-
PDF
- Split View
-
Views
-
Cite
Cite
H Morgan, M Strocchi, A Ardinal, M Bishop, A Chiribiri, C A Rinaldi, D Perera, Non-invasive electrocardiographic assessment of arrhythmic risk in ischaemic cardiomyopathy patients undergoing revasularisation, EP Europace, Volume 26, Issue Supplement_1, May 2024, euae102.298, https://doi.org/10.1093/europace/euae102.298
Close - Share Icon Share
Abstract
Ventricular arrhythmias are a leading cause of death in patients with ischaemic cardiomyopathy (ICM). Ischaemia is thought to increase arrhythmic risk and coronary revascularisation is frequently undertaken to reduce this risk, although the recent REVIVED-BCIS2 trial did not show a difference in the incidence of death, device therapies or sustained arrhythmias in patients assigned to have percutaneous coronary intervention (PCI) compared to optimal medical therapy alone(1).
We assessed the mechanistic effects of revascularisation on arrhythmic risk in patients with ICM using non-invasive electrocardiographic imaging (ECGi).
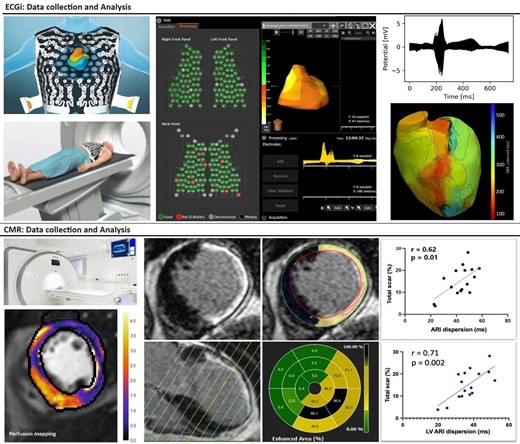
Patients were eligible if they had a left ventricular ejection fraction (LVEF) <40%, extensive coronary disease (BCIS Jeopardy Score≥6) and were scheduled to undergo revascularisation with coronary artery bypass grafting or PCI. ECGi assessment was performed using a 252-electrode vest with anatomical co-registration using a CT thorax. Patients underwent stress perfusion cardiac magnetic resonance (CMR) imaging; both ECGi and CMR were conducted at baseline and 3 months post revascularisation(Figure 1). The primary outcome measure was dispersion of repolarisation measured using global activation recovery interval (ARI) dispersion. Secondary outcome measures included repolarisation time (RT) dispersion, mean ARI and LV ARI dispersion. We also assessed the relationship between ARI dispersion, revascularisation and left ventricular scar burden. Data are presented as mean ± SD or median [IQR].
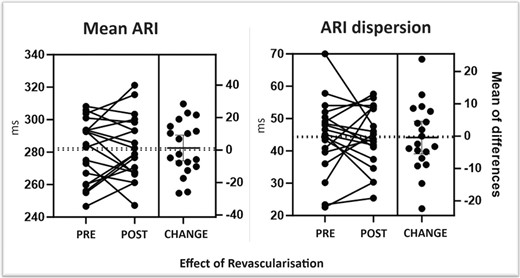
Thirty patients were recruited between 2020-2023; age 67±11 years, 90% male, BMI 28±5 and baseline LVEF was 29±8%. Twelve patients underwent CABG, 18 (60%) had PCI. The BCIS jeopardy score was 10 [9-11] at enrolment and decreased to 2 [0-4] after revascularisation. The LV scar burden at baseline was 15.1±6.5% and the change at 3 months was -0.5±5% (p=0.70). ARI dispersion and LV ARI dispersion were correlated with LV scar burden (r=0.62,p=0.01 and 0.71,p=0.002 respectively). No differences were seen in ARI dispersion (44.5 vs 44.1, p=0.86) or secondary outcome measures before and after revascularisation (RT dispersion: 45.5 vs 44.7, p=0.49; Mean ARI: 281.3 vs 282.6, p=0.74; ARI dispersion: 44.5 vs 44.1, p=0.86; LV ARI dispersion: 38.4 vs 36.7, p=0.39)(Figure 2). The LVEF change on CMR at 3 months was +6.9±10%; no relationship was seen between change in LVEF and ARI dispersion.
Author notes
Funding Acknowledgements: Type of funding sources: Other. Main funding source(s): British Heart Foundation Clinical Research Training Fellowship
- cardiac arrhythmia
- electrocardiogram
- percutaneous coronary intervention
- ischemia
- left ventricular ejection fraction
- coronary artery bypass surgery
- body mass index procedure
- coronary revascularization
- ischemic cardiomyopathy
- left ventricle
- cause of death
- cicatrix
- perfusion
- risk assessment
- diagnostic imaging
- stress
- chest
- ventricular arrhythmia
- coronary heart disease
- revascularization
- cardiac mri
- medical devices
- outcome measures
- electrocardiogram with concurrent imaging
- medical management
- primary outcome measure



