-
PDF
- Split View
-
Views
-
Cite
Cite
Raquel Adeliño, Katarzyna Malaczynska-Rajpold, Laura Perrotta, Martin Manninger, Philippe Vanduynhoven, Martina Nesti, Emilia-Violeta Goanță, Victor Waldmann, Nikola Pavlovic, Michal M Farkowski, Jose M Guerra, Diego Penela, Serge Boveda, Julian K R Chun, Occupational radiation exposure of electrophysiology staff with reproductive potential and during pregnancy: an EHRA survey, EP Europace, Volume 25, Issue 9, September 2023, euad216, https://doi.org/10.1093/europace/euad216
Close - Share Icon Share
Abstract
Electrophysiology (EP) is a growing field in cardiology, with an increasing involvement of young people. Nevertheless, concerns about radiation exposure and its impact on reproduction and pregnancy may discourage the choice of an EP career. The study is aimed at investigating the level of awareness and main sources of concern about the effects of radiation on reproductive potential and pregnancy, exploring the safety measures adopted in different EP labs, and verifying the adherence to the current guidelines.
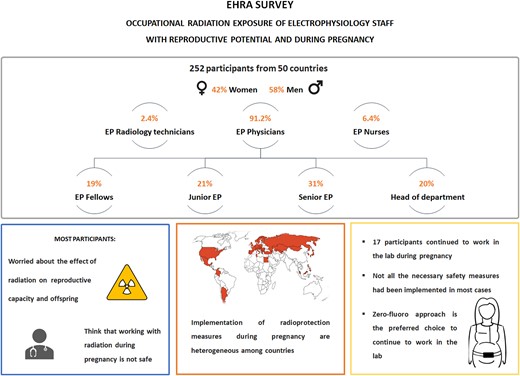
An online survey was conducted using the European Heart Rhythm Association (EHRA) infrastructure from April to June 2022. A total of 252 EP personnel (42% women) participated, from 50 countries and different professional roles. Most participants expressed concerns regarding the effects of radiation on reproductive capacity (67.1%) and offspring diseases (68.2%). Only 37.9% of participants were aware of the EHRA 2017 consensus document about occupational radiation exposure. Most participants (80.9%) considered that occupational radiation during pregnancy is not safe. EP female staff were not allowed to work in the EP lab during pregnancy in 48.1% of cases. Zero-fluoroscopy was the preferred choice to continue working in the EP lab during pregnancy.
EP staff, including both men and women, have concerns about the effects of radiation on reproductive capacity. Despite the recommendations issued by international bodies, implementation of the policies regarding pregnancy and occupational radiation exposure is heterogeneous. Zero-fluoroscopy is the preferred approach to ensure safety during pregnancy in the EP lab.
This EHRA survey explores for the first time the awareness and concerns regarding occupational radiation exposure on reproductive capacity and pregnancy across EP laboratory staff members.
The majority of respondents is unaware of the EHRA 2017 consensus document on occupational radiation exposure which endorses work during pregnancy within specific regulations.
Still, a high percentage (45%) of pregnant EP women are not permitted to work in the EP laboratory.
Implementation of radioprotection measures during pregnancy is heterogeneous and requires improvement.
Zero or nearly zero fluoroscopy appears to be the preferred strategy during pregnancy, but its use is not yet generalized.
Introduction
Electrophysiology (EP) is a greatly expanding field in cardiology, with an increasing involvement of young people in different roles (physicians, nurses, radiology technicians, etc).1
Many EP procedures are performed under fluoroscopy guidance. However, technological advances such as 3D navigation systems have enabled to reduce the use of radiation, even allowing for a zero or nearly zero–fluoroscopy approach.2,3 In addition, protective cabins or bigger/thicker protective lead shields are also expanding their use.4 Nevertheless, the implementation of these measures is very heterogeneous among different centres, and EP staff with reproductive capacity are still potentially exposed to variable levels of occupational radiation.
Occupational radiation may be a discouraging reason for choosing EP as professional career among cardiologists, especially for women, due to its potential effects on pregnancy.5
In 2013, guidelines on radiological protection in cardiology were issued by the International Commission on Radiological Protection (ICRP)6 and were adopted by the European Directive 2013/59/Euratom.7 It was stated that the condition of pregnancy does not require removing the exposed professional from work but careful review of working conditions to guarantee the limit of safe foetal radiation exposure of 1 mSv throughout pregnancy.6,7 Based on this, the EHRA consensus document on occupational radiation exposure in the electrophysiology laboratory with a focus on personnel with reproductive potential and during pregnancy was published in 2017, to inform about international recommendations and legislations on occupational exposure in the EP laboratory to personnel with childbearing potential and during pregnancy.8 The European Association of Percutaneous Cardiovascular Interventions (EAPCI), in collaboration with EHRA, has also recently published a position statement on this issue.9
This survey was an initiative from the EHRA Young EP committee and executed in conjunction with the EHRA SIC aiming to explore the general knowledge of the potentially harmful effects of radiation on EP staff with reproductive potential and during pregnancy, to identify the main sources of concern, to investigate the different safety measures adopted in different EP labs, and to verify the adherence to the ICRP guidelines, the Euratom directive, and the EHRA 2017 consensus document.
Methods
An online questionnaire consisting of 48 questions (see Supplementary material) was distributed using the European Heart Rhythm Association (EHRA) infrastructure to EHRA members and members of national EP working groups and via social media platforms (Twitter, LinkedIn, and Facebook) between April and June 2022. Although the survey was distributed through a European network, there was no restriction to participate for non-European countries. The survey addressed all staff working in the EP lab, including all professional roles.
Continuous variables are presented as mean ± SD or median ± interquartile range (IQR). Categorical variables are presented as percentages and counts. Comparison between groups was performed using chi-squared test for categorical questions and Mann–Whitney U test for questions with continuous numerical answers. A two-sided P-value of <0.05 was considered significant. Statistical analyses and graphics were performed using Stata software (version 15.1, StataCorp, College Station, TX).
Results
Demographic data
The survey was completed by 252 EP staff participants [42% (105) women, 58% (147) men] from 50 different countries (34 European and 16 extra-European, Figure 1 ). Among them, 2.4% (6) were radiology technicians, 6.4% (16) nurses, 19.1% (48) EP fellows, 21.0% (53) junior consultants, 31.4% (79) senior consultants, and 19.5% (49) heads of department. Distribution by gender of professional role showed a statistically significantly higher proportion of female nurses and male head of department, whereas the other professional categories showed a similar distribution. Most participants were in the age group between 30–39 y.o. (47.6%) (Table 1). Among the youngest age group (below 30 y.o.), there was a greater proportion of females (11.4% vs. 2.7%, P = 0.023) while there was a tendency of a higher proportion of men (12.9% vs. 5.7%, P = 0.059) in the 50–59 y.o. group, and a similar distribution in other age intervals. The general average years of experience in EP was 8 ± 9 years, with a longer experience in men than women (10 ± 12 years vs. 6 ± 8 years, P = 0.001). Demographic data are summarized in Table 1.
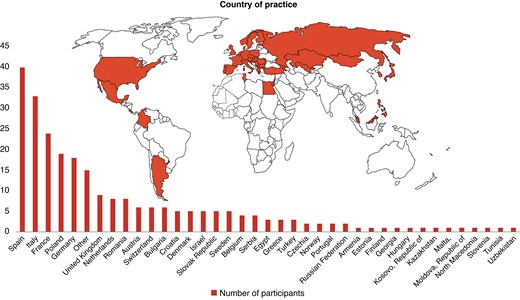
Bar graphic representing the number of participants per country.
| . | Total . | Male . | Female . | P-value . |
|---|---|---|---|---|
| Age (years) | (n = 252) | (n = 147) | (n = 105) | |
| Below 30 | 16 (6.4%) | 4 (2.7%) | 12 (11.4%) | 0.005 |
| 30–39 | 120 (47.6%) | 63 (42.9%) | 57 (54.3%) | 0.073 |
| 40–49 | 78 (31.0%) | 50 (20.6%) | 28 (26.7%) | 0.214 |
| 50–59 | 25 (9.9%) | 19 (12.9%) | 6 (5.7%) | 0.059 |
| 60–69 | 10 (4.0%) | 8 (3.2%) | 2 (1.9%) | 0.156 |
| 70 or older | 3 (1.2%) | 3 (2.0%) | 0 (0.0%) | 0.141 |
| Professional role | (n = 251) | (n = 146) | (n = 105) | |
| Radiology technician | 6 (2.4%) | 4 (2.7%) | 2 (1.9%) | 0.675 |
| Nurse | 16 (6.4%) | 5 (3.4%) | 11 (11.4%) | 0.023 |
| Fellow | 48 (19.1%) | 23 (15.6%) | 25 (23.8%) | 0.104 |
| Junior consultant | 53 (21.0%) | 28 (19.1%) | 25 (23.8%) | 0.360 |
| Senior consultant | 79 (31.4%) | 45 (30.6%) | 34 (32.4%) | 0.765 |
| Head of department | 49 (19.5%) | 41 (27.9%) | 8 (7.6%) | <0.01 |
| Years of experience in EP | 8 ± 9 | 10 ± 12 | 6 ± 8 | 0.001 |
| . | Total . | Male . | Female . | P-value . |
|---|---|---|---|---|
| Age (years) | (n = 252) | (n = 147) | (n = 105) | |
| Below 30 | 16 (6.4%) | 4 (2.7%) | 12 (11.4%) | 0.005 |
| 30–39 | 120 (47.6%) | 63 (42.9%) | 57 (54.3%) | 0.073 |
| 40–49 | 78 (31.0%) | 50 (20.6%) | 28 (26.7%) | 0.214 |
| 50–59 | 25 (9.9%) | 19 (12.9%) | 6 (5.7%) | 0.059 |
| 60–69 | 10 (4.0%) | 8 (3.2%) | 2 (1.9%) | 0.156 |
| 70 or older | 3 (1.2%) | 3 (2.0%) | 0 (0.0%) | 0.141 |
| Professional role | (n = 251) | (n = 146) | (n = 105) | |
| Radiology technician | 6 (2.4%) | 4 (2.7%) | 2 (1.9%) | 0.675 |
| Nurse | 16 (6.4%) | 5 (3.4%) | 11 (11.4%) | 0.023 |
| Fellow | 48 (19.1%) | 23 (15.6%) | 25 (23.8%) | 0.104 |
| Junior consultant | 53 (21.0%) | 28 (19.1%) | 25 (23.8%) | 0.360 |
| Senior consultant | 79 (31.4%) | 45 (30.6%) | 34 (32.4%) | 0.765 |
| Head of department | 49 (19.5%) | 41 (27.9%) | 8 (7.6%) | <0.01 |
| Years of experience in EP | 8 ± 9 | 10 ± 12 | 6 ± 8 | 0.001 |
| . | Total . | Male . | Female . | P-value . |
|---|---|---|---|---|
| Age (years) | (n = 252) | (n = 147) | (n = 105) | |
| Below 30 | 16 (6.4%) | 4 (2.7%) | 12 (11.4%) | 0.005 |
| 30–39 | 120 (47.6%) | 63 (42.9%) | 57 (54.3%) | 0.073 |
| 40–49 | 78 (31.0%) | 50 (20.6%) | 28 (26.7%) | 0.214 |
| 50–59 | 25 (9.9%) | 19 (12.9%) | 6 (5.7%) | 0.059 |
| 60–69 | 10 (4.0%) | 8 (3.2%) | 2 (1.9%) | 0.156 |
| 70 or older | 3 (1.2%) | 3 (2.0%) | 0 (0.0%) | 0.141 |
| Professional role | (n = 251) | (n = 146) | (n = 105) | |
| Radiology technician | 6 (2.4%) | 4 (2.7%) | 2 (1.9%) | 0.675 |
| Nurse | 16 (6.4%) | 5 (3.4%) | 11 (11.4%) | 0.023 |
| Fellow | 48 (19.1%) | 23 (15.6%) | 25 (23.8%) | 0.104 |
| Junior consultant | 53 (21.0%) | 28 (19.1%) | 25 (23.8%) | 0.360 |
| Senior consultant | 79 (31.4%) | 45 (30.6%) | 34 (32.4%) | 0.765 |
| Head of department | 49 (19.5%) | 41 (27.9%) | 8 (7.6%) | <0.01 |
| Years of experience in EP | 8 ± 9 | 10 ± 12 | 6 ± 8 | 0.001 |
| . | Total . | Male . | Female . | P-value . |
|---|---|---|---|---|
| Age (years) | (n = 252) | (n = 147) | (n = 105) | |
| Below 30 | 16 (6.4%) | 4 (2.7%) | 12 (11.4%) | 0.005 |
| 30–39 | 120 (47.6%) | 63 (42.9%) | 57 (54.3%) | 0.073 |
| 40–49 | 78 (31.0%) | 50 (20.6%) | 28 (26.7%) | 0.214 |
| 50–59 | 25 (9.9%) | 19 (12.9%) | 6 (5.7%) | 0.059 |
| 60–69 | 10 (4.0%) | 8 (3.2%) | 2 (1.9%) | 0.156 |
| 70 or older | 3 (1.2%) | 3 (2.0%) | 0 (0.0%) | 0.141 |
| Professional role | (n = 251) | (n = 146) | (n = 105) | |
| Radiology technician | 6 (2.4%) | 4 (2.7%) | 2 (1.9%) | 0.675 |
| Nurse | 16 (6.4%) | 5 (3.4%) | 11 (11.4%) | 0.023 |
| Fellow | 48 (19.1%) | 23 (15.6%) | 25 (23.8%) | 0.104 |
| Junior consultant | 53 (21.0%) | 28 (19.1%) | 25 (23.8%) | 0.360 |
| Senior consultant | 79 (31.4%) | 45 (30.6%) | 34 (32.4%) | 0.765 |
| Head of department | 49 (19.5%) | 41 (27.9%) | 8 (7.6%) | <0.01 |
| Years of experience in EP | 8 ± 9 | 10 ± 12 | 6 ± 8 | 0.001 |
Radiologic protection training
Out of the 252 respondents, 77% (193) stated that specific training in radiologic protection is mandatory, while 23% (58) answered that this was not mandatory. Only 10% (25) of the respondents had not performed this type of training.
Degree of concern about occupational exposure to radiation
Most respondents [67% (169)] claimed to be worried about the effects of occupational radiation exposure on reproductive capacity and on offspring (Figure 2A and B), without statistically significant differences by gender. However, when analysing by age, the group between 30 and 39 y.o. showed the greatest concern compared to the other age groups (P = 0.001).
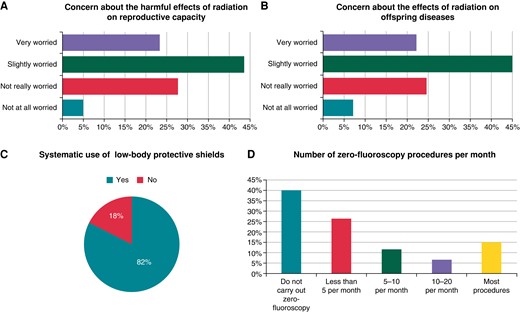
Graphic representation of the answers to four general questions in the survey. Panels A and B represent the results to the question about the degree of concern about the effects of occupational radiation on the reproductive capacity and offspring, respectively. Panel C shows the results to a question that asked about the use of low-body radiation protector. Panel D represents the results of the question about the number of zero-fluoroscopy procedures per month.
Measures to reduce radiation exposure
Most respondents [82.5% (207)] use systematically lower-body protective shields (Figure 2C). A high proportion of respondents [40% (100)] does not perform zero-fluoroscopy procedures, while 15.2% (38) attempted most procedures without the use of fluoroscopy (Figure 2D).
Occupational radiation exposure and pregnancy
The majority of the respondents stated that they were aware of the legal regulations in their countries and the local policies in their centres concerning occupational radiation exposure [55.2% (139) and 58.2% (146), respectively]. A lower proportion of participants [37.9% (95)] claimed to know the EHRA 2017 consensus document by Sarkozy et al8 (Table 2).
Results from the three questions about awareness of the national legal regulation and the hospital policy with regard to pregnancy and occupational radiation exposure, and of the EHRA 2017 consensus document about occupational radiation exposure in the electrophysiology laboratory with a focus on personnel with reproductive potential and during pregnancy
| Awareness of… . | National legal regulation . | Centre local policy . | EHRA 2017 consensus document . |
|---|---|---|---|
| (n = 252) . | (n = 251) . | (n = 251) . | |
| Yes | 139 (55.2%) | 146 (58.2%) | 95 (37.85%) |
| No | 52 (20.6%) | 55 (21.9%) | 122 (48.6%) |
| Not sure | 61 (24.2%) | 50 (19.9%) | 34 (13.6%) |
| Awareness of… . | National legal regulation . | Centre local policy . | EHRA 2017 consensus document . |
|---|---|---|---|
| (n = 252) . | (n = 251) . | (n = 251) . | |
| Yes | 139 (55.2%) | 146 (58.2%) | 95 (37.85%) |
| No | 52 (20.6%) | 55 (21.9%) | 122 (48.6%) |
| Not sure | 61 (24.2%) | 50 (19.9%) | 34 (13.6%) |
Results from the three questions about awareness of the national legal regulation and the hospital policy with regard to pregnancy and occupational radiation exposure, and of the EHRA 2017 consensus document about occupational radiation exposure in the electrophysiology laboratory with a focus on personnel with reproductive potential and during pregnancy
| Awareness of… . | National legal regulation . | Centre local policy . | EHRA 2017 consensus document . |
|---|---|---|---|
| (n = 252) . | (n = 251) . | (n = 251) . | |
| Yes | 139 (55.2%) | 146 (58.2%) | 95 (37.85%) |
| No | 52 (20.6%) | 55 (21.9%) | 122 (48.6%) |
| Not sure | 61 (24.2%) | 50 (19.9%) | 34 (13.6%) |
| Awareness of… . | National legal regulation . | Centre local policy . | EHRA 2017 consensus document . |
|---|---|---|---|
| (n = 252) . | (n = 251) . | (n = 251) . | |
| Yes | 139 (55.2%) | 146 (58.2%) | 95 (37.85%) |
| No | 52 (20.6%) | 55 (21.9%) | 122 (48.6%) |
| Not sure | 61 (24.2%) | 50 (19.9%) | 34 (13.6%) |
96.8% (244) of participants believed that both female and male personnel should be equally informed about occupational radiation exposure and pregnancy.
33.5% (84) of the participants stated that they were allowed to continue to work with radiation during pregnancy in their countries, while 39.8% (100) and 26.7% (67) declared they were not allowed or they were not sure, respectively. Of note, participants from 12 countries (Austria, Belgium, Bulgaria, France, Germany, Israel, Netherlands, Poland, Portugal, Romania, Spain, and Sweden) answered both ‘yes’ and ‘no’ to this question.
Once an EP female staff member declares pregnancy, in 45.0% of cases, she is not allowed to continue to work in the lab and is redeployed to different professional tasks. Only in 17.1% of cases they continue to work with the use of radiation (with appropriate safety measures). In 14.4%, only zero-fluoroscopy procedures are allowed, and in 20.3%, the work is restricted to the control room.
However, the majority of the participants [80.9% (203)] thinks that working with ionizing radiation during pregnancy is not safe, with a higher proportion of men (85.7% vs. 74.03%, P = 0.021). Regarding the attitude of the other team members towards a pregnant colleague, 56.2% (140) considered it supportive, while 20.9% (52) considered it uncomfortable.
Most participants [74.1% (186)], especially women (96.2% vs. 58.5%, P < 0.001), believed that pregnancy and maternity leave represent a disadvantage in the professional career for EP women.
Questions addressed specifically to men
Among the participants, only 24.5% (36) knew about the radiation threshold dose beyond which semen quality is affected. During the training period, 53.74% (79) were informed by the occupational health department about the protection measures to be taken to minimize the effects of radiation on germ cells. In the case of three participants (2.0%), diagnostic sperm tests were performed by the occupational health department; 53.1% (78) stated that diagnostic sperm tests should be performed as part of occupational health examination and 44.9% (66) did not consider it necessary.
Questions addressed specifically to women
Women who have been pregnant during their professional career
Among the 105 female participants, 41.0% (43) had a pregnancy during her professional career. Out of them, 80.5% (33) were worried about notifying their managers about pregnancy, mainly due to concern about being redeployed or not being able to keep up with work [39.0% (16)]. Other sources of concern were fear of being fired or being negatively considered by their colleagues in terms of their commitment to work. Forty-one percent [41.5% (17)] stated that they did not receive the information about the radiation-related safety measures from their occupational health department once they announced their pregnancy. Only 21.9% (23) among the EP female staff were correctly informed by the occupational health department about the safety measures during pregnancy.
Out of the 43 women who had been pregnant during their professional career, 58.5% (24) stopped working in the EP lab (Figure 3A), in most cases [45.8% (11)] due to restrictions from the occupational health department/local regulations, and for a self-decision in 29.2% (7), mainly for safety reasons concerning foetal risk [71.4% (15)] (Figure 3B).
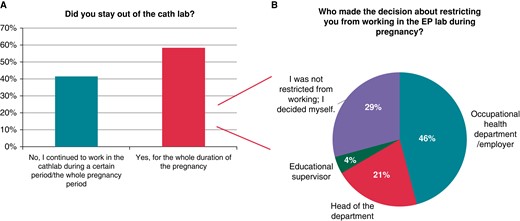
Results from questions addressed to women who had been pregnant during their professional career. Graphic A shows the answers to the ‘Did you stay out of the EP lab?’ addressed to women who had been pregnant during their professional career. Graphic B shows the answers to the question ‘who restricted you from working in the EP lab during pregnancy?’ addressed to those women who declared having stayed out of the EP lab during pregnancy.
Seventeen women continued to work at the EP lab during a certain period of their pregnancy (coming from France, Germany, Mexico, Poland, Portugal, Romania, and Spain). Among them, 16 were physicians and 1 nurse. Of them, 18.8% (3) participated in only zero-fluoroscopy procedures, 33.8% (7) in both zero-fluoroscopy and use-of-radiation procedures, and 37.5% (6) in only use-of-radiation procedures (Figure 4A). Seven women (43.8%) declared having performed less than 10 procedures requiring the use of radiation, while five (31.3%) performed between 10 and 50 procedures, and four (25.0%) more than 50 procedures requiring radiation.
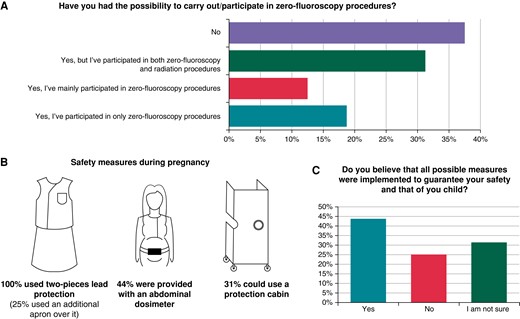
Results from questions addressed to women who had continued to work in the EP lab during pregnancy. Panel A shows the proportion of pregnant EP women who could participate in zero-fluoroscopy procedures. Panel B shows the results from the specific safety measures used by pregnant EP women who continued to work. Panel C represents the answers to the question ‘Do you think that all possible necessary measures were implemented to guarantee your safety and that of your child?’.
Most of them, 52.9% (9), were not provided with an abdominal dosimeter, and only four were provided with a continuous dosimeter. 37.5% (6) did not obtain any information about the dose of radiation received during the pregnancy period. Among those who received information about the radiation dose, this information was given with a monthly or more frequent periodicity in 50% (6) of cases. The remaining participants received this information less frequently or did not receive it at all. They all wore a two-piece lead apron (vest and skirt), and four of them (25%) wore an additional apron over it. Out of them, only in five (31.3%) cases the occupational hazards department had previously guaranteed the integrity of the lead aprons and only in three (18.8%) cases they had been provided with new aprons according to their size as the pregnancy progressed. Five (31.2%) of them could work with a lead cabin for radiologic protection (Figure 4B). The majority of them (81.3%) declared having made some modifications in their practice to reduce radiation exposure. When asked specifically about the dose received, 12 women declared that it never exceeded the limit permitted during pregnancy (80%), while three (20%) of them did not know this information, and none of the answered it had exceeded the limit permitted. However, a discrepancy was found with this regard, since there was a different question asking about the reason to decide to stop working in the EP lab and one participant answered ‘because the dose exceeded the limit permitted’. Only four declared the exact dose received, which was 0 mSv/mGy in all cases. Although 81.3% (13) believed that exposure to radiation did not alter the normal course of the pregnancy [and 18.8% (3) were not sure], only 43.8% (7) had the impression that all possible necessary measures to guarantee their safety and that of the baby had been implemented (Figure 4C).
Women who have not been pregnant during their professional career
Among the 62 female participants who had not been pregnant during their professional career, radiation exposure during pregnancy represents a concern for 73.8% (45) of them, and consequently, 18.0% (11) of them dismiss the possibility of having a pregnancy (Figure 5A). The main sources of concern are foetal and child safety in 51.7% (30) of cases, followed by a negative impact on their professional career [29.3% (17)].
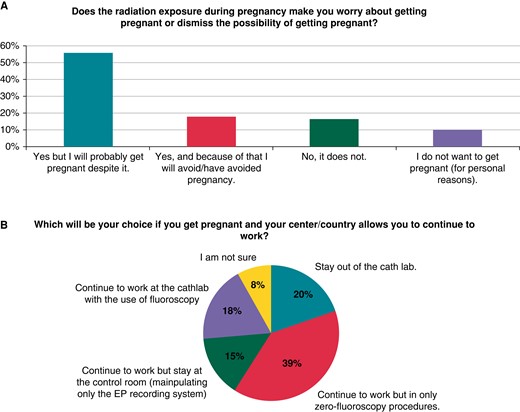
Results from questions addressed to women who had not been pregnant during their professional career.
When they were asked about their choice in case they became pregnant, only 18.0% (11) would continue to work carrying out procedures with the use of radiation. Among the remaining, most of them [39.3% (24)] would participate in only zero-fluoroscopy procedures, 14.8% (9) would continue to work at the EP lab but restricted to the control room, and 19.7% (12) would stay out of the EP lab (Figure 5B).
Missing answer handling
Throughout the survey, it was found that some questions had missing answers; however, the maximum number of missing answers detected per question was 2. Since the number of missing answers was very low and only impacted a few questions, the response percentages for each question were calculated based on the total valid responses, excluding the missing ones.
Discussion
This EHRA survey aimed to explore the current situation regarding the degree of awareness and concern about the occupational radiation effects on reproductive capacity and pregnancy, and the different policies and safety measures that are currently implemented. The main findings of the study were that there is a high degree of concern among EP staff about the harmful effects of radiation on reproductive capacity, diseases in offspring, and pregnancy and that the implementation of the safety measures with regard to pregnancy and occupational radiation exposure is very heterogenous between countries (Graphical abstract).
Radiation protection training
Most respondents (82.5%) declared having already received a regulated training in radiation protection (mandatory in 76.9% of cases). Nevertheless, basic safety measures as low-body shield addressed for gonadal protection are not systematically implemented in almost 20% of cases. Of note, only 24.5% of men knew about the radiation threshold beyond which semen quality is affected, although 70% expressed their concern about it. The results reflect an inadequate level of awareness and compliance with standard safety measures and could suggest that radiation protection training programmes might need to deepen their content and attention to the effects on reproductive capacity, pregnancy, and offspring mutations to sufficiently address this issue.
Radiation regulation and safety measures during pregnancy
Official European bodies have issued policies and regulations that allow pregnant women to continue to work with the use of occupational radiation during pregnancy by guaranteeing their safety and that of their child, as long as certain measures (total dose received < 1 mSv along the pregnancy with at least a monthly dosimeter follow-up) are complied with.6 The EHRA 2017 consensus document replicated these regulations adapted to the EP field8 and so have the 2022 EAPCI position statement in collaboration with EHRA9 and a recent review about pregnancy and interventional cardiology by Cheney AE et al.10 Yet, 80% of participants think that working with the use of radiation during pregnancy is not safe, and in many cases, EP women are not allowed to continue to work in the EP lab. A possible explanation for this may be an overestimation of the teratogenic risk associated with radiation, as it was found in a previous survey that compared the real teratogenic risk of radiation with the perceived risk by healthcare personnel.11
Remarkably, implementation of ICRP recommendations and European Directive 2013/59/Euratom is heterogeneous between European countries. When it was asked whether it was or not allowed to work with radiation during pregnancy, discrepancies (both ‘yes’ and ‘no’) were detected in the answers of 12 countries. In addition, women from the same country answered that they had been allowed to work with radiation during pregnancy and others had not. These data clearly reflect the heterogeneous law implementation in different regions or hospitals. However, the discrepancies found in the answers in this physician-based survey prevent calculation of the real proportion of countries where it is allowed to work during pregnancy, which also exceeds the scope of this survey.
Half of the women who continued to work during pregnancy obtained information about the received dose less frequently than monthly, and only 43.8% felt that all necessary measures were put in place to guarantee foetal safety. Therefore, more efforts should be done by occupational health/EP departments to ensure compliance with safety measures for pregnant EP staff who wish to continue to work in the EP lab.
Most participants (74%), especially women (96.2%), believed that pregnancy and maternity leave represent a disadvantage in the professional career for EP women. In line with these results, in a recent survey conveyed in the US, it was found that 41% of women cardiologists suffered from a decrease in their salary during pregnancy or maternity leave and that 51% reported that pregnancy had adversely impacted their career;12 therefore, more efforts should be made to do away with this gender gap.
Effect of radiation on reproductive capacity and offspring and solutions to reduce its impact
Finally, both female and male EP staff have expressed their preoccupation about the effects of radiation on reproductive capacity and offspring diseases. In reference to this, recent studies and reviews have examined the risk of occupational radiation to the foetus, showing that deterministic effects occur at a dose threshold much higher than the limits permitted by the European legislation (< 1mSv) and the radiation dose that a pregnant healthcare worker would receive while wearing a protective apron in the EP lab.13,14,10 As for stochastic (probabilistic) risks, their exact magnitude is less well understood; nevertheless, based on current data, it is considered that the potential additional risk of childhood cancer resulting from occupational radiation exposure to the foetus, when all safety measures are followed and the total received dose is <1 mSv, is negligible.15,8
Furthermore, small retrospective studies16,14 have indicated no significant variance in foetal loss rates between women exposed to occupational hazards and the general population, although there is a lack of prospective studies investigating the risk of miscarriage among healthcare workers exposed to occupational radiation.13
Despite this, most EP women have declared to be concerned about the potential hazards of radiation on pregnancy and 18% dismiss the idea of getting pregnant because of this.
Out of the possible approaches to combine pregnancy and EP activity, the performance of only zero-fluoroscopy procedures was chosen as the preferred option. Several studies2,3,17,18 demonstrated the safety and efficacy of a zero-fluoroscopy approach that might help to minimize the harmful effects on reproductive capacity, offspring, and pregnancy, without compromising procedural outcomes. Furthermore, recent publications have showcased the feasibility of performing more complex procedures, such as transeptal puncture19 or ablation in the left atrium,20 reducing or avoiding the use of fluoroscopy thanks to the advancements in 3D electroanatomic maps and the utilization of intracardiac echography (ICE). Nevertheless, 40% of the participants in this survey declared not performing EP procedures with a zero-fluoroscopy strategy. Thus, although its use is expanding, it is still quite low and not yet generalized.
Notably, among pregnant EP staff who continued to work in the EP lab, 81.3% affirmed that they had implemented modifications to minimize radiation usage and its impact. By optimizing the use of radiation, there is a significant reduction in the dose received by the operator during the procedure.8,15 Previous surveys conducted in Italy21 and at the European level22 have already examined the measures implemented by EP physicians to optimize and reduce radiation doses, identifying areas where improvement is still needed. This is primarily attributed to insufficient adherence to measures such as working with low frame rates, overusing the left anterior oblique projection, limited adoption of 3D navigation systems, and low attendance at radiation training courses.21,22 Various publications23–26 propose multiple strategies for reducing radiation exposure, which are crucial for ensuring radiation protection during pregnancy in the EP lab.13
Key areas for improvement
This survey has revealed a lack of knowledge about regulations regarding occupational radiation exposure, particularly during pregnancy, as well as a lack of systematic implementation of basic radiation protection measures. In addition, the minimum EP staff still consider pregnancy to be a disadvantage in their professional career.
Possible solutions to overcome these important issues might be as follows:
Make radiation protection training mandatory for all EP staff and ensure its content is updated and comply with the current guidelines with regard to reproductive capacity and pregnancy.
Promote the publication of consensus documents issued by official medical societies to increase awareness on this topic.
According to current legislation, further steps should be taken to reduce the gender gap and allow women to continue to keep up with work in the way of her preference during pregnancy and ensuring adequate compliance to safety measures.
Generalization of the use of 3D navigation systems and ICE may allow to reduce or suppress the use of radiation, with special interest for EP staff during pregnancy.
Limitations
Since these are survey-based results, they may be affected by several biases, such as selection bias: only those people interested in the topic may have answered the survey, therefore compromising the generalization of the results. Also, self-reported data may be inaccurate. The other limitation of this study is the absence of data regarding the working environments of the participants, such as university hospitals, non-university hospitals, private hospitals, and other relevant factors, which could have provided valuable insights into potential variations in responses.
Conclusion
The effects of occupational radiation exposure on reproductive capacity are a source of concern for EP staff (both men and women). Despite the recommendations issued by international and European bodies, the implementation of the policies regarding pregnancy and occupational radiation exposure is very heterogeneous between countries. The zero-fluoroscopy approach with the use of 3D navigation systems seems to be the preferred choice to continue to work in the EP lab during pregnancy, although its use is not yet generalized.
Supplementary material
Supplementary material is available at Europace online.
Acknowledgements
The production of this document is under the responsibility of the Scientific Initiatives Committee of the European Heart Rhythm Association: Julian K.R. Chun (Chair), Sergio Castrejon (Co-Chair), Ante Anic, Giulio Conte, Piotr Futyma, Andreas Metzner, Federico Migliore, Giacomo Mugnai, Diego Penela, Laura Perrotta, Rui Providencia, Sergio Richter, Laurent Roten, and Arian Sultan. The authors acknowledge the EHRA Scientific Research Network centres participating in this survey. A list of these centres can be found on the EHRA website.
Funding
The authors declare that no financial support was received from any organization or entity to conduct this survey.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
References
Author notes
Conflict of interest: The authors declare that there are no conflicts of interest regarding this article.



