-
PDF
- Split View
-
Views
-
Cite
Cite
Anat Milman, Aviram Hochstadt, Antoine Andorin, Jean-Baptiste Gourraud, Frederic Sacher, Philippe Mabo, Sung-Hwan Kim, Giulio Conte, Elena Arbelo, Tsukasa Kamakura, Takeshi Aiba, Carlo Napolitano, Carla Giustetto, Isabelle Denjoy, Jimmy J M Juang, Shingo Maeda, Yoshihide Takahashi, Eran Leshem, Yoav Michowitz, Michael Rahkovich, Camilla H Jespersen, Yanushi D Wijeyeratne, Jean Champagne, Leonardo Calo, Zhengrong Huang, Yuka Mizusawa, Pieter G Postema, Ramon Brugada, Arthur A M Wilde, Gan-Xin Yan, Elijah R Behr, Jacob Tfelt-Hansen, Kenzo Hirao, Christian Veltmann, Antoine Leenhardt, Domenico Corrado, Fiorenzo Gaita, Silvia G Priori, Kengo F Kusano, Masahiko Takagi, Pietro Delise, Josep Brugada, Pedro Brugada, Gi-Byoung Nam, Vincent Probst, Bernard Belhassen, Time-to-first appropriate shock in patients implanted prophylactically with an implantable cardioverter-defibrillator: data from the Survey on Arrhythmic Events in BRUgada Syndrome (SABRUS), EP Europace, Volume 21, Issue 5, May 2019, Pages 796–802, https://doi.org/10.1093/europace/euy301
Close - Share Icon Share
Abstract
Data on predictors of time-to-first appropriate implantable cardioverter-defibrillator (ICD) therapy in patients with Brugada Syndrome (BrS) and prophylactically implanted ICD’s are scarce.
SABRUS (Survey on Arrhythmic Events in BRUgada Syndrome) is an international survey on 678 BrS patients who experienced arrhythmic event (AE) including 252 patients in whom AE occurred after prophylactic ICD implantation. Analysis was performed on time-to-first appropriate ICD discharge regarding patients’ characteristics. Multivariate logistic regression models were utilized to identify which parameters predicted time to arrhythmia ≤5 years. The median time-to-first appropriate ICD therapy was 24.8 ± 2.8 months. A shorter time was observed in patients from Asian ethnicity (P < 0.05), those with syncope (P = 0.001), and those with Class IIa indication for ICD (P = 0.001). A longer time was associated with a positive family history of sudden cardiac death (P < 0.05). Multivariate Cox regression revealed shorter time-to-ICD therapy in patients with syncope [odds ratio (OR) 1.65, P = 0.001]. In 193 patients (76.6%), therapy was delivered during the first 5 years. Factors associated with this time were syncope (OR 0.36, P = 0.001), spontaneous Type 1 Brugada electrocardiogram (ECG) (OR 0.5, P < 0.05), and Class IIa indication (OR 0.38, P < 0.01) as opposed to Class IIb (OR 2.41, P < 0.01). A near-significant trend for female gender was also noted (OR 0.13, P = 0.052). Two score models for prediction of <5 years to shock were built.
First appropriate therapy in BrS patients with prophylactic ICD’s occurred during the first 5 years in 76.6% of patients. Syncope and spontaneous Type 1 Brugada ECG correlated with a shorter time to ICD therapy.
In patients with Brugada syndrome who had an appropriate shock from a prophylactically implanted implantable cardioverter-defibrillator (ICD), the great majority (76.6%) received this shock during the first 5 years after ICD implantation.
Clinical parameters predicting a shorter time to appropriate shock were syncope and a spontaneous Type 1 electrocardiogram. A near-significant trend for female gender was also noted.
Two score models were built using these parameters to predict the time-to-first arrhythmic event and will need to be validated in future studies.
Introduction
Brugada Syndrome (BrS) is a well-recognized cause of sudden cardiac death (SCD) particularly in apparently healthy middle-aged males.1 The cause of death is a ventricular tachyarrhythmia usually occurring without precipitating warning signs.2 Most clinical research on this potentially lethal arrhythmic disease has mainly focused on risk stratification to identify patients at risk who will benefit from an implantable cardioverter-defibrillator (ICD), the most advocated option to prevent SCD.
Present indications for prophylactic ICD implantation in patients with BrS electrocardiogram (ECG) include3: (i) spontaneous Type 1 Brugada ECG pattern and a history of syncope (Class IIa indication) and (ii) spontaneous or drug-induced Type 1 Brugada ECG with induction of ventricular fibrillation (VF) during programmed ventricular stimulation with two or three extrastimuli (Class IIb indication). When a patient is identified as complying with these guideline recommendations,3 the most appropriate timing of the implantation is unknown with a double-edged sword decision for implant: too early might expose the patient to possible complications, whereas too late might have a detrimental outcome.
SABRUS (Survey on Arrhythmic Events in BRUgada Syndrome) is a multicentre international survey that collected data on a large cohort (n = 678) of BrS patients who experienced arrhythmic events (AE) including 252 patients in whom the AE occurred after a prophylactic ICD implantation.
The present study sought to gain insight into the factors that affect the time-to-first appropriate ICD therapy in all the 252 BrS patients who received a prophylactic ICD.
Methods
Study group
As mentioned in previous papers,1,2 the SABRUS cohort population comprised a total of 678 BrS patients with AE who were recruited from 23 centres from both 10 Western countries (426 patients; 62.8%) and 4 Asian countries (252 patients; 37.2%). In 426 patients (Group A), the AE was documented during aborted cardiac arrest (CA), while in 252 patients (Group B), the AE was documented from an ICD implanted prophylactically following conventional Class IIa or IIb indications3 (75% of patients) or non-Class IIa or IIb indications (25% of patients).2
Group B patients comprised the study group of the present study.
The study was approved by the Research Ethics Boards of all participating institutions.
Data acquisition
Anonymous patient information was collected using a predefined questionnaire regarding the following: (i) gender; (ii) patient age at time of ICD implantation; (iii) date of ICD implantation; (iv) date at which the first AE occurred after ICD implantation; (v) ethnicity (Caucasian, Asian, other, or unknown); (vi) proband status; (vii) family history of SCD; (viii) prior history of syncope; (ix) presence of spontaneous or drug-induced Brugada ECG Type 1; (x) inducibility of sustained VF at EP study (EPS); and (xi) results of genetic testing for the presence of SNC5A mutation.
Definitions
Arrhythmic events
Arrhythmic event was defined as any sustained ventricular tachyarrhythmia triggering appropriate ICD shock therapy.
Statistical analysis
Estimation of median time to AE for ordinal variables was done using Kaplan–Meier curves; significance of the difference between two curves was calculated using the log-rank test. Multivariate time to AE analysis and analysis of continuous parameters was done using Cox regression models. Calculation of each parameter effect on probability of time to AE being >5 years was done using binary logistic regression models. To prevent detection bias due to patients with longer follow-up having a longer time to AE, we added the year of ICD implantation in all of the multivariate analyses to cancel out this effect. Out of the multivariate logistic regression model, we built prediction scores using the relative odds ratios (ORs) as a guide to each parameter score. The trend between the scores and the above probability was assessed using Mantel–Haenszel test of trend and the highest-ranking scores were selected. Time to AE is shown as median ± standard error. P-values were considered significant when P < 0.05, all calculations were done using SPSS v.24 from IBM, Armonk, VA, USA.
Results
Study group
The study group comprised 252 patients aged 1.1–77.5 (mean 46.1 ± 13.3) years at time of AE, most being males (n = 229, 91%) and Caucasians (n = 160, 63.5%) (Supplementary material online, Table S1). A positive family history of SCD and a prior history of syncope were present in 29% and 63% of patients, respectively. A spontaneous Type 1 Brugada ECG was observed in 69% of patients. Most of the patients (79%) underwent an EPS during which VF was inducible in 72% of them. Genetic testing was performed in 67% of patients and revealed an SCN5A mutation in 36% of them. The age at time of ICD implantation ranged from 1 to 73.2 years (mean 43.4 ± 13.1).
Time-to-shock
The time-to-shock ranged from 0 to 168.4 months (median 24.4 ± 2.8 months), Figure 1 shows the Kaplan–Meier curves for the entire time span. Table 1 elaborates the comparison of the median time-to-shock according to different patient characteristics and Figure 2 displays the results. The following two factors were found to be associated with a significantly shorter time-to-shock: Asian vs. Caucasian ethnicity (16.5 ± 4.8 vs. 30.9 ± 16.5 months, respectively, P < 0.05) and a prior history of syncope vs. being asymptomatic (19.5 ± 2.5 vs. 36.5 ± 4.9 months, respectively, P = 0.001). In contrast a positive family history of SCD resulted in a longer time-to-shock (33.5 ± 4.8 vs. 21.2 ± 3.1 months in patients without such a history, P < 0.05).
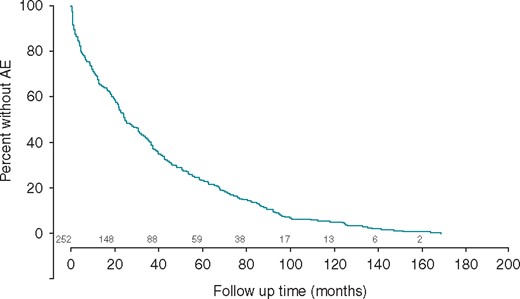
Kaplan–Meier curves for the entire time span. The percentage of patients without an AE by months of follow-up. AE, arrhythmic event.
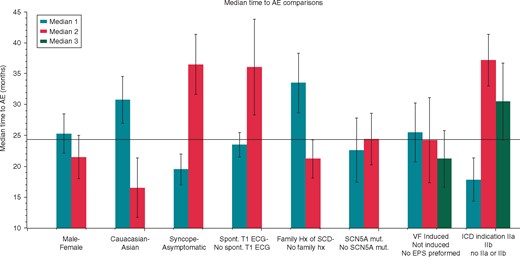
Median time-to-shock by different parameters. The median time-to-shock for the overall group was 24.4 ± 2.8 months. The figure displays the comparison of the median time-to-shock by different patient characteristics: gender, ethnicity, symptoms, ECG type, family history of SCD, mutation, EPS results, and ICD indication (see text for elaboration). AE, arrhythmic event; ECG, electrocardiogram; EPS, EP study; ICD, implantable cardioverter-defibrillator; SCD, sudden cardiac death.
| . | Time-to-shock (months), median ± SE . | P-value . |
|---|---|---|
| Overall | 24.4 ± 2.8 | |
| Gender | ||
| Male | 25.3 ± 3.2 | 0.458 |
| Female | 21.5 ± 3.5 | |
| Ethnicity | ||
| Caucasian | 30.9 ± 16.5 | 0.036 |
| Asian | 16.5 ± 4.8 | |
| Family history of SCD | ||
| Yes | 33.5 ± 4.8 | 0.019 |
| No | 21.2 ± 3.1 | |
| Prior history of syncope | ||
| Yes | 19.5 ± 2.5 | 0.001 |
| No | 36.5 ± 4.9 | |
| Spontaneous Type 1 ECG | ||
| Yes | 23.5 ± 2 | 0.258 |
| No | 36.1 ± 7.7 | |
| VF inducibility during EPS | ||
| Positive EPS | 25.5 ± 4.8 | 0.426 |
| Negative EPS | 24.2 ± 6.9 | |
| EPS not performed | 21.2 ± 4.6 | |
| Presence of SCN5A mutation | ||
| SCN5A positive | 22.6 ± 5.2 | 0.799 |
| SCN5A negative | 24.4 ± 4.2 | |
| Class of indication for ICD | ||
| IIa | 17.8 ± 3.5 | 0.003a,b |
| IIb | 37.2 ± 4.2 | |
| No IIa or IIb | 29.6 ± 2.8 | |
| . | Time-to-shock (months), median ± SE . | P-value . |
|---|---|---|
| Overall | 24.4 ± 2.8 | |
| Gender | ||
| Male | 25.3 ± 3.2 | 0.458 |
| Female | 21.5 ± 3.5 | |
| Ethnicity | ||
| Caucasian | 30.9 ± 16.5 | 0.036 |
| Asian | 16.5 ± 4.8 | |
| Family history of SCD | ||
| Yes | 33.5 ± 4.8 | 0.019 |
| No | 21.2 ± 3.1 | |
| Prior history of syncope | ||
| Yes | 19.5 ± 2.5 | 0.001 |
| No | 36.5 ± 4.9 | |
| Spontaneous Type 1 ECG | ||
| Yes | 23.5 ± 2 | 0.258 |
| No | 36.1 ± 7.7 | |
| VF inducibility during EPS | ||
| Positive EPS | 25.5 ± 4.8 | 0.426 |
| Negative EPS | 24.2 ± 6.9 | |
| EPS not performed | 21.2 ± 4.6 | |
| Presence of SCN5A mutation | ||
| SCN5A positive | 22.6 ± 5.2 | 0.799 |
| SCN5A negative | 24.4 ± 4.2 | |
| Class of indication for ICD | ||
| IIa | 17.8 ± 3.5 | 0.003a,b |
| IIb | 37.2 ± 4.2 | |
| No IIa or IIb | 29.6 ± 2.8 | |
ECG, electrocardiogram; EPS, EP study; ICD, implantable cardioverter-defibrillator; SCD, sudden cardiac death; SE, standard error; VF, ventricular fibrillation.
IIa vs. IIb, P = 0.001.
IIa vs. No, P = 0.058.
| . | Time-to-shock (months), median ± SE . | P-value . |
|---|---|---|
| Overall | 24.4 ± 2.8 | |
| Gender | ||
| Male | 25.3 ± 3.2 | 0.458 |
| Female | 21.5 ± 3.5 | |
| Ethnicity | ||
| Caucasian | 30.9 ± 16.5 | 0.036 |
| Asian | 16.5 ± 4.8 | |
| Family history of SCD | ||
| Yes | 33.5 ± 4.8 | 0.019 |
| No | 21.2 ± 3.1 | |
| Prior history of syncope | ||
| Yes | 19.5 ± 2.5 | 0.001 |
| No | 36.5 ± 4.9 | |
| Spontaneous Type 1 ECG | ||
| Yes | 23.5 ± 2 | 0.258 |
| No | 36.1 ± 7.7 | |
| VF inducibility during EPS | ||
| Positive EPS | 25.5 ± 4.8 | 0.426 |
| Negative EPS | 24.2 ± 6.9 | |
| EPS not performed | 21.2 ± 4.6 | |
| Presence of SCN5A mutation | ||
| SCN5A positive | 22.6 ± 5.2 | 0.799 |
| SCN5A negative | 24.4 ± 4.2 | |
| Class of indication for ICD | ||
| IIa | 17.8 ± 3.5 | 0.003a,b |
| IIb | 37.2 ± 4.2 | |
| No IIa or IIb | 29.6 ± 2.8 | |
| . | Time-to-shock (months), median ± SE . | P-value . |
|---|---|---|
| Overall | 24.4 ± 2.8 | |
| Gender | ||
| Male | 25.3 ± 3.2 | 0.458 |
| Female | 21.5 ± 3.5 | |
| Ethnicity | ||
| Caucasian | 30.9 ± 16.5 | 0.036 |
| Asian | 16.5 ± 4.8 | |
| Family history of SCD | ||
| Yes | 33.5 ± 4.8 | 0.019 |
| No | 21.2 ± 3.1 | |
| Prior history of syncope | ||
| Yes | 19.5 ± 2.5 | 0.001 |
| No | 36.5 ± 4.9 | |
| Spontaneous Type 1 ECG | ||
| Yes | 23.5 ± 2 | 0.258 |
| No | 36.1 ± 7.7 | |
| VF inducibility during EPS | ||
| Positive EPS | 25.5 ± 4.8 | 0.426 |
| Negative EPS | 24.2 ± 6.9 | |
| EPS not performed | 21.2 ± 4.6 | |
| Presence of SCN5A mutation | ||
| SCN5A positive | 22.6 ± 5.2 | 0.799 |
| SCN5A negative | 24.4 ± 4.2 | |
| Class of indication for ICD | ||
| IIa | 17.8 ± 3.5 | 0.003a,b |
| IIb | 37.2 ± 4.2 | |
| No IIa or IIb | 29.6 ± 2.8 | |
ECG, electrocardiogram; EPS, EP study; ICD, implantable cardioverter-defibrillator; SCD, sudden cardiac death; SE, standard error; VF, ventricular fibrillation.
IIa vs. IIb, P = 0.001.
IIa vs. No, P = 0.058.
In respect to the conventional indications of prophylactic ICD implantation,3 the shortest median time-to-shock was observed in the Class IIa subgroup (17.8 ± 3.5 months) when compared with Class IIb subgroup (37.2 ± 4.2 months, P = 0.001) or to non-IIa/IIb indications (29.6 ± 2.8 months, P = 0.058).
Univariate Cox regression for continuous variables did not find a significant relation between a shorter time-to-shock and patient age at time of ICD implantation [P = 0.285; OR 1.06; 95% confidence interval (CI) 0.96–1.17]. Multivariate Cox regression was significant for a history of syncope (P = 0.001; OR 1.65; 95% CI 1.21–2.25) and for year of ICD implantation (P < 0.001; OR 1.12; 95% CI 1.07–1.16) but not for ethnicity or family history of SCD.
Less than 5 years-to-shock time
Table 2 shows patients characteristics in respect to a 5 years-to-shock time. In 193 (76.6%) patients appropriate ICD shock therapy was delivered during the first 5 years. Univariate logistic regression (Figure 3) analyses showed that factors favouring this time lag were a prior history of syncope (P = 0.001, OR 0.36; 95% CI 0.2–0.65), the presence of a spontaneous Type 1 Brugada ECG (P < 0.05, OR 0.5; 95% CI 0.27–0.92) and the year of ICD implantation (P < 0.001; OR 0.87; 95% CI 0.82–0.94). Female gender showed a trend towards shock time less than 5 years (P = 0.052, OR 0.13; 95% CI 0.02–1.02). Multivariate Cox regression analysis was significant for all the aforementioned parameters (Supplementary material online, Table S3).
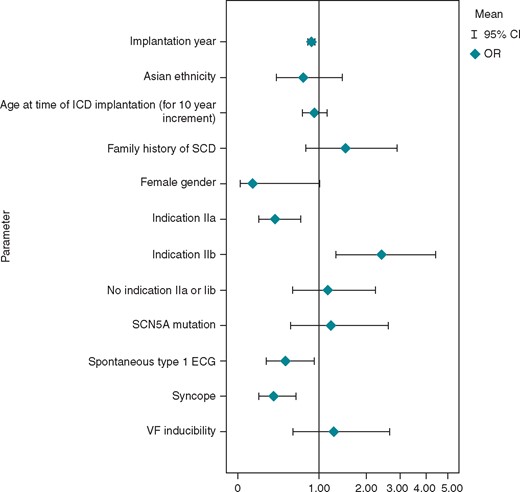
Predictors of ≤5 years to shock (OR) univariate logistic regression for factors favouring ≤5 years to shock delivery. OR, odds ratio.
Characteristics of patients in respect to the appropriate time-to-shock (less or more than 5 years) delivery
| . | Time to AE . | P-value . | |
|---|---|---|---|
| ≤5 years . | >5 years . | ||
| 193 (76.6) . | 59 (23.4) . | ||
| Gender | |||
| Male | 171 (88.6) | 58 (98.3) | 0.045 |
| Female | 22 (11.4) | 1 (1.7) | |
| Ethnicity | |||
| Caucasian | 119 (61.7) | 41 (69.5) | 0.48 |
| Asian | 62 (32.1) | 16 (27.1) | |
| Other | 4 (2.1) | 0 (0) | 0.613 |
| Unknown | 8 (4.1) | 2 (3.4) | |
| Family history of SCD | |||
| Yes | 52 (26.9) | 20 (33.9) | 0.278 |
| No | 122 (63.2) | 31 (52.5) | |
| Unknown | 19 (9.8) | 8 (13.6) | 0.571 |
| Prior history of syncope | |||
| Yes | 133 (68.9) | 26 (44.1) | 0.001 |
| No | 60 (31.1) | 33 (55.9) | |
| Spontaneous Type 1 ECG | |||
| Yes | 141 (73.1) | 34 (57.6) | 0.037 |
| No | 52 (26.9) | 25 (42.4) | |
| VF inducibility during EPS | |||
| Not performed | 42 (21.8) | 10 (16.9) | 0.538 |
| Positive EPS | 107 (70.9) | 37 (75.5) | 0.529 |
| Negative EPS | 44 (29.1) | 12 (24.5) | |
| Presence of SCN5A mutation | |||
| Not performed | 60 (31.1) | 24 (40.7) | 0.226 |
| SCN5A positive | 47 (35.3) | 14 (40) | 0.609 |
| SCN5A negative | 86 (64.7) | 21 (60) | |
| . | Time to AE . | P-value . | |
|---|---|---|---|
| ≤5 years . | >5 years . | ||
| 193 (76.6) . | 59 (23.4) . | ||
| Gender | |||
| Male | 171 (88.6) | 58 (98.3) | 0.045 |
| Female | 22 (11.4) | 1 (1.7) | |
| Ethnicity | |||
| Caucasian | 119 (61.7) | 41 (69.5) | 0.48 |
| Asian | 62 (32.1) | 16 (27.1) | |
| Other | 4 (2.1) | 0 (0) | 0.613 |
| Unknown | 8 (4.1) | 2 (3.4) | |
| Family history of SCD | |||
| Yes | 52 (26.9) | 20 (33.9) | 0.278 |
| No | 122 (63.2) | 31 (52.5) | |
| Unknown | 19 (9.8) | 8 (13.6) | 0.571 |
| Prior history of syncope | |||
| Yes | 133 (68.9) | 26 (44.1) | 0.001 |
| No | 60 (31.1) | 33 (55.9) | |
| Spontaneous Type 1 ECG | |||
| Yes | 141 (73.1) | 34 (57.6) | 0.037 |
| No | 52 (26.9) | 25 (42.4) | |
| VF inducibility during EPS | |||
| Not performed | 42 (21.8) | 10 (16.9) | 0.538 |
| Positive EPS | 107 (70.9) | 37 (75.5) | 0.529 |
| Negative EPS | 44 (29.1) | 12 (24.5) | |
| Presence of SCN5A mutation | |||
| Not performed | 60 (31.1) | 24 (40.7) | 0.226 |
| SCN5A positive | 47 (35.3) | 14 (40) | 0.609 |
| SCN5A negative | 86 (64.7) | 21 (60) | |
AE, arrhythmic event; ECG, electrocardiogram; EPS, EP study; SCD, sudden cardiac death; VF, ventricular fibrillation.
Characteristics of patients in respect to the appropriate time-to-shock (less or more than 5 years) delivery
| . | Time to AE . | P-value . | |
|---|---|---|---|
| ≤5 years . | >5 years . | ||
| 193 (76.6) . | 59 (23.4) . | ||
| Gender | |||
| Male | 171 (88.6) | 58 (98.3) | 0.045 |
| Female | 22 (11.4) | 1 (1.7) | |
| Ethnicity | |||
| Caucasian | 119 (61.7) | 41 (69.5) | 0.48 |
| Asian | 62 (32.1) | 16 (27.1) | |
| Other | 4 (2.1) | 0 (0) | 0.613 |
| Unknown | 8 (4.1) | 2 (3.4) | |
| Family history of SCD | |||
| Yes | 52 (26.9) | 20 (33.9) | 0.278 |
| No | 122 (63.2) | 31 (52.5) | |
| Unknown | 19 (9.8) | 8 (13.6) | 0.571 |
| Prior history of syncope | |||
| Yes | 133 (68.9) | 26 (44.1) | 0.001 |
| No | 60 (31.1) | 33 (55.9) | |
| Spontaneous Type 1 ECG | |||
| Yes | 141 (73.1) | 34 (57.6) | 0.037 |
| No | 52 (26.9) | 25 (42.4) | |
| VF inducibility during EPS | |||
| Not performed | 42 (21.8) | 10 (16.9) | 0.538 |
| Positive EPS | 107 (70.9) | 37 (75.5) | 0.529 |
| Negative EPS | 44 (29.1) | 12 (24.5) | |
| Presence of SCN5A mutation | |||
| Not performed | 60 (31.1) | 24 (40.7) | 0.226 |
| SCN5A positive | 47 (35.3) | 14 (40) | 0.609 |
| SCN5A negative | 86 (64.7) | 21 (60) | |
| . | Time to AE . | P-value . | |
|---|---|---|---|
| ≤5 years . | >5 years . | ||
| 193 (76.6) . | 59 (23.4) . | ||
| Gender | |||
| Male | 171 (88.6) | 58 (98.3) | 0.045 |
| Female | 22 (11.4) | 1 (1.7) | |
| Ethnicity | |||
| Caucasian | 119 (61.7) | 41 (69.5) | 0.48 |
| Asian | 62 (32.1) | 16 (27.1) | |
| Other | 4 (2.1) | 0 (0) | 0.613 |
| Unknown | 8 (4.1) | 2 (3.4) | |
| Family history of SCD | |||
| Yes | 52 (26.9) | 20 (33.9) | 0.278 |
| No | 122 (63.2) | 31 (52.5) | |
| Unknown | 19 (9.8) | 8 (13.6) | 0.571 |
| Prior history of syncope | |||
| Yes | 133 (68.9) | 26 (44.1) | 0.001 |
| No | 60 (31.1) | 33 (55.9) | |
| Spontaneous Type 1 ECG | |||
| Yes | 141 (73.1) | 34 (57.6) | 0.037 |
| No | 52 (26.9) | 25 (42.4) | |
| VF inducibility during EPS | |||
| Not performed | 42 (21.8) | 10 (16.9) | 0.538 |
| Positive EPS | 107 (70.9) | 37 (75.5) | 0.529 |
| Negative EPS | 44 (29.1) | 12 (24.5) | |
| Presence of SCN5A mutation | |||
| Not performed | 60 (31.1) | 24 (40.7) | 0.226 |
| SCN5A positive | 47 (35.3) | 14 (40) | 0.609 |
| SCN5A negative | 86 (64.7) | 21 (60) | |
AE, arrhythmic event; ECG, electrocardiogram; EPS, EP study; SCD, sudden cardiac death; VF, ventricular fibrillation.
Opposite results were found between the Class IIa and IIb indications for prophylactic ICD implantation: a Class IIa indication was a significant predictor for ≤5 years-to-appropriate shock (P < 0.01; OR 0.38; 95% CI 0.2–0.71), whereas a Class IIb indication was a significant predictor for >5 years-to-appropriate shock (P < 0.01; OR 2.41; 95% CI 1.32–4.22) (Figure 3).
Time-to-shock score
Taking into consideration the aforementioned patients’ characteristics predicting a time-to-shock ≤5 years, their relative OR, and parameter significance, two risks scores were built. One with a history of syncope and spontaneous Type 1 Brugada ECG (minimal score) and the second with female gender added, as it had a borderline significance, yet we postulated it could add power to the score (gender augmented score).
These Scores sum the risk factors found to have significance for an earlier AE after a prophylactic ICD implantation. Each risk factor received a score between 1 and 2 and the sum gives the percentage of patients who received an appropriate therapy during the first 5 years from the implant (Figure 4). One point is given for either prior syncope or the presence of a spontaneous Type 1 Brugada ECG, and for the gender augmented score—two points were added for female gender. The scores range between 0 and 2 for the minimal score and 0 and 4 for the gender augmented score. A score of 0 was found in 50.0% of patients using the minimal score and in 46.4% of patients using the gender augmented score. A maximal score (two in the minimal score system and four in the gender augmented system) was observed in 85% and 100% of patients, respectively. The trend between the score and the percentage of patients with time-to-shock less than 5 years were highly significant for both scores (P < 0.001 for both) but reached a higher level for the gender augmented score (Mantel–Haenszel statistics of 16 and 20.1 for the minimal and the gender augmented scores, accordingly).
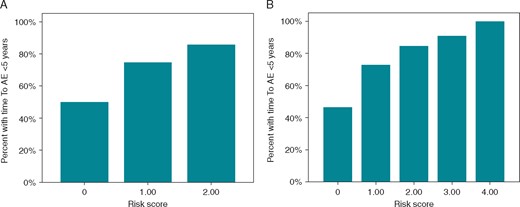
The time-to-shock score. (A) This risk score sums the following risk factors found to have significance for an earlier AE after a prophylactic ICD implantation: one point is given for either prior syncope or the presence of a spontaneous Type 1 Brugada ECG. (B) A gender augmented score, using both the above risk factors and two points for female gender. A P-value for trend between the score and the P-value of <0.001 for both scores. AE, arrhythmic event; ECG, electrocardiogram; ICD, implantable cardioverter-defibrillator.
Discussion
Our study showed that the median time-to-first appropriate ICD therapy in the 252 BrS patients who received a prophylactic ICD was 24.8 ± 2.8 months. The shortest times were observed in patients of Asian ethnicity, in those with prior syncope and in those who had a Class IIa indication for ICD implantation. The longest time was associated with a positive family history of SCD. In >3 quarters of the study patients, appropriate ICD therapy was delivered during the first 5 years after implantation, especially in patients with a female gender, those with a prior syncope and those with a spontaneous Type 1 Brugada ECG. Two score models for predicting a time-to-shock ≤5 years were built according to the significance of the parameters; one included syncope and a Type 1 Brugada ECG and the second included female gender which had a borderline significance and resulted in a 100% accuracy when patients exhibited all these characteristics.
Time-to-shock
The literature regarding the time-to-first appropriate shock therapy in BrS patients implanted prophylactically with an ICD is scarce. Only three studies report their results on small patient cohorts (ranging from 7 to 34 patients).4–6 Sarkozy et al.5 found a mean time-to-first appropriate therapy of 13 months (3 days to 4 years) in seven male patients including three with a history of syncope. They did not find a significant predictor of appropriate shock-free survival.5 In an earlier study, Sacher et al.4 demonstrated that the asymptomatic group (n = 5) had a shorter median time-to-shock (16 months) than the syncope group (n = 9) (24 months).4 However, in a latter larger study by the same group with prolonged follow-up duration, time-to-shock lengthened with no difference found between the symptomatic (47 months, n = 22) and asymptomatic (45 months, n = 12) groups.6
In the present study, which involved the largest cohort population with AEs documented after prophylactic ICD implantation (n = 252), the median time-to-shock was 24.8 months. Asian ethnicity and a history of syncope were predictors of a shorter time-to-shock, suggesting these factors should be taken into consideration when contemplating ICD implantation. This is consistent with the fact that Group IIa patients had the shortest time-to-shock.
By multivariate logistic regression the presence of syncope was found to correlate with a shorter time-to-shock (19.5 ± 2.5 months vs. 36.5 ± 4.9 months in asymptomatic patients, P < 0.001). It is noteworthy that these results are in agreement with those of the FINGER study7 where time-to-first event was reported to be significantly shorter in the syncope group patients than in the asymptomatic group.
In the present study, a positive family history of SCD correlated with a longer time-to-shock, however, these findings should be considered with caution since they were seen only in the univariate analysis and not in the multivariate one. One possible explanation could be a biased decision taken by the referring patient’s physician who considered a family history of SCD as a major risk factor. On the other hand, we already stressed elsewhere the problematic definition of family history of SCD in our study.2 Implantable cardioverter-defibrillator implant year was a predictor of early AE, mostly due to longer follow-up in patients that had an ICD implanted in the past, although this finding might also represent different trends in ICD implant indications, and changes in ICD arrhythmia detection algorithms.
Time-to-shock within 5 years
Considering the lifesaving properties of ICD in comparison to its non-negligible complication rate together with the low incidence of AE requiring ICD intervention in BrS patients implanted prophylactically, up to a 5-year time-to-shock was chosen as accounting for a well-timed implant. Our study found that syncope and a spontaneous Type 1 BrS ECG were significantly associated with time-to-shock of ≤5 years. Therefore, it is not surprising that Group IIa patients which included those with syncope and a spontaneous Type 1 BrS ECG belonged to this 5 years’ time-to-shock period. Moreover, the fact that in contrast Group IIb patients exhibited their AE more than 5 years after implantation is in congruence with the lower risk of AE found in Group IIb when compared with Group IIa patients.8
Our study showed that 96% of female patients vs. 75% of males had their AE’s ≤5 years after ICD implant. In our recent article,9 we discussed several factors suggesting a more aggressive course of the disease in females. This should support an early implantation of ICD in females found to be at high risk.
Time-to-shock score
The time-to-shock score (TScore) was created to help the identification of patients who will need an ICD implant with the shortest delays. The significant risk factors found in our study to be associated with a time-to-shock ≤5 years were attributed a score according to their statistical significance. Because female gender had a borderline significance (P = 0.052), which could be a result of the low number of females included in the study, we created two scores one including gender and one excluding it. Both scores showed high prediction rates for AE ≤5 years after ICD implant, yet the gender augmented score showed a more significant trend with a higher predictive value for the maximal score (85% for the maximal score in the minimal scoring system vs. 100% for the gender augmented system). As indicated in Figure 3, the absence of any of these risk factors, results in a risk of approximately 50% chance of exhibiting an AE ≤5 years after ICD implant. Thus, patients with a score of 0 could be implanted less urgently. On the other hand, a maximal score of 4 (i.e. a female with syncope and a spontaneous Type 1 BrS ECG) in the gender augmented system should lead to ICD implant with the shortest delays. The value of this TScore should be further validated and assessed prospectively in future studies, where the question of the influence of gender could also be assessed more accurately.
Limitations
The present study by nature is a retrospective cumulative analysis of results from the largest EP-centres with experience with BrS. The decision to implant a prophylactic ICD in those patients who did not fulfil Class II indications was left to the discretion of the treating physician. We acknowledge that defining risk factors without a comparative group of asymptomatic patients is problematic and that the results should be prospectively tested in future studies. Also, our cohort was probably not powered enough to assess the influence of female gender as resulted in a borderline significance for a time-to-shock of less than 5 years.
Conclusion
The present study describes for the first time, in a large cohort of BrS patients with AE’s documented after prophylactic ICD implantation, the characteristics of those who exhibited their AE within 5 years. Two factors (syncope and spontaneous Type 1 BrS ECG) were found to be associated with this time-to-shock delay. A score based on these factors is proposed and should be assessed prospectively.
Conflict of interest: none declared.



