods
Our sample of Watchman device insertions was derived from the National Inpatient Sample (NIS) database (Graphical Abstract). We queried the NIS from 2016 to 2019 and identified a cohort of patients who underwent LAAO per the International Classification of Diseases (ICD) coding (02L73DK). Noteworthy is that Amulet LAAO devices are likely not within our sample since they were approved in 2021. To streamline the cohort and decrease variables confounding our primary outcomes, only the patients who had a discharge primary diagnosis of AFB and atrial flutter (AFL) were included in our sample (I48.x). Atrial flutter was included as an off-label use and secondary to the fact that AFB may have concurrent AFL. Patients who had any of the following were excluded: concomitant ablation procedure in the same admission, any type of coronary revascularization (stenting, bypass procedure, and thrombolysis) during the same admission, and those missing any of the primary outcomes or classification of sex. Through applying ICD-10 codes in all procedure and diagnosis fields, comorbidities and complications were identified, and as applicable, only codes signifying initial encounters were used in the analysis, excluding subsequent encounter codes. All analysis was performed using STATA, version 17.0 (StataCorp LLC, Lakeway Drive, TX). Categorical data are presented as percentages, while continuous data are displayed as mean ± SD. A multivariable logistic regression model was used to calculate the adjusted odds ratio (OR) of in-hospital outcomes between sexes. The model included the following comorbidities: diabetes mellitus, hypertension, hyperlipidaemia, chronic ischaemic heart disease, peripheral vascular disease, chronic obstructive pulmonary disease, smoking status, peripheral artery disease, heart failure (of any severity), renal disease (of any severity), Charlson’s comorbidity index, age, and race. Propensity score matching was also carried out using a greedy matching algorithm and a calliper of 0.05.
Results
In-hospital mortality was higher in females only after propensity score matching with an adjusted post-match odds ratio (aOR) of 5 and a 95% confidence interval (CI) of 1.91–13.1 (P < 0.01) (Table 1). Periprocedural bleeding, anaemia, and requirement of blood transfusions (represented as bleeding complications; OR: 1.82, CI: 1.6–2.05, P < 0.01), along with cardiac complications (OR: 1.56, P < 0.01) and acute kidney injury (OR: 1.33, CI: 1.16–1.54, P < 0.01), represented as renal complications, were more likely to occur in females, and this remained consistent post-propensity score matching (Table 1). Pulmonary complications were more likely to occur in females as well (aOR: 3.44, CI: 2.22–5.33, P < 0.01), driven by post-operative respiratory failure (post-OP RF) (aOR: 4.56, CI: 2.37–8.76, P < 0.01), iatrogenic injuries (combined incidence of post-operative or ventilator-associated pneumonia and other respiratory complications: aOR: 4.01, CI: 1.50–10.67, P < 0.01), and the need for pleural drainage procedures (aOR: 2.4, CI: 1.15–5.03, P = 0.02). Females were more likely to spend >1 day in-hospital (aOR: 1.79, CI: 1.67–1.93, P < 0.01) and to be discharged to a facility (short-term hospital, skilled nursing, intermediate care, and/or other type of facilities) rather than home (aOR: 1.54, CI: 1.33–1.80, P < 0.01). As for transoesophageal echo (TEE)–related complications, upper gastrointestinal (GI) bleeding was more likely to occur in females than males (aOR: 1.6, CI: 1.35–1.85, P < 0.01). Furthermore, the combined incidence of upper GI injuries (including oesophagitis, oesophageal injury/laceration, and throat/larynx injury) was more likely to occur in females (aOR: 4, CI: 1.5–10.67, P < 0.01).
Breakdown of primary outcomes with multivariate regression before and univariate regression after matching
 |
 |
Breakdown of primary outcomes with multivariate regression before and univariate regression after matching
 |
 |
Discussion
In concordance with Darden et al.’s7 analysis from the National Cardiovascular Data Registry on LAAO (NCDR-LAAO registry), our data show that there is a higher likelihood of pericardial effusion, haemopericardium, tamponade, and the need for pericardial intervention in females compared to males following LAAO while concurrently showing higher myocardial perforation incidence. Our study encompasses a time when Watchman FLX and Amulet devices were not introduced yet, bringing into question the applicability of the results nowadays. However, a comparison study including 144 patients undergoing either Watchman 2.5 or Watchman FLX showed no differences in the inpatient 7-day outcomes and complications between the treatment arms.8 Furthermore, an analysis of 1833 patients from the Amulet IDE trial showed a similar trend of a higher incidence of pericardial effusion requiring intervention among females as compared to males (2.0% vs. 0.5%),6 a rate similar to the pericardial interventions performed in our sample (1.91% vs. 0.56%). As such, though technological and procedural advances have occurred, they may have not optimally minimized pericardial outcome variation between sexes. As we advance in the field, device manufacturers must take this finding into consideration.
The higher rate of post-OP RF and iatrogenic injuries related to intubation among females undergoing LAAO seen in our analysis is a unique finding not previously described. Given that our data reveal that female patients tend to experience more periprocedural cardiac complications, it is reasonable to deduce that the mechanical ventilation and critical care interventions coinciding with these complications also occur at higher rates in female patients.
Moreover, albeit the low overall incidence, our analysis revealed that females were more likely to experience upper GI injuries such as oesophagitis, oesophageal injury/laceration, upper GI bleeding, and/or throat/larynx injury. Recent advances have resulted in intracardiac echocardiography (ICE) being used for LAAO closure.9 Frangieh et al.10 compared ICE to TEE in LAAO closure and found comparable efficacy with 100% success rates in both groups. Gianni et al.11 additionally noted a significant reduction in procedure time with ICE (−17 min, −26 to −9, P < 0.0001) among patients undergoing Watchman FLX implantation. Prospectively, with the increasing use of ICE, there could be a trend towards a decrease in TEE-related complications.
Funding
None declared.
Data availability
The data underlying this article are available in the National inpatient sample database at https://www.hcup-us.ahrq.gov/, and can be accessed by purchasing them directly from the HCUP website.
References
Author notes
Conflict of interest: L.D.B. is a consultant for Biosense Webster, Stereotaxis, and Rhythm Management and has received speaker honoraria/travel from Biosense Webster, St. Jude Medical (now Abbott), Boston Scientific, Medtronic, Biotronik, AtriCure, Baylis, and ZOLL.
- atrial fibrillation
- atrial flutter
- transesophageal echocardiography
- left auricular appendage
- comorbidity
- inpatients
- diagnosis
- heart
- mortality
- international classification of diseases
- off-label use
- percutaneous left atrial appendage occlusion device
- primary outcome measure
- left atrial appendage occlusion



