-
PDF
- Split View
-
Views
-
Cite
Cite
Fouad Khalil, Shilpkumar Arora, Ammar M Killu, Byomesh Tripathi, Christopher V DeSimone, Alexander Egbe, Peter A Noseworthy, Suraj Kapa, Siva Mulpuru, Bernard Gersh, Alkhouli Mohamad, Paul Friedman, David Holmes, Abhishek J Deshmukh, Utilization and procedural adverse outcomes associated with Watchman device implantation, EP Europace, Volume 23, Issue 2, February 2021, Pages 247–253, https://doi.org/10.1093/europace/euaa219
Close - Share Icon Share
Abstract
The Food and Drug Administration (FDA) approval of the Watchman device [percutaneous left atrial appendage occlusion (LAAO)] has resulted in the widespread use of this procedure in many centres across the USA. We sought to estimate the nationwide utilization and frequency of adverse outcomes associated with Watchman device implantation. The objective of this study was to evaluate the Watchman device implantation peri-procedural complications and comparison of the results with the previous studies.
The National Inpatient Sample (NIS) was queried for all hospitalizations with a primary diagnosis of atrial fibrillation or atrial flutter during the year 2016 with percutaneous LAAO during the same admission (ICD-10 code—02L73DK). The frequency of peri-procedural complications, including mortality, procedure-related stroke, major bleeding requiring blood transfusion, and pericardial effusion, was assessed. We compared the complication rates with the published randomized controlled trials and the European Watchman registry. An estimated 5175 LAAO procedures were performed in 2016. The majority of procedures was performed in males (59.1%), age ≥75 years (58.7%), and White (83.1%). The overall complication rate was 1.9%. The in-hospital mortality was 0.29%. Pericardial effusion requiring pericardiocentesis was the most frequent complication (0.68%). Bleeding requiring transfusion was noted in 0.1% of device implants. The rates of post-procedure stroke and systemic embolism were 0% and 0.29%, respectively.
Percutaneous LAAO with the Watchman device in the USA is associated with low in-hospital complications and a similar safety profile to a recently published EWOLUTION cohort. The complication rates were lower than those reported in the major randomized clinical trials (RCTs). We report the frequency of peri-procedural complications of the LAAO using the Watchman device from the NIS database. We also compare the frequency of peri-procedural complications with the previously published RCTs and EWOLUTION cohort. Our findings are in concordance with findings from EWOLUTION cohort and compare favourably with RCTs.
We present real-world data on the safety of the implant procedure that are necessary to create reasonable expectations of procedural risks and guidance for implanting centres.
Our findings regarding the safety of the Watchman device are in concordance with findings from EWOLUTION cohort.
We report a lower complications incidence compared with the previously published randomized clinical trials.
Our encouraging findings suggest increased experience amongst providers and reflect the maturation of technology and implant technique.
Introduction
Atrial fibrillation (AF) and AF-related strokes impose a major burden on patients and the society by contributing to increased morbidity and mortality and substantially to increased health care utilization and costs.1 The left atrial appendage (LAA) is thought to be implicated as the site of thrombus formation in >90% of strokes in AF patients.2 Thus, the LAA serves as an attractive anatomical target for closure to reduce stroke and systemic embolism.3 The Watchman device (Boston Scientific Corp., Marlborough, MA, USA) is the only approved left atrial appendage occlusion (LAAO) device in the USA, with an FDA approval for stroke prevention as an alternative to warfarin for selected patients with non-valvular AF.4 The goal is to reduce thromboembolic events and offer an alternative to anticoagulation therapy, especially in patients with absolute or relative contraindications for anticoagulation.
Initial promise for stroke prevention was noted in the Watchman Left Atrial Appendage System for Embolic Protection in Patients with AF (PROTECT-AF) trial. However, in this early experience with the device, the peri-procedural complication rate was not insignificant.5 The subsequent Watchman Left Atrial Appendage Closure device in patients with AF vs. long-term warfarin therapy (PREVAIL) trial and The Continued Access to PROTECT-AF (CAP) showed fewer complications as the experience of the implanting physicians increased.6 A more recent European registry, EWOLUTION, demonstrated a further reduction in peri-procedural complications compared with randomized clinical trials (RCTs).7
We examined the utilization and complications associated with Watchman implantation in the routine clinical practice in the USA and compared the complication rates with the RCTs and the registry data.
Methods
Our study cohort was derived from the National Inpatient Sample (NIS) database, a subset of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality. The NIS is the largest publicly available all-payer inpatient care database in the USA, including data on >7 million hospital stays per year, and is a stratified sample designed to ∼20% sample of US community (non-federal, short-term, general, and specialty) hospitals.8 National estimates are estimated using sampling weights provided by the sponsor. Annual data quality assessment of the NIS is performed to ensure the internal validity of the database. It is also validated with external data sources like the American Hospital Association Annual Survey Database, the National Hospital Discharge Survey from the National Center for Health Statistics, and the Medicare Provider Analysis and Review (MedPAR) inpatient data from the Centers for Medicare and Medicaid Services.9–11 This study was deemed exempt by the local IRB.
We identified hospitalizations associated with the ICD-10 diagnosis code for reporting AF or flutter with I48. Amongst this, we identified the Watchman implants, i.e. 02L73DK (occlusion of LAA with intraluminal device, percutaneous approach) from the year 2016. Specific ICD-10 code for Watchman implants was noted in ICD-10 codes. The NIS transitioned to ICD-10 codes from the fourth quarter of 2015, hence we chose 2016 for annual estimates. We included all hospitalizations of patients ≥18 years of age. We excluded all hospitalizations with missing age, sex, and in-hospital mortality status (Figure 1).
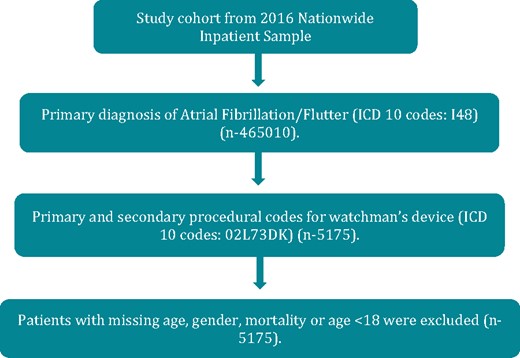
Diagram showing steps of patients inclusion using Nationwide Inpatient Sample. ICD, implantable cardioverter-defibrillator.
Patient-level characteristics, such as age, sex, race, median household income according to ZIP code, primary payer (Federal vs. Private insurance), admission type (elective vs. non-elective), day of admission (weekdays vs. weekend), and hospital-level characteristics, such as hospital location (urban vs. rural), hospital bed size (small/medium vs. large), hospital region (Northeast, Midwest or North Central, South, and West), and hospital teaching status (non-teaching vs. teaching), were provided by NIS. Specific comorbidities were identified by using a group of ICD-10 codes provided by HCUP12 (Supplementary material online, Table S1).
Specific comorbidities and CHA2DS2-VASc scores were assessed using appropriate ICD-10 codes for score-related comorbidities (Supplementary material online, Table S2). The cost was calculated by using cost to charge ratio provided by HCUP.
We investigated the commonly described acute, in-hospital complications associated with implantation of the Watchman device. The frequency of peri-procedural complications including mortality, stroke, major bleeding requiring a blood transfusion, and pericardial effusions was determined. These were assessed using the appropriate ICD-10 codes in the secondary diagnosis field (Supplementary material online, Table S3). We included these complications based on the frequency previously reported in the clinical literature and as a comparison to complications noted in the PREVAIL, PROTECT-AF, CAP, and the EVOLUTION data.
Statistical analysis
SAS 9.4 (SAS Institute Inc., Cary, NC, USA) were utilized for analyses. Weighted values of hospitalization-level observations were generated to produce a nationally representative estimate of the entire US population of hospitalized patients. Differences between categorical variables were tested using the χ2 test, and differences between continuous variables were tested using the Student’s t-test. We used the Cochran–Armitage test for categorical variables. P-values of <0.05 were considered statistically significant.
Results
Patient and procedural demographics
The baseline demographic characteristics are summarized in Table 1. Based on the NIS, 5175 LAAO procedures were performed in the USA in 2016. The majority of the implants was performed in individuals age ≥75 years (58.6%), males (59.1%), and Caucasians (83%). Hypertension (83.3%), coronary artery disease (48.2%), and diabetes mellitus (30.8%) were the three most common comorbidities. Most of these procedures were performed at large bed size (69.6%) and teaching hospitals (88.2%) in urban regions. Overall, 92.3% of the procedures were covered by federal insurance. The majority of patients (97%) was discharged home after the procedure, with only 2.6% requiring disposition to a different healthcare facility. The mean cost of hospitalization was $25 724 per procedure and an average length of stay was 1.36 ± 0.05 days (Table 1). The mean CHA2DS2-VASc score was 4.4 (Table 2).
| . | Overall (%), 5175 . | No complication (%) (n = 5075) . | Any complication (%) (n = 100) . | P-value . |
|---|---|---|---|---|
| Watchman device implantations | ||||
| Age (years) | 0.117 | |||
| 18–49 | 0.77 | 0.79 | 0.00 | |
| 50–64 | 7.54 | 7.59 | 5.00 | |
| 65–74 | 33.04 | 33.2 | 25.00 | |
| ≥75 | 58.65 | 58.42 | 70.00 | |
| Gender | 0.228 | |||
| Male | 59.13 | 59.01 | 65.00 | |
| Female | 40.87 | 40.99 | 35.00 | |
| Race | 0.063 | |||
| White | 83.09 | 82.96 | 90.00 | |
| Non-White | 16.91 | 17.04 | 10.00 | |
| Comorbiditiesa | ||||
| Obesity | 11.5 | 11.53 | 10.00 | 0.635 |
| Hypertension | 83.38 | 83.65 | 70.00 | 0.000 |
| Diabetes | 30.82 | 30.94 | 25.00 | 0.203 |
| Heart failure | 30.82 | 30.84 | 30.00 | 0.850 |
| Coronary artery disease | 48.21 | 48.28 | 45.00 | 0.516 |
| COPD | 15.46 | 15.47 | 15.00 | 0.898 |
| CKD stage 3 or more | 19.52 | 19.61 | 15.00 | 0.250 |
| Prior CABG | 17.87 | 18.03 | 10.00 | 0.038 |
| Hyperthyroidism | 0.19 | 0.2 | 0.00 | 0.657 |
| Alcohol disorder | 1.06 | 0.99 | 5.00 | 0.000 |
| Mitral valve stenosis | 0.19 | 0.2 | 0.00 | 0.657 |
| Prior stroke/TIA | 27.92 | 28.28 | 10.00 | <0.001 |
| Peripheral vascular disease | 8.21 | 8.18 | 10.00 | 0.511 |
| Anaemia | 15.36 | 15.07 | 30.00 | <0.001 |
| Median household income category for patient's zip codeb | 0.023 | |||
| 1. 0–25th percentile | 17.39 | 17.54 | 10.00 | |
| 2. 26–50th percentile | 23.09 | 22.86 | 35.00 | |
| 3. 51–75th percentile | 27.54 | 27.59 | 25.00 | |
| 4. 76–100th percentile | 30.34 | 30.34 | 30.00 | |
| Primary payerc | 0.314 | |||
| Federal insurance | 92.35 | 92.3 | 95.00 | |
| Private insurance | 7.65 | 7.7 | 5.00 | |
| Hospital characteristics | ||||
| Hospital region | 0.015 | |||
| Northeast | 16.71 | 16.55 | 25.00 | |
| Midwest | 19.9 | 20.1 | 10.00 | |
| South | 34.78 | 34.68 | 40.00 | |
| West | 28.6 | 28.67 | 25.00 | |
| Hospital bed sized | 0.306 | |||
| Small/medium | 30.34 | 30.25 | 35.00 | |
| Large | 69.66 | 69.75 | 65.00 | |
| Hospital teaching statuse | 0.034 | |||
| Non-teaching | 11.79 | 11.92 | 5.00 | |
| Teaching | 88.21 | 88.08 | 95.00 | |
| Hospital location | 0.373 | |||
| Rural | 0.77 | 0.79 | 0.00 | |
| Urban | 99.23 | 99.21 | 100.00 | |
| Admission type | 0.306 | |||
| Non-elective | 11.74 | 11.67 | 15.00 | |
| Elective | 88.26 | 88.33 | 85.00 | |
| Disposition | <0.001 | |||
| Home | 97 | 97.54 | 70.00 | |
| Facility/others | 2.61 | 2.36 | 0.15 | |
| In-hospital mortality | 0.29 | 0 | 0.15 | |
| Length of stay (mean ± std err) (days) | 1.36 ± 0.05 | 1.34 ± 0.04 | 3.00 ± 0.69 | <0.001 |
| Cost of care (mean ± std err) (USD) | 25 724 ± 358 | 25 540 ± 350 | 35 523 ±5164 | 0.001 |
| . | Overall (%), 5175 . | No complication (%) (n = 5075) . | Any complication (%) (n = 100) . | P-value . |
|---|---|---|---|---|
| Watchman device implantations | ||||
| Age (years) | 0.117 | |||
| 18–49 | 0.77 | 0.79 | 0.00 | |
| 50–64 | 7.54 | 7.59 | 5.00 | |
| 65–74 | 33.04 | 33.2 | 25.00 | |
| ≥75 | 58.65 | 58.42 | 70.00 | |
| Gender | 0.228 | |||
| Male | 59.13 | 59.01 | 65.00 | |
| Female | 40.87 | 40.99 | 35.00 | |
| Race | 0.063 | |||
| White | 83.09 | 82.96 | 90.00 | |
| Non-White | 16.91 | 17.04 | 10.00 | |
| Comorbiditiesa | ||||
| Obesity | 11.5 | 11.53 | 10.00 | 0.635 |
| Hypertension | 83.38 | 83.65 | 70.00 | 0.000 |
| Diabetes | 30.82 | 30.94 | 25.00 | 0.203 |
| Heart failure | 30.82 | 30.84 | 30.00 | 0.850 |
| Coronary artery disease | 48.21 | 48.28 | 45.00 | 0.516 |
| COPD | 15.46 | 15.47 | 15.00 | 0.898 |
| CKD stage 3 or more | 19.52 | 19.61 | 15.00 | 0.250 |
| Prior CABG | 17.87 | 18.03 | 10.00 | 0.038 |
| Hyperthyroidism | 0.19 | 0.2 | 0.00 | 0.657 |
| Alcohol disorder | 1.06 | 0.99 | 5.00 | 0.000 |
| Mitral valve stenosis | 0.19 | 0.2 | 0.00 | 0.657 |
| Prior stroke/TIA | 27.92 | 28.28 | 10.00 | <0.001 |
| Peripheral vascular disease | 8.21 | 8.18 | 10.00 | 0.511 |
| Anaemia | 15.36 | 15.07 | 30.00 | <0.001 |
| Median household income category for patient's zip codeb | 0.023 | |||
| 1. 0–25th percentile | 17.39 | 17.54 | 10.00 | |
| 2. 26–50th percentile | 23.09 | 22.86 | 35.00 | |
| 3. 51–75th percentile | 27.54 | 27.59 | 25.00 | |
| 4. 76–100th percentile | 30.34 | 30.34 | 30.00 | |
| Primary payerc | 0.314 | |||
| Federal insurance | 92.35 | 92.3 | 95.00 | |
| Private insurance | 7.65 | 7.7 | 5.00 | |
| Hospital characteristics | ||||
| Hospital region | 0.015 | |||
| Northeast | 16.71 | 16.55 | 25.00 | |
| Midwest | 19.9 | 20.1 | 10.00 | |
| South | 34.78 | 34.68 | 40.00 | |
| West | 28.6 | 28.67 | 25.00 | |
| Hospital bed sized | 0.306 | |||
| Small/medium | 30.34 | 30.25 | 35.00 | |
| Large | 69.66 | 69.75 | 65.00 | |
| Hospital teaching statuse | 0.034 | |||
| Non-teaching | 11.79 | 11.92 | 5.00 | |
| Teaching | 88.21 | 88.08 | 95.00 | |
| Hospital location | 0.373 | |||
| Rural | 0.77 | 0.79 | 0.00 | |
| Urban | 99.23 | 99.21 | 100.00 | |
| Admission type | 0.306 | |||
| Non-elective | 11.74 | 11.67 | 15.00 | |
| Elective | 88.26 | 88.33 | 85.00 | |
| Disposition | <0.001 | |||
| Home | 97 | 97.54 | 70.00 | |
| Facility/others | 2.61 | 2.36 | 0.15 | |
| In-hospital mortality | 0.29 | 0 | 0.15 | |
| Length of stay (mean ± std err) (days) | 1.36 ± 0.05 | 1.34 ± 0.04 | 3.00 ± 0.69 | <0.001 |
| Cost of care (mean ± std err) (USD) | 25 724 ± 358 | 25 540 ± 350 | 35 523 ±5164 | 0.001 |
CABG, coronary artery bypass graft; COPD, chronic obstructive pulmonary disease; CKD, chronic kidney disease; TIA, transient ischaemic attack.
All comorbidities were coded using appropriate ICD-10 codes in secondary diagnosis field as per Supplementary material online, Table S1.
A quartile classification of the estimated median household income of residents in the patients ZIP Code, derived from ZIP Code-demographic data obtained from Claritas. The quartiles are identified by values of 1–4, indicating the poorest to wealthiest populations. Because these estimates are updated annually, the value ranges vary by year https://www.hcup-us.ahrq.gov/db/vars/zipinc_qrtl/nisnote.jsp.
If primary payer were either Medicare or Medicaid, it was defined as federal insurance, all other categories were defined as private insurance https://www.hcup-us.ahrq.gov/db/vars/pay1/nisnote.jsp.
The bed size cut-off points divided into small, medium, and large have been done so that approximately one-third of the hospitals in a given region, location, and teaching status combination would fall within each bed size category https://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp.
A hospital is considered to be a teaching hospital if it has an AMA-approved residency program, is a member of the Council of Teaching Hospitals (COTH) or has a ratio of full-time equivalent interns and residents to beds of 0.25 or higher https://www.hcup-us.ahrq.gov/db/vars/hosp_locteach/nisnote.jsp.
| . | Overall (%), 5175 . | No complication (%) (n = 5075) . | Any complication (%) (n = 100) . | P-value . |
|---|---|---|---|---|
| Watchman device implantations | ||||
| Age (years) | 0.117 | |||
| 18–49 | 0.77 | 0.79 | 0.00 | |
| 50–64 | 7.54 | 7.59 | 5.00 | |
| 65–74 | 33.04 | 33.2 | 25.00 | |
| ≥75 | 58.65 | 58.42 | 70.00 | |
| Gender | 0.228 | |||
| Male | 59.13 | 59.01 | 65.00 | |
| Female | 40.87 | 40.99 | 35.00 | |
| Race | 0.063 | |||
| White | 83.09 | 82.96 | 90.00 | |
| Non-White | 16.91 | 17.04 | 10.00 | |
| Comorbiditiesa | ||||
| Obesity | 11.5 | 11.53 | 10.00 | 0.635 |
| Hypertension | 83.38 | 83.65 | 70.00 | 0.000 |
| Diabetes | 30.82 | 30.94 | 25.00 | 0.203 |
| Heart failure | 30.82 | 30.84 | 30.00 | 0.850 |
| Coronary artery disease | 48.21 | 48.28 | 45.00 | 0.516 |
| COPD | 15.46 | 15.47 | 15.00 | 0.898 |
| CKD stage 3 or more | 19.52 | 19.61 | 15.00 | 0.250 |
| Prior CABG | 17.87 | 18.03 | 10.00 | 0.038 |
| Hyperthyroidism | 0.19 | 0.2 | 0.00 | 0.657 |
| Alcohol disorder | 1.06 | 0.99 | 5.00 | 0.000 |
| Mitral valve stenosis | 0.19 | 0.2 | 0.00 | 0.657 |
| Prior stroke/TIA | 27.92 | 28.28 | 10.00 | <0.001 |
| Peripheral vascular disease | 8.21 | 8.18 | 10.00 | 0.511 |
| Anaemia | 15.36 | 15.07 | 30.00 | <0.001 |
| Median household income category for patient's zip codeb | 0.023 | |||
| 1. 0–25th percentile | 17.39 | 17.54 | 10.00 | |
| 2. 26–50th percentile | 23.09 | 22.86 | 35.00 | |
| 3. 51–75th percentile | 27.54 | 27.59 | 25.00 | |
| 4. 76–100th percentile | 30.34 | 30.34 | 30.00 | |
| Primary payerc | 0.314 | |||
| Federal insurance | 92.35 | 92.3 | 95.00 | |
| Private insurance | 7.65 | 7.7 | 5.00 | |
| Hospital characteristics | ||||
| Hospital region | 0.015 | |||
| Northeast | 16.71 | 16.55 | 25.00 | |
| Midwest | 19.9 | 20.1 | 10.00 | |
| South | 34.78 | 34.68 | 40.00 | |
| West | 28.6 | 28.67 | 25.00 | |
| Hospital bed sized | 0.306 | |||
| Small/medium | 30.34 | 30.25 | 35.00 | |
| Large | 69.66 | 69.75 | 65.00 | |
| Hospital teaching statuse | 0.034 | |||
| Non-teaching | 11.79 | 11.92 | 5.00 | |
| Teaching | 88.21 | 88.08 | 95.00 | |
| Hospital location | 0.373 | |||
| Rural | 0.77 | 0.79 | 0.00 | |
| Urban | 99.23 | 99.21 | 100.00 | |
| Admission type | 0.306 | |||
| Non-elective | 11.74 | 11.67 | 15.00 | |
| Elective | 88.26 | 88.33 | 85.00 | |
| Disposition | <0.001 | |||
| Home | 97 | 97.54 | 70.00 | |
| Facility/others | 2.61 | 2.36 | 0.15 | |
| In-hospital mortality | 0.29 | 0 | 0.15 | |
| Length of stay (mean ± std err) (days) | 1.36 ± 0.05 | 1.34 ± 0.04 | 3.00 ± 0.69 | <0.001 |
| Cost of care (mean ± std err) (USD) | 25 724 ± 358 | 25 540 ± 350 | 35 523 ±5164 | 0.001 |
| . | Overall (%), 5175 . | No complication (%) (n = 5075) . | Any complication (%) (n = 100) . | P-value . |
|---|---|---|---|---|
| Watchman device implantations | ||||
| Age (years) | 0.117 | |||
| 18–49 | 0.77 | 0.79 | 0.00 | |
| 50–64 | 7.54 | 7.59 | 5.00 | |
| 65–74 | 33.04 | 33.2 | 25.00 | |
| ≥75 | 58.65 | 58.42 | 70.00 | |
| Gender | 0.228 | |||
| Male | 59.13 | 59.01 | 65.00 | |
| Female | 40.87 | 40.99 | 35.00 | |
| Race | 0.063 | |||
| White | 83.09 | 82.96 | 90.00 | |
| Non-White | 16.91 | 17.04 | 10.00 | |
| Comorbiditiesa | ||||
| Obesity | 11.5 | 11.53 | 10.00 | 0.635 |
| Hypertension | 83.38 | 83.65 | 70.00 | 0.000 |
| Diabetes | 30.82 | 30.94 | 25.00 | 0.203 |
| Heart failure | 30.82 | 30.84 | 30.00 | 0.850 |
| Coronary artery disease | 48.21 | 48.28 | 45.00 | 0.516 |
| COPD | 15.46 | 15.47 | 15.00 | 0.898 |
| CKD stage 3 or more | 19.52 | 19.61 | 15.00 | 0.250 |
| Prior CABG | 17.87 | 18.03 | 10.00 | 0.038 |
| Hyperthyroidism | 0.19 | 0.2 | 0.00 | 0.657 |
| Alcohol disorder | 1.06 | 0.99 | 5.00 | 0.000 |
| Mitral valve stenosis | 0.19 | 0.2 | 0.00 | 0.657 |
| Prior stroke/TIA | 27.92 | 28.28 | 10.00 | <0.001 |
| Peripheral vascular disease | 8.21 | 8.18 | 10.00 | 0.511 |
| Anaemia | 15.36 | 15.07 | 30.00 | <0.001 |
| Median household income category for patient's zip codeb | 0.023 | |||
| 1. 0–25th percentile | 17.39 | 17.54 | 10.00 | |
| 2. 26–50th percentile | 23.09 | 22.86 | 35.00 | |
| 3. 51–75th percentile | 27.54 | 27.59 | 25.00 | |
| 4. 76–100th percentile | 30.34 | 30.34 | 30.00 | |
| Primary payerc | 0.314 | |||
| Federal insurance | 92.35 | 92.3 | 95.00 | |
| Private insurance | 7.65 | 7.7 | 5.00 | |
| Hospital characteristics | ||||
| Hospital region | 0.015 | |||
| Northeast | 16.71 | 16.55 | 25.00 | |
| Midwest | 19.9 | 20.1 | 10.00 | |
| South | 34.78 | 34.68 | 40.00 | |
| West | 28.6 | 28.67 | 25.00 | |
| Hospital bed sized | 0.306 | |||
| Small/medium | 30.34 | 30.25 | 35.00 | |
| Large | 69.66 | 69.75 | 65.00 | |
| Hospital teaching statuse | 0.034 | |||
| Non-teaching | 11.79 | 11.92 | 5.00 | |
| Teaching | 88.21 | 88.08 | 95.00 | |
| Hospital location | 0.373 | |||
| Rural | 0.77 | 0.79 | 0.00 | |
| Urban | 99.23 | 99.21 | 100.00 | |
| Admission type | 0.306 | |||
| Non-elective | 11.74 | 11.67 | 15.00 | |
| Elective | 88.26 | 88.33 | 85.00 | |
| Disposition | <0.001 | |||
| Home | 97 | 97.54 | 70.00 | |
| Facility/others | 2.61 | 2.36 | 0.15 | |
| In-hospital mortality | 0.29 | 0 | 0.15 | |
| Length of stay (mean ± std err) (days) | 1.36 ± 0.05 | 1.34 ± 0.04 | 3.00 ± 0.69 | <0.001 |
| Cost of care (mean ± std err) (USD) | 25 724 ± 358 | 25 540 ± 350 | 35 523 ±5164 | 0.001 |
CABG, coronary artery bypass graft; COPD, chronic obstructive pulmonary disease; CKD, chronic kidney disease; TIA, transient ischaemic attack.
All comorbidities were coded using appropriate ICD-10 codes in secondary diagnosis field as per Supplementary material online, Table S1.
A quartile classification of the estimated median household income of residents in the patients ZIP Code, derived from ZIP Code-demographic data obtained from Claritas. The quartiles are identified by values of 1–4, indicating the poorest to wealthiest populations. Because these estimates are updated annually, the value ranges vary by year https://www.hcup-us.ahrq.gov/db/vars/zipinc_qrtl/nisnote.jsp.
If primary payer were either Medicare or Medicaid, it was defined as federal insurance, all other categories were defined as private insurance https://www.hcup-us.ahrq.gov/db/vars/pay1/nisnote.jsp.
The bed size cut-off points divided into small, medium, and large have been done so that approximately one-third of the hospitals in a given region, location, and teaching status combination would fall within each bed size category https://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp.
A hospital is considered to be a teaching hospital if it has an AMA-approved residency program, is a member of the Council of Teaching Hospitals (COTH) or has a ratio of full-time equivalent interns and residents to beds of 0.25 or higher https://www.hcup-us.ahrq.gov/db/vars/hosp_locteach/nisnote.jsp.
The CHA2DS2-VASc score of the study population with the corresponding overall complications
| CHA2 DS2-VASca . | Overall complications (%) . | Overall patients in group (n) . |
|---|---|---|
| 0 | 0 | 5 |
| 1 | 15.38 | 65 |
| 2 | 1.16 | 430 |
| 3 | 1.06 | 940 |
| 4 | 3.17 | 1420 |
| 5 | 2.19 | 1140 |
| 6 | 0 | 675 |
| 7 | 1.41 | 355 |
| 8 | 0 | 125 |
| 9 | 0 | 20 |
| P-trend | <0.001 |
| CHA2 DS2-VASca . | Overall complications (%) . | Overall patients in group (n) . |
|---|---|---|
| 0 | 0 | 5 |
| 1 | 15.38 | 65 |
| 2 | 1.16 | 430 |
| 3 | 1.06 | 940 |
| 4 | 3.17 | 1420 |
| 5 | 2.19 | 1140 |
| 6 | 0 | 675 |
| 7 | 1.41 | 355 |
| 8 | 0 | 125 |
| 9 | 0 | 20 |
| P-trend | <0.001 |
CHA2DS2-VASc score was defined as per Supplementary material online, Table S2.
The CHA2DS2-VASc score of the study population with the corresponding overall complications
| CHA2 DS2-VASca . | Overall complications (%) . | Overall patients in group (n) . |
|---|---|---|
| 0 | 0 | 5 |
| 1 | 15.38 | 65 |
| 2 | 1.16 | 430 |
| 3 | 1.06 | 940 |
| 4 | 3.17 | 1420 |
| 5 | 2.19 | 1140 |
| 6 | 0 | 675 |
| 7 | 1.41 | 355 |
| 8 | 0 | 125 |
| 9 | 0 | 20 |
| P-trend | <0.001 |
| CHA2 DS2-VASca . | Overall complications (%) . | Overall patients in group (n) . |
|---|---|---|
| 0 | 0 | 5 |
| 1 | 15.38 | 65 |
| 2 | 1.16 | 430 |
| 3 | 1.06 | 940 |
| 4 | 3.17 | 1420 |
| 5 | 2.19 | 1140 |
| 6 | 0 | 675 |
| 7 | 1.41 | 355 |
| 8 | 0 | 125 |
| 9 | 0 | 20 |
| P-trend | <0.001 |
CHA2DS2-VASc score was defined as per Supplementary material online, Table S2.
Complications
The overall peri-procedural complication rate was 1.9%, and the in-hospital mortality rate was 0.29%. Pericardial effusion requiring pericardiocentesis was noted in 0.68% of cases. Overall, 0.29% of cases required open-heart surgery related to procedural complications. Major bleeding requiring blood product transfusion occurred in 0.1% of the cases. Systemic embolism occurred in 0.29% of the cases, whereas no post-operative stroke was reported (Table 3).
| Watchman’s device closure . | 5175 . |
|---|---|
| Complicationsa | % |
| Overall complications | 1.93 |
| Died | 0.29 |
| Systemic embolism | 0.29 |
| Draining pericardial cavity-open/percutaneous | 0.68 |
| Other pericardial complications | 0.58 |
| Intra-/post-operative stroke | 0 |
| Major bleed needing transfusion | 0.1 |
| Requiring open heart surgery | 0.29 |
| Watchman’s device closure . | 5175 . |
|---|---|
| Complicationsa | % |
| Overall complications | 1.93 |
| Died | 0.29 |
| Systemic embolism | 0.29 |
| Draining pericardial cavity-open/percutaneous | 0.68 |
| Other pericardial complications | 0.58 |
| Intra-/post-operative stroke | 0 |
| Major bleed needing transfusion | 0.1 |
| Requiring open heart surgery | 0.29 |
NIS, National Inpatient Sample.
All complications were coded using appropriate ICD-10 codes in secondary diagnosis field as per Supplementary material online, Table S3
| Watchman’s device closure . | 5175 . |
|---|---|
| Complicationsa | % |
| Overall complications | 1.93 |
| Died | 0.29 |
| Systemic embolism | 0.29 |
| Draining pericardial cavity-open/percutaneous | 0.68 |
| Other pericardial complications | 0.58 |
| Intra-/post-operative stroke | 0 |
| Major bleed needing transfusion | 0.1 |
| Requiring open heart surgery | 0.29 |
| Watchman’s device closure . | 5175 . |
|---|---|
| Complicationsa | % |
| Overall complications | 1.93 |
| Died | 0.29 |
| Systemic embolism | 0.29 |
| Draining pericardial cavity-open/percutaneous | 0.68 |
| Other pericardial complications | 0.58 |
| Intra-/post-operative stroke | 0 |
| Major bleed needing transfusion | 0.1 |
| Requiring open heart surgery | 0.29 |
NIS, National Inpatient Sample.
All complications were coded using appropriate ICD-10 codes in secondary diagnosis field as per Supplementary material online, Table S3
There was no difference in complication rates based on the region of the country, urban vs. rural location of the hospital, elective vs. non-elective admission, or bed size (small/medium vs. large). Non-teaching hospitals had a higher complication rate compared with teaching hospitals (P = 0.03) (Table 1).
Comparison with previous studies
We also compared the complications associated with the Watchman device from the PREVAIL, PROTECT-AF trial, CAP, and the EWOLUTION cohort. We noted that the complication rates were similar to those noted from the EWOLUTION cohort and less than those in the RCTs (Table 4).
| . | PROTECT-AF . | CAP . | PREVAIL . | EWOLUTION cohort . | NIS . |
|---|---|---|---|---|---|
| Total implants (n) | 408 | 460 | 265 | 1025 | 5175 |
| Overall complications (%) | 8.7 | 4.1 | 2.2 | 1.8 | 1.9 |
| Pericardial effusion requiring surgery (%) | 1.6 | 0.2 | 0.4 | 0.09 | 0.29 |
| Pericardial effusion with pericardiocentesis (%) | 2.4 | 1.2 | 1.5 | 0.29 | 0.68 |
| Procedure-related ischaemic strokes (%) | 1.1 | 0 | 0.7 | 0 | 0 |
| Mortality (%) | 0 | 0 | 0 | 0.39 | 0.29 |
| . | PROTECT-AF . | CAP . | PREVAIL . | EWOLUTION cohort . | NIS . |
|---|---|---|---|---|---|
| Total implants (n) | 408 | 460 | 265 | 1025 | 5175 |
| Overall complications (%) | 8.7 | 4.1 | 2.2 | 1.8 | 1.9 |
| Pericardial effusion requiring surgery (%) | 1.6 | 0.2 | 0.4 | 0.09 | 0.29 |
| Pericardial effusion with pericardiocentesis (%) | 2.4 | 1.2 | 1.5 | 0.29 | 0.68 |
| Procedure-related ischaemic strokes (%) | 1.1 | 0 | 0.7 | 0 | 0 |
| Mortality (%) | 0 | 0 | 0 | 0.39 | 0.29 |
NIS, National Inpatient Sample; RCTs, randomized clinical trials.
| . | PROTECT-AF . | CAP . | PREVAIL . | EWOLUTION cohort . | NIS . |
|---|---|---|---|---|---|
| Total implants (n) | 408 | 460 | 265 | 1025 | 5175 |
| Overall complications (%) | 8.7 | 4.1 | 2.2 | 1.8 | 1.9 |
| Pericardial effusion requiring surgery (%) | 1.6 | 0.2 | 0.4 | 0.09 | 0.29 |
| Pericardial effusion with pericardiocentesis (%) | 2.4 | 1.2 | 1.5 | 0.29 | 0.68 |
| Procedure-related ischaemic strokes (%) | 1.1 | 0 | 0.7 | 0 | 0 |
| Mortality (%) | 0 | 0 | 0 | 0.39 | 0.29 |
| . | PROTECT-AF . | CAP . | PREVAIL . | EWOLUTION cohort . | NIS . |
|---|---|---|---|---|---|
| Total implants (n) | 408 | 460 | 265 | 1025 | 5175 |
| Overall complications (%) | 8.7 | 4.1 | 2.2 | 1.8 | 1.9 |
| Pericardial effusion requiring surgery (%) | 1.6 | 0.2 | 0.4 | 0.09 | 0.29 |
| Pericardial effusion with pericardiocentesis (%) | 2.4 | 1.2 | 1.5 | 0.29 | 0.68 |
| Procedure-related ischaemic strokes (%) | 1.1 | 0 | 0.7 | 0 | 0 |
| Mortality (%) | 0 | 0 | 0 | 0.39 | 0.29 |
NIS, National Inpatient Sample; RCTs, randomized clinical trials.
Discussion
Using a large, nationally representative database of inpatient hospitalization, we demonstrate the safety of Watchman implantation in the routine practice in the USA. The complications observed in routine practice are less frequent than those reported in the pivotal RCTs and may represent greater user experience over time.13
The findings of our study are in concordance with findings reported by the recently published EWOLUTION registry regarding the safety profile of the Watchman device.7
The Watchman device has been studied in two RCTs, namely the PROTECT-AF and PREVAIL.6,14PROTECT-AF trial demonstrated a non-inferior rate of cardiovascular death, stroke, or systemic embolism, compared with warfarin alone. Adverse outcomes were higher in the device group due to a high occurrence of pericardial effusion. The PREVAIL trial was performed to address concerns raised by the FDA on the patient selection and safety data from the PROTECT-AF trial. The PREVAIL trial reported a lower overall complication rate compared with the PROTECT-AF trial. The CAP registry investigated patient outcomes after the end of the enrolment of PROTECT-AF trial and also reported a lower complication rate.15 A patient-level meta-analysis that combined 5-year outcomes of both PROTECT-AF and PREVAIL trials reported equivalent all-cause stroke with significant reductions in haemorrhagic and fatal/disabling stroke. The study also reported significant reductions in cardiovascular and all-cause mortality.16 The multi-centre EWOLUTION registry reported outcomes of LAAO with the Watchman device in 1025 patients treated in 47 centres in 13 countries where indication was based on the European Society of Cardiology guidelines.17
The EWOLUTION cohort evaluated the clinical outcomes in routine clinical practice outside of RCTs.18 The NIS has been used to assess the adverse outcomes of LAAO in the USA between 2006 and 2010.19 The study reported a significantly higher overall adverse event rate (24.3%) compared with all other studies. It could be partially explained by the inclusion of a broader range of complications. Of note, the study could not assess the rate of complications associated with the Watchman device, specifically due to the use of a single ICD-9 code for LAAO. Thus, it could not differentiate between various devices, specifically those with the combined epicardial and endocardial approach.
Our finding of overall complications being 1.9% is consistent with results from the EWOLUTION cohort (1.8%). Inherent limitations to observational studies, transition to ICD-10 codes, underreporting or missed complications after discharge have to be considered when comparing our study with the previous RCTs.
The initial experience of Watchman from the PROTECT-AF trial had a complication rate of 8.7%. This high complication rate was attributed to operator inexperience. Subsequent reports from the PREVAIL trial and the CAP registry have suggested a decreasing incidence of complications (Table 4). The fact that our data also mirror the findings from the EWOLUTION cohort is consistent with improved outcomes with more experience and training in using the technology and is consistent with our relatively recent study period.
In our study, we noted that the most frequent complication was pericardial effusion requiring pericardiocentesis akin to that reported in PROTECT-AF, PREVAIL, CAP, and EWOLUTION. We report that pericardial effusion requiring pericardiocentesis was 0.68%. The pericardial effusion rate was higher in PROTECT-AF (2.4%). We report the overall need for open-heart surgery to be 0.29%, which was lower than the PROTECT-AF, PREVAIL, and CAP but higher than the EWOLUTION cohort (Table 4).
In concordance with the EWOLUTION and CAP, there were no procedure-related ischaemic strokes in our analysis,15,17 whereas the rate of procedure-related ischaemic stroke in PROTECT-AF and PREVAIL was 1.1% and 0.7%, respectively.5,6
In our study, the procedure-related mortality is 0.29%; it compares with a total of 0.39% in the EWOUTION registry. The mortality rate was 0% in the previously published RCTs (Table 4). Most of the deaths in the previous RCTs occurred during the follow-up, so they were most likely unrelated to the procedure.19
This report provides a much larger body of data on the peri-procedural adverse events of Watchman implantations. The result of our study, with corresponding overall complications rate of 1.93% are encouraging in that it is reflective of the maturation of the technology and implant technique. The newest generation of the device (Watchman FLX) has been available in Europe since March 2019. The new device is available in five different sizes. Therefore, it can be used for different LAA ostia sizes. The new Watchman FLX device can be implanted in shallower LAA anatomies due to the reduced device length. A single-centre experience with Watchman FLX reported no peri-procedural strokes, pericardial effusion, or device embolization. However, there are no large studies to confirm the safety of the new device.20
Accurate observational data are especially important in the field of LAAO because several approaches are in use notwithstanding those with substantially less evidence than that supporting the WATCHMAN system.21 Consequently, robust surveillance for safety issues could have important implications for patients. Because of the restricted populations and operators involved in traditional randomized trials, other sources of data help to evaluate the generalizability of findings into the real-world clinical setting. Observational data are crucial supplements to RCTs because they provide a broader perspective from a much larger cohort size. Observational studies have evolved to serve as an important component of post-market device surveillance in practice.22 The approval of the WATCHMAN in the USA by the FDA was based on the conduct of two post-market cohort studies,23 reflecting the expanding importance of observational studies in the FDA surveillance strategy.
Limitations
We acknowledge several limitations, some of which are inherent to the analysis of any claims data. We used the best practices as outlined by prior reports highlighting the use of claims datasets.24,25 Coding errors, unmeasured confounders, and under-reporting of comorbidities are potential limitations of using ICD-10 CM codes. The actual procedural experience, challenge during implantation, and overall results of the device deployment cannot be assessed. Further complications noted after discharge from the hospital cannot be accounted for.
Conclusions
Our study demonstrates a favourable safety profile for Watchman device implantation in real-world clinical practice. Our findings are in concordance with the EWOLUTION cohort and compare favourably with the previously published RCTs. Future observational studies are essential to assess the safety profile as regional differences may emerge.
Supplementary material
Supplementary material is available at Europace online.
Conflict of interest: The authors declare that there is no conflict of interest.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
HHS (ed). WATCHMANTM Left Atrial Appendage Closure Device. FDA, Natick, MA,
HCUP Databases. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality R, MD. Overview of the National (Nationwide) Inpatient Sample (NIS),
HCUP Databases. Healthcare Cost and Utilization Project - Overview of the National (Nationwide) Inpatient Sample (NIS) Agency for Healthcare Research and Quality; Rockville, MD: Dec, 2019. www.hcup-us.ahrq.gov/nisoverview.jsp (28 August 2019, date last accessed).
Elixhauser Comorbidity Software for ICD-10-CM (beta version) Healthcare Cost and Utilization Project (HCUP).Agency for Healthcare Research and Quality R, Rockville, MD,
Center for Devices and Radiological Health USFaDA. Strengthening Our National System for Medical Device Postmarket Surveillance, Food and Drug Administration 10903 New Hampshire Avenue Document Control Center – WO66-G609 Silver Spring, MD 20993-0002,
Approval. UDoHaHSWLo. WATCHMAN Letter of Approval. http://www.accessdata.fda.gov/cdrh_docs/pdf13/p130013a.pdf (26 December
Author notes
Fouad Khalil and Shilpkumar Arora contributed equally to the study.
- atrial fibrillation
- pericardial effusion
- pericardiocentesis
- atrial flutter
- left auricular appendage
- hemorrhage
- cerebrovascular accident
- ischemic stroke
- blood transfusion
- hospital mortality
- inpatients
- safety
- united states food and drug administration
- diagnosis
- mortality
- transfusion
- embolism
- international classification of diseases
- percutaneous left atrial appendage transcatheter occlusion
- device implant
- percutaneous left atrial appendage occlusion device
- left atrial appendage occlusion



