-
PDF
- Split View
-
Views
-
Cite
Cite
Christine Alonso, Christelle Marquie, Pascal Defaye, Nicolas Clementy, Pierre Mondoly, Nicolas Sadoul, Serge Boveda, Françoise Hidden-Lucet, Antoine Dompnier, Antoine Da Costa, Eloi Marijon, Christophe Leclercq, Guillaume Caudron, Olivier Piot, Jean-Claude DEHARO, “groupe Rythmologie—Stimulation cardiaque de la société française de cardiologie”, FRAGILE: FRench Attitude reGistry in case of ICD LEad replacement, EP Europace, Volume 23, Issue 3, March 2021, Pages 389–394, https://doi.org/10.1093/europace/euaa290
Close - Share Icon Share
Abstract
FRench Attitude reGistry in case of ICD LEad replacement (FRAGILE) registry was set-up to describe the attitude in different French institutions in case of implantable cardioverter-defibrillator (ICD) lead replacement, extraction, or abandonment and to compare outcomes in both groups.
Prospective observational study comparing two attitudes in case of ICD lead replacement, extraction, or abandonment. Primary endpoint describes the attitude in different French centres, collect parameters that may influence the decision. Secondary endpoint compares early and mid-term (2 years) complications in both groups.
Between April 2013 and April 2017, 552 patients were included in 32 centres. 434 (78.6%) were male, mean patient’s age was 60.3 ± 14.4 years. In 56.9% of the cases, the decision was to explant the lead. Patients in the extraction group were younger than in the abandonment group (56.7 ± 14.5 vs. 65 ± 12.7 P < 0.0001) and less likely to have comorbidities (46.5% vs. 58.3% of the patients P = 0.022). The mean lead dwelling time was significantly longer in the abandonment group as compared with the extraction group (7.6 ± 3.9 vs. 5.2 ± 3.1 years, P < 0.0001). There was no statistical difference between both groups concerning early and 2 years complications.
In this registry, the strategy in case of non-infected ICD lead replacement was mainly influenced by patient’s age and comorbidities and lead dwelling time. No difference was observed in outcomes in both strategies.
In this prospective registry, among 552 patients included in 32 centres there was a rather even proportion of extracted and abandoned leads.
Decision to extract or abandon the lead was mainly influenced by operator experience in lead extraction, patient’s age and comorbidities, and lead dwelling time that is coherent with data from published surveys.
We found no significant difference in early and 2 years outcomes.
Introduction
In 2016, there were >105.000 implantable cardioverter-defibrillator (ICD) implanted in Europe and the ICD implant rates increases over years with, in a decade, an estimated increase in ICD implant rate ranging from 11% to 228% according to the country.1 The lead is still the most vulnerable component of ICD. The cumulative lead survival rate at 5 years is ∼85–89%.2–4 The main cause of lead failure is fracture, mainly by insulation defect, beside abnormal electrical parameters (impedance, sensing, and pacing thresholds), with lead failure annual rates of >10% for an 8-year-old lead and 20% for a 10-year-old lead.5,6 Higher lead dysfunction rates are observed with advisory leads such as Sprint Fidelis and Riata.7–9 Moreover, preventive replacement can be proposed for a still functioning advisory lead, especially during elective generator replacement.10 Consequently, ICD lead’s replacement is a common situation in which the physician has to decide either to extract or to cap the lead. We anticipate that transvenous lead extraction (TLE) should be associated with higher periprocedural morbidity and that lead abandonment may lead to long-term complications. Thus, comparison of both options is difficult and the potential benefit of TLE in this context is hard to grasp. Furthermore, the decision to extract or abandon the lead may be influenced by several parameters: patient-related, lead-related, physician-related that may in turn influence patient’s prognosis. In this context, the FRAGILE registry was set-up to describe the attitude in different French centres in case of ICD lead replacement; extraction vs. abandonment.
Methods
FRench Attitude reGistry in case of ICD LEad replacement (FRAGILE) is a prospective observational study comparing two attitudes in case of ICD lead replacement; extraction or capping and abandonment.
Participating centres: every French centre experienced with ICD implantation (>50/year) and willing to participate.
Inclusion period: 4 years.
Follow-up: 2 years.
Inclusion criteria: every informed patient needing an ICD lead replacement except in case of an infection.
Primary endpoint: describe the attitude in different French centres, collect patient-related and lead-related parameters that may influence the decision.
Secondary endpoint: compare early and mid-term (2 years) complications in both groups.
Perioperative complications were defined as complications occurring during or early after intervention during initial hospitalization. A major complication was defined as a complication requiring reintervention or leading to patient’s death.
Statistical analysis
Categorical data were presented as numbers and percentages. Quantitative data were presented as mean ± standard deviation (or as median + inter-quartile range when skewed). For univariate analyses, differences between the two groups were tested using χ2 tests for categorical data and using student's t-tests or Mann–Whitney non-parametric tests for quantitative data. Factors associated with extraction with P < 0.15 in univariate analyses were taken into account for multivariate analyses, and factors independently associated with the extraction decision were then studied using stepwise backward logistic regression.
Statistical signification was assumed at P < 0.05. Statistical analyses were performed using Stata Statistical Software, release 10 (StataCorp, College Station, TX, USA).
Results
Between April 2013 and April 2017, 552 patients were included in 32 centres. The majority of them was public hospitals (78%) (Supplementary material online, Appendix S1). By centre, the mean number of ICD implants per year was 70 ± 57 (50–228) and the mean number of extractions performed per year was 24.6 ± 22.6 (0–100).
The reason for lead replacement was a lead fracture in 236 patients (43.6%) and 109 patients had an inappropriate shock. In all, 85 patients (15.9%) had a recalled ICD lead without any electrical abnormalities at the time of decision to replace it. In 56.9% of the cases, the decision was to explant the lead and in 43.1% to abandon it.
Each centre included at least 1 patient and the higher number of patients included in one centre was 72 (Figure 1).

Patients and device characteristics
Among the 552 patients, 434 (78.6%) were male. Mean patient’s age was 60.3 ± 14.4 years (18–91). Implantable cardioverter-defibrillator indication was primary prevention in 55.4% of the cases with 44.5% of the patients having ischaemic cardiomyopathy, 23.7%, idiopathic dilated cardiomyopathy and 8.7% no documented cardiopathy. Overall, 45.3% of the patients had a single chamber ICD, 28.8% a dual chamber, and 25.9% a cardiac resynchronization therapy defibrillator (CRT-D). Twenty-eight patients (5.1%) had at least one abandoned lead. Time to first ICD implant at the time of lead replacement was <5 years in 31.2% of the patients and >7 years in 34.6% of them. Mean follow-up duration was 19.4 ± 7.9 months and nine patients (1.6%) were lost of follow-up.
Intervention
There was a positive correlation between the annual number of extractions in a centre and its percentage of extraction in the FRAGILE registry (RhoSpearman = 0.725, P < 0.001) (Figure 2).
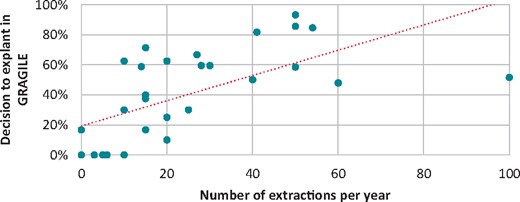
Correlation between the annual number of extractions in a centre and its percentage of extraction in the FRAGILE registry (RhoSpearman= 0.725, P<0.001). FRAGILE, FRench Attitude reGistry in case of ICD LEad replacement
When the decision was to explant the lead, the extraction success rate was of 92.3%.
Overall, 29.2% of the leads were extracted by single traction, 15.5% using a locking stylet, and 47.4% required a sheath. A laser-powered sheath was used in 18% of the patients, thus representing the most common technique when using a sheath. The venous permeability was checked prior intervention, either by a phlebography or by a doppler, in 21.9% of the patients in the extraction group and 16.1% of the patients in the abandonment group. A stenosis or occlusion was observed in 28.6% of the patients in whom the venous permeability was checked. The new implanted lead was in 73.9% of the patients a single coil active-fixation ICD lead. A subcutaneous system was chosen in 10.4% of the patients and no new lead was implanted in 1.8% of the cases. The mean intervention duration was longer in the extraction group as compared with the abandonment one (92.4 ± 48.6 vs. 68.7 ± 36.9 min, P < 0.001) as was the irradiation time (median 4.4 vs. 3 min, P < 0.001).
Comparison of both groups
The patients’ characteristics are reported in Table 1. Patients in the extraction group were younger than in the abandonment group (56.7 ± 14.5 vs. 65 ± 12.7 P < 0.0001) and were less likely to have comorbidities (46.5% vs. 58.3% of the patients P = 0.022) than in the abandonment group. Table 2 summarizes the device and leads characteristics prior lead replacement. The mean lead dwelling time was longer in the abandonment group than in the extraction group (7.6 ± 3.9 vs. 5.2 ± 3.1 years, P < 0.001) and the percentage of old leads implanted for ≥7 years was higher in the abandonment group than in the extraction group (55.4% vs. 26% P < 0.0001). By contrast neither the number of leads in place nor the type of ICD lead (active or passive fixation, single, or dual-coil) statistically differed among both groups.
| . | Abandonment . | Extraction . | P (univariate analysis) . | P (multivariate analysis) . |
|---|---|---|---|---|
| Male | 78.1% | 79% | NS | NS |
| Age | 65 ± 12.7 | 56.7 ± 14.5 | <0.0001 | <0.0001 |
| BMI | 27 ± 4.9 | 26.6 ± 5.4 | NS | NS |
| Ischaemic cardiopathy | 49.6% | 40.5% | 0.03 | NS |
| Presence of comorbiditiesa | 58.3% | 46.5% | 0.006 | 0.022 |
| Anticoagulants | 36.3% | 28.4% | NS | NS |
| . | Abandonment . | Extraction . | P (univariate analysis) . | P (multivariate analysis) . |
|---|---|---|---|---|
| Male | 78.1% | 79% | NS | NS |
| Age | 65 ± 12.7 | 56.7 ± 14.5 | <0.0001 | <0.0001 |
| BMI | 27 ± 4.9 | 26.6 ± 5.4 | NS | NS |
| Ischaemic cardiopathy | 49.6% | 40.5% | 0.03 | NS |
| Presence of comorbiditiesa | 58.3% | 46.5% | 0.006 | 0.022 |
| Anticoagulants | 36.3% | 28.4% | NS | NS |
Hypertension, diabetes, renal failure, or atrial fibrillation.
| . | Abandonment . | Extraction . | P (univariate analysis) . | P (multivariate analysis) . |
|---|---|---|---|---|
| Male | 78.1% | 79% | NS | NS |
| Age | 65 ± 12.7 | 56.7 ± 14.5 | <0.0001 | <0.0001 |
| BMI | 27 ± 4.9 | 26.6 ± 5.4 | NS | NS |
| Ischaemic cardiopathy | 49.6% | 40.5% | 0.03 | NS |
| Presence of comorbiditiesa | 58.3% | 46.5% | 0.006 | 0.022 |
| Anticoagulants | 36.3% | 28.4% | NS | NS |
| . | Abandonment . | Extraction . | P (univariate analysis) . | P (multivariate analysis) . |
|---|---|---|---|---|
| Male | 78.1% | 79% | NS | NS |
| Age | 65 ± 12.7 | 56.7 ± 14.5 | <0.0001 | <0.0001 |
| BMI | 27 ± 4.9 | 26.6 ± 5.4 | NS | NS |
| Ischaemic cardiopathy | 49.6% | 40.5% | 0.03 | NS |
| Presence of comorbiditiesa | 58.3% | 46.5% | 0.006 | 0.022 |
| Anticoagulants | 36.3% | 28.4% | NS | NS |
Hypertension, diabetes, renal failure, or atrial fibrillation.
| . | Abandonment (%) . | Extraction (%) . | P (univariate analysis) . | P (multivariate analysis) . |
|---|---|---|---|---|
| Device on a right position | 3.8 | 9 | 0.01 | 0.025 |
| Type of device | NS | NS | ||
| Single-chamber | 45.9 | 44.8 | ||
| Dual-chamber | 26.4 | 30.6 | ||
| CRT-D | 27.7 | 24.5 | ||
| >2 leads | 28.1 | 25.5 | NS | NS |
| Type of lead | NS | NS | ||
| Dual coil—active fixation | 32 | 25.5 | ||
| Dual coil—passive fixation | 6.3 | 5.8 | ||
| Single coil—active fixation | 58.7 | 66.8 | ||
| Single coil—passive fixation | 2.9 | 1.9 | ||
| Lead dwelling time | <0.0001 | <0.001 | ||
| <4 years | 14.3 | 35.6 | ||
| 4–6 years | 30.3 | 38.4 | ||
| ≥7 years | 55.4 | 26 |
| . | Abandonment (%) . | Extraction (%) . | P (univariate analysis) . | P (multivariate analysis) . |
|---|---|---|---|---|
| Device on a right position | 3.8 | 9 | 0.01 | 0.025 |
| Type of device | NS | NS | ||
| Single-chamber | 45.9 | 44.8 | ||
| Dual-chamber | 26.4 | 30.6 | ||
| CRT-D | 27.7 | 24.5 | ||
| >2 leads | 28.1 | 25.5 | NS | NS |
| Type of lead | NS | NS | ||
| Dual coil—active fixation | 32 | 25.5 | ||
| Dual coil—passive fixation | 6.3 | 5.8 | ||
| Single coil—active fixation | 58.7 | 66.8 | ||
| Single coil—passive fixation | 2.9 | 1.9 | ||
| Lead dwelling time | <0.0001 | <0.001 | ||
| <4 years | 14.3 | 35.6 | ||
| 4–6 years | 30.3 | 38.4 | ||
| ≥7 years | 55.4 | 26 |
CRT-D, cardiac resynchronization therapy defibrillator.
| . | Abandonment (%) . | Extraction (%) . | P (univariate analysis) . | P (multivariate analysis) . |
|---|---|---|---|---|
| Device on a right position | 3.8 | 9 | 0.01 | 0.025 |
| Type of device | NS | NS | ||
| Single-chamber | 45.9 | 44.8 | ||
| Dual-chamber | 26.4 | 30.6 | ||
| CRT-D | 27.7 | 24.5 | ||
| >2 leads | 28.1 | 25.5 | NS | NS |
| Type of lead | NS | NS | ||
| Dual coil—active fixation | 32 | 25.5 | ||
| Dual coil—passive fixation | 6.3 | 5.8 | ||
| Single coil—active fixation | 58.7 | 66.8 | ||
| Single coil—passive fixation | 2.9 | 1.9 | ||
| Lead dwelling time | <0.0001 | <0.001 | ||
| <4 years | 14.3 | 35.6 | ||
| 4–6 years | 30.3 | 38.4 | ||
| ≥7 years | 55.4 | 26 |
| . | Abandonment (%) . | Extraction (%) . | P (univariate analysis) . | P (multivariate analysis) . |
|---|---|---|---|---|
| Device on a right position | 3.8 | 9 | 0.01 | 0.025 |
| Type of device | NS | NS | ||
| Single-chamber | 45.9 | 44.8 | ||
| Dual-chamber | 26.4 | 30.6 | ||
| CRT-D | 27.7 | 24.5 | ||
| >2 leads | 28.1 | 25.5 | NS | NS |
| Type of lead | NS | NS | ||
| Dual coil—active fixation | 32 | 25.5 | ||
| Dual coil—passive fixation | 6.3 | 5.8 | ||
| Single coil—active fixation | 58.7 | 66.8 | ||
| Single coil—passive fixation | 2.9 | 1.9 | ||
| Lead dwelling time | <0.0001 | <0.001 | ||
| <4 years | 14.3 | 35.6 | ||
| 4–6 years | 30.3 | 38.4 | ||
| ≥7 years | 55.4 | 26 |
CRT-D, cardiac resynchronization therapy defibrillator.
Complications
There was no statistical difference between both groups concerning peri-operative complications. They occurred in 7.9% of the patients in the abandonment group and 6.5% in the extraction group (NS). The major complication rates neither differed between the two groups; 3.6% in the extraction group and 2.6% in the abandonment group. There was one death in the extraction group and none in the abandonment group. One tamponade was observed in the abandonment group and three venous injuries in the extraction group. Early complications in both groups are detailed Table 3.
| . | Abandonment . | Extraction . |
|---|---|---|
| Total | 19 | 20 |
| Death | 0 | 1 |
| Tamponade | 1 | 0 |
| Venous injury | 0 | 3 |
| Transfusion | 0 | 3 |
| Other (with no need for reintervention)a | 18 | 17 |
| . | Abandonment . | Extraction . |
|---|---|---|
| Total | 19 | 20 |
| Death | 0 | 1 |
| Tamponade | 1 | 0 |
| Venous injury | 0 | 3 |
| Transfusion | 0 | 3 |
| Other (with no need for reintervention)a | 18 | 17 |
Pocket haematoma, lead dislodgment (other than the explanted RV lead), fever, pneumothorax, heart failure decompensation, and pericardial effusion.
| . | Abandonment . | Extraction . |
|---|---|---|
| Total | 19 | 20 |
| Death | 0 | 1 |
| Tamponade | 1 | 0 |
| Venous injury | 0 | 3 |
| Transfusion | 0 | 3 |
| Other (with no need for reintervention)a | 18 | 17 |
| . | Abandonment . | Extraction . |
|---|---|---|
| Total | 19 | 20 |
| Death | 0 | 1 |
| Tamponade | 1 | 0 |
| Venous injury | 0 | 3 |
| Transfusion | 0 | 3 |
| Other (with no need for reintervention)a | 18 | 17 |
Pocket haematoma, lead dislodgment (other than the explanted RV lead), fever, pneumothorax, heart failure decompensation, and pericardial effusion.
Neither statistical difference was observed for 2 years major complications incidence, with 17 deaths in each group, respectively, 9 and 8 infections, 14 and 19 reinterventions in the abandonment and in the extraction groups, and 1 superior vena cava syndrome in the extraction group (Figure 3).
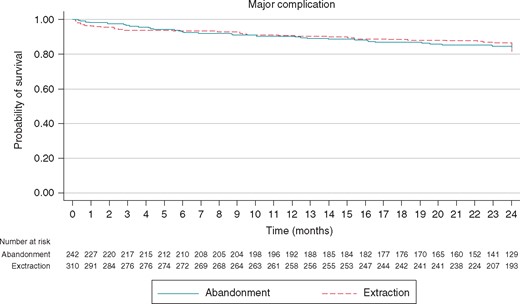
Kaplan-Meier freedom of major complication in patients with abandoned lead vs patients with extracted lead
Discussion
To our knowledge, this is the first prospective registry comparing ICD lead extraction and abandonment strategies in case of ICD lead replacement. Among the 552 patients included in 32 French centres, there was a rather even proportion of extracted (57%) and abandoned (43%) leads.
Factors influencing the decision for lead extraction
One important factor influencing the decision for extraction was the centre experience in lead extraction. We can note that an important number of centres had a low rate of procedures per year (10 centres declared an annual rate of extractions <15) and we know that low volume extraction centre is an important risk factor of complications of TLE.11,12 Among them, seven centres decide to abandon the lead in all cases in FRAGILE patients and there was a correlation between the declared annual extraction rate and the percentage of extraction in FRAGILE registry. This is coherent with findings in other registries such as the survey, published in 2009 in which personal experience had a strong influence in failing lead management beside medical literature and professional guidelines.13
Other factors influencing the decision of extracting or abandoning the lead were patient’s age, the presence of comorbidities, and the lead dwelling time. This is consistent with the results of the European survey in which patient’s age, damaged leads, and lead dwelling time were the main factors influencing the decision to extract or abandon the lead.14 Other reported risk factors for TLE complications such as female sex and number of leads are not encountered in FRAGILE registry.12,13,15 Indeed, in the FRAGILE registry, the number of leads did not influenced the decision, whereas it is the main parameter in guidelines (class IIa recommendation for lead extraction when new lead implantation would be associated with more than four leads on one side or more than five leads through the superior vena cava).12 In the present registry, the type of ICD lead (type of fixation and number of coils) did not influence the decision. In the US inquiry as in the European survey, number of leads, type of fixation, and number of coils had some influence on the decision.11,14 Dual coil leads are reported to be associated with a potential increase risk of extraction and/or to a longer and more difficult procedure.12,16
Complications and results of lead extraction
Concerning the technical aspects of lead extraction, the success rate was lower than in ELECTRa registry (92.3% vs. 95.7%). This is probably explained by indication for extraction in the ELECTRa registry that was infection in more than a half of the patients. In this indication, complete extraction is mandatory. Tools used for extraction were rather similar in both ELECTRa and FRAGILE registries except for mechanical sheaths that were less used in FRAGILE registry.13
In this registry, the peri-operative complication rate in the extraction group, was in the high range of that reported in the literature.12,13 The peri-operative complication rate in the abandonment group seems high, but is lower than reported in REPLACE registry in cohort 2 (patients with the intent to add one or more leads).17 The peri-operative and 2-year complication rates were not statistically different in both groups.
Long-term comparison of abandoned vs. extracted leads
There are several recent papers comparing complications of abandoned leads to extraction. One of them, based on the National Cardiovascular Data Registry (NCDR) ICD registry retrospectively compared ICD lead abandonment to extraction. There was a slightly higher in-hospital complications (3.77% vs. 2.19%, P < 0.001) and deaths (0.64% vs. 0.21%, P < 0.001) in patients undergoing extraction than in those with lead abandonment decision. The one-year mortality was also slightly higher in the extraction patients, but the difference was not statistically significant (11.39% vs. 8.16%, P = 0.06).18 Another study retrospectively compared extraction and abandonment of pacemaker and defibrillator leads in 488 patients and found no difference in outcomes between the two strategies with a mean follow-up of 3 years.19 Another one, also retrospectively comparing extraction vs. capping and abandoning pacing and defibrillator Leads, found similar 5 years survival in both groups with a lower risk of device infection at 5 years with extraction when compared with capping (adjusted hazard ratio, 0.78; 95% CI, 0.62–0.97; P = 0.027).20 One limitation of the two last studies is that they included pacing as well as defibrillator leads when we know that defibrillator leads extraction may be more difficult and more often require specific tools.21
Other studies assessed the impact of the presence of abandoned leads on further extraction for infection, progress. The one of the Cleveland Clinic, included >1.000 patients undergoing extraction for device infection, 23.3% had abandoned leads in place. In the presence of abandoned leads, the extraction was more complex, with longer procedures, more often the need for specialized tools, and was more likely to be incomplete.22 Otherwise, the presence of abandoned leads is associated with a higher complication rate of extraction.15,22 A sub-analysis of ELECTRa registry also reported lower procedural success rate and a higher incidence of major complications in the presence of abandoned leads at the time of TLE.23 Another retrospective analysis on 3810 patients (582 with abandoned leads) undergoing TLE found Lower procedural success rates and more frequent technical complications in the presence of abandoned leads.24
Study limitations
Although prospective this is not a randomized study. Hence, the decision for extraction was left to the physician decision with a probable bias towards a more aggressive strategy in younger, healthier patients with preferably more recent leads. This may mask higher complication rates in case of extraction. Another limitation is the short (2 years) follow-up with complications of abandoned leads may appear after a longer follow-up.
Conclusions
In our study, the decision to extract or abandon in case of non-infected ICD lead replacement was mainly influenced by operator experience in lead extraction, patient’s age and comorbidities, and lead dwelling time. No difference was observed in outcomes in both groups. Further randomized prospective studies, with long follow-up are needed to compare risks and benefits of both strategies.
Supplementary material
Supplementary material is available at Europace online.
Acknowledgements
We would like to thank “the groupe Rythmologie—Stimulation cardiaque de la société française de cardiologie.”
Funding
This study was funded by Groupe Rythmologie—Stimulation cardiaque de la société française de cardiologie.
Conflict of interest: none declared.
Data availability
Data are available on request.



