-
PDF
- Split View
-
Views
-
Cite
Cite
A Papazoglou, A Kartas, A Samaras, I Vouloagkas, E Vrana, D Moysidis, E Akrivos, G Kotzampasis, A Papanastasiou, A Baroutidou, M Botis, C Tsagkaris, E Karagiannidis, A Tzikas, G Giannakoulas, Prognostic significance of diabetes mellitus in patients with atrial fibrillation, EP Europace, Volume 23, Issue Supplement_3, May 2021, euab116.136, https://doi.org/10.1093/europace/euab116.136
Close - Share Icon Share
Abstract
Type of funding sources: None.
Despite the plethora of studies on atrial fibrillation (AF) and diabetes mellitus (DM), there is still no sufficient data on the blood glucose regulation as a prognostic modifier in DM patients with AF.
The purpose of this study was to investigate the association of DM and levels of glycated hemoglobin (HbA1c) with outcomes in patients with AF.
This retrospective cohort study included patients who were recently hospitalized with a primary or secondary diagnosis of AF from December 2015 through June 2018. Kaplan-Meier curves and Cox-regression adjusted hazard ratios (aHR) were calculated for the primary outcome of all-cause mortality and for the secondary outcomes of cardiovascular (CV) mortality, stroke and the composite outcome of CV death or hospitalization. Spline curve models were fitted to investigate associations of HbA1c values and mortality among patients with AF and DM.
In total 1140 AF patients were included, of whom 373 (32.7%) had DM. During a median follow-up of 2.6 years, 414 (37.3%) patients died. The presence of DM was associated with a higher risk of all-cause mortality (aHR = 1.44, 95% confidence intervals [CI]: 1.12-1.85), CV mortality (aHR = 1.44, 95% CI: 1.08-1.93), stroke (aHR = 2.62, 95% CI: 1.24-5.53) and the composite outcome of hospitalization or CV death (aHR = 1.28, 95% CI: 1.06-1.54). In AF patients with comorbid DM, the spline curves showed a positive linear association between HbA1c levels and outcomes, with values <6.2% predicting significantly decreased all-cause and CV mortality.
Follow-up outcomes by presence of DM
| Outcome . | DM . | Non-DM . | Adjusted HR(95% CI) . | p-value . |
|---|---|---|---|---|
| All-cause death | 171/373 (45.8%) | 243/736 (33%) | 1.44 (1.12-1.85) | <0.001 |
| CV-death | 130/373 (34.9%) | 173/736 (23.5%) | 1.44 (1.08-1.93) | <0.001 |
| Major bleeding | 18/340 (5.3%) | 29/644 (4.5%) | 1.53 (0.71-3.28) | 0.291 |
| Stroke | 24/340 (7.1%) | 28/645 (4.3%) | 2.62 (1.24-5.53) | 0.013 |
| AF-related hospitalization | 59/340 (17.4%) | 115/645 (17.8%) | 1.20 (0.78-1.85) | 0.281 |
| HF-related hospitalization | 35/333 (10.5%) | 46/640 (7.2%) | 1.34 (0.83-2.19) | 0.235 |
| Hospitalization or CV-death | 243/373 (65.1%) | 399/736(54.2%) | 1.28 (1.06-1.54) | <0.001 |
| Outcome . | DM . | Non-DM . | Adjusted HR(95% CI) . | p-value . |
|---|---|---|---|---|
| All-cause death | 171/373 (45.8%) | 243/736 (33%) | 1.44 (1.12-1.85) | <0.001 |
| CV-death | 130/373 (34.9%) | 173/736 (23.5%) | 1.44 (1.08-1.93) | <0.001 |
| Major bleeding | 18/340 (5.3%) | 29/644 (4.5%) | 1.53 (0.71-3.28) | 0.291 |
| Stroke | 24/340 (7.1%) | 28/645 (4.3%) | 2.62 (1.24-5.53) | 0.013 |
| AF-related hospitalization | 59/340 (17.4%) | 115/645 (17.8%) | 1.20 (0.78-1.85) | 0.281 |
| HF-related hospitalization | 35/333 (10.5%) | 46/640 (7.2%) | 1.34 (0.83-2.19) | 0.235 |
| Hospitalization or CV-death | 243/373 (65.1%) | 399/736(54.2%) | 1.28 (1.06-1.54) | <0.001 |
*Adjusted for: age, gender, smoking, BMI, history of hypertension, eGFR (CKD-EPI) and use of statin, ACEI-ARB, OAC and rate control medication after discharge.
DM, diabetes mellitus; HR, hazard ratio; AF, atrial fibrillation; CV, cardiovascular; HF, heart failure.
Follow-up outcomes by presence of DM
| Outcome . | DM . | Non-DM . | Adjusted HR(95% CI) . | p-value . |
|---|---|---|---|---|
| All-cause death | 171/373 (45.8%) | 243/736 (33%) | 1.44 (1.12-1.85) | <0.001 |
| CV-death | 130/373 (34.9%) | 173/736 (23.5%) | 1.44 (1.08-1.93) | <0.001 |
| Major bleeding | 18/340 (5.3%) | 29/644 (4.5%) | 1.53 (0.71-3.28) | 0.291 |
| Stroke | 24/340 (7.1%) | 28/645 (4.3%) | 2.62 (1.24-5.53) | 0.013 |
| AF-related hospitalization | 59/340 (17.4%) | 115/645 (17.8%) | 1.20 (0.78-1.85) | 0.281 |
| HF-related hospitalization | 35/333 (10.5%) | 46/640 (7.2%) | 1.34 (0.83-2.19) | 0.235 |
| Hospitalization or CV-death | 243/373 (65.1%) | 399/736(54.2%) | 1.28 (1.06-1.54) | <0.001 |
| Outcome . | DM . | Non-DM . | Adjusted HR(95% CI) . | p-value . |
|---|---|---|---|---|
| All-cause death | 171/373 (45.8%) | 243/736 (33%) | 1.44 (1.12-1.85) | <0.001 |
| CV-death | 130/373 (34.9%) | 173/736 (23.5%) | 1.44 (1.08-1.93) | <0.001 |
| Major bleeding | 18/340 (5.3%) | 29/644 (4.5%) | 1.53 (0.71-3.28) | 0.291 |
| Stroke | 24/340 (7.1%) | 28/645 (4.3%) | 2.62 (1.24-5.53) | 0.013 |
| AF-related hospitalization | 59/340 (17.4%) | 115/645 (17.8%) | 1.20 (0.78-1.85) | 0.281 |
| HF-related hospitalization | 35/333 (10.5%) | 46/640 (7.2%) | 1.34 (0.83-2.19) | 0.235 |
| Hospitalization or CV-death | 243/373 (65.1%) | 399/736(54.2%) | 1.28 (1.06-1.54) | <0.001 |
*Adjusted for: age, gender, smoking, BMI, history of hypertension, eGFR (CKD-EPI) and use of statin, ACEI-ARB, OAC and rate control medication after discharge.
DM, diabetes mellitus; HR, hazard ratio; AF, atrial fibrillation; CV, cardiovascular; HF, heart failure.
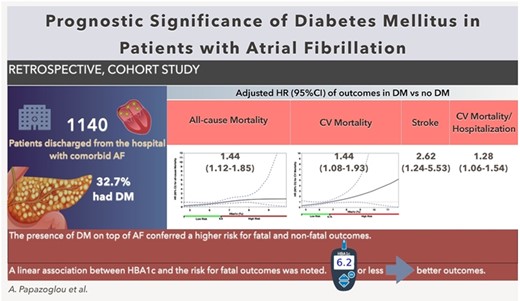
Abstract Figure. Visual overview of the study
- angiotensin-converting enzyme inhibitors
- atrial fibrillation
- smoking
- hypertension
- body mass index procedure
- statins
- diabetes mellitus
- hemorrhage
- cerebrovascular accident
- ischemic stroke
- heart failure
- hemoglobin
- cardiovascular system
- comorbidity
- follow-up
- hemoglobin a, glycosylated
- aryl hydrocarbon receptor
- survival rate
- blood glucose
- diagnosis
- morbidity
- mortality
- patient prognosis
- gender
- cox proportional hazards models
- creatinine-based formula (ckd-epi)
- primary outcome measure
- composite outcomes



