-
PDF
- Split View
-
Views
-
Cite
Cite
Giuseppe Boriani, Marco Vitolo, Valentina Kutyifa, Cardiac resynchronization therapy: need to synchronize patients and device longevities with comorbidities, EP Europace, Volume 21, Issue 5, May 2019, Pages 683–685, https://doi.org/10.1093/europace/euy297
Close - Share Icon Share
This editorial refers to ‘Survival after cardiac resynchronization therapy: results from 50 084 implantations’, by F. Leyva et al., on pages 754--762.
Cardiac resynchronization therapy (CRT) started as a last resort therapeutic solution for patients with severe heart failure associated with left bundle branch block, but its development and clinical validation was relatively quick, owing to a series of randomized controlled trials with hard endpoints that constituted the basis for guideline recommendations.1,2
In this issue of EP Europace, Leyva et al.3 present a non-randomized, retrospective study exploring total mortality and relative survival after a first CRT device implantation. The authors obtained data from a data warehouse containing data on admissions to all public hospitals in England and mortality data, cross-validated with the Office of National Statistics, were retrieved over a period of 9 years. The authors present the largest study on long-term outcomes of CRT in the real world in terms of patient numbers and length of follow-up and are the first to assess survival after CRT in relation to individuals in the general population, using the concept of relative survival already applied in the oncology field. In view of the originality of their approach and the amount of data evaluated, the authors are to be commended for undertaking this study. In an analysis of over 8.8 years (median follow-up 2.7 years), focusing on 50 084 patients, with a mean age of 72 years implanted with CRT-D (n = 25 273) or CRT-P devices (n = 24 811), expected survival decreased with age and a series of clinical variables (male sex, history of ischaemic heart disease, diabetes, chronic kidney disease), as well as the burden of comorbidities, assessed by the Charlson comorbidity score, were associated with a lower relative survival.
These data on the impact of comorbidities are in line with other real-world analysis and confirm the need for evaluating the effect of treatments outside of the golden setting of randomized controlled clinical trials. In a regional registry from Italy including consecutive heart failure patients who underwent a first implant of a CRT-D device, survival free from death/cardiac transplant was 64% at 5 years, but comorbidities, as evaluated by the Charlson comorbidity index, had a significant impact on outcomes in terms of mortality, heart transplant, hospitalizations, and days spent alive and out of hospital.4 Moreover, patient age, implant during urgent, unplanned hospitalization, and a higher New York Heart Association (NYHA) class had a significant negative impact on both hospitalizations and mortality, while male sex was a predictor of mortality after CRT-D implants, in line with Leyva et al.3 and other studies.4
According to the detailed data presented by Leyva et al.,3 a mismatch is seen between device longevity and patient longevity for patients with an age <80 without severe comorbidities affecting the outcome. The problem related to a mismatch between the device service life and patient survival is of a growing importance and leads to consideration of longevity of CRT-D devices as an important target for technology improvement. Replacement of cardiac implantable devices is associated with a notable risk of complications, particularly infections, reported as the most harmful complication after CRT replacement, with an incidence of approximately 1.5–2%.5 Moreover, replacements involve incremental costs, as well as patient discomfort, and consequently extending longevity may significantly improve cost-effectiveness estimates for CRT-D therapy.5
The temporal trend evidenced by Leyva et al.3 indicates that in most recent years, mortality after CRT is decreasing, probably due to the growing use of CRT in patients with mild heart failure and improvement in pharmacological treatments and device management, a finding that further underlines the importance and the usefulness of extending device longevity. In a modelling study in a 15-year time window, an extension of device longevity for a CRT-D device can have an important impact in reducing long-term costs of device therapy, with substantial daily savings in favour of devices with extended longevity up to 30%, depending on clinical scenarios.6 Since data on longevity of devices are mainly based on projections, and therefore have some limitations, actual data from large datasets should be collected, as done by Leyva et al.,3 in order to better synchronize patient and device longevity.
In this dataset from the UK, CRT-D was associated with a higher relative survival than CRT-P both in the overall study sample and in subgroups with or without ischaemic heart disease. It is noteworthy that this analysis included a larger number of patients implanted with CRT-P compared to what can be observed in many other countries. This is related to the NICE guidelines that recommended CRT-P instead of CRT-D for patients with non-ischaemic cardiomyopathy between 2007 and 2014, with a subsequent change of this recommendation in favour of CRT-D. As a matter of fact, a great heterogeneity can be found in Europe in the proportion of the use of CRT-P and CRT-D devices, respectively (Figure 1).7 This can be interpreted as taking into account many factors, including the lack of solid evidence supporting the clinical decision to implant a CRT-D or a CRT-P device. Indeed, the comparison of outcome after implant of a CRT-P vs. a CRT-D system has been a subject of great debate, since no adequately powered data from randomized controlled trials are available.8
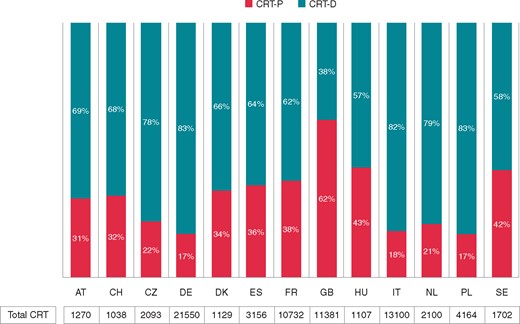
Number of CRT implants in European countries (ISO country codes) and proportions of CRT-P and CRT-D implants (data for year 2016, related to countries with at least 1000 CRT implants in the EHRA White book 2017 are shown. Data from: https://www.escardio.org/static_file/Escardio/Subspecialty/EHRA/Publications/Documents/2017/ehra-white-book-2017.pdf). CRT, cardiac resynchronization therapy.
In the study by Leyva et al.,3 relative survival was higher after CRT-D than after CRT-P in the overall group of patients, as well as in subgroups with or without ischaemic heart disease. However, it should be noted that in view of the observational nature of the study, the clinical characteristics of the patients were different, CRT-D patients were more frequently affected by ischaemic heart disease and less frequently had chronic kidney disease. In this analysis, CRT-D was associated with a lower observed mortality than CRT-P also after adjustment for age, sex, history of comorbidities, Charlson comorbidity index, history of ischaemic heart disease, and year of implantation. In another single-centre patient cohort by Kutyifa et al.,9 CRT-D was associated with a mortality benefit over CRT-P in patients with ischaemic cardiomyopathy, but no incremental benefit of CRT-D vs. CRT-P was detected in non-ischaemic cardiomyopathy. Moreover, in a retrospective analysis form Belgium,10 it emerged that the mode of death was predominantly non-cardiac in CRT-P vs. CRT-D recipients (71% vs. 38%) and that age >80 years, NYHA Class IV, intolerance to beta-blockers, and underlying non-ischaemic cardiomyopathy were independently associated with small incremental value of CRT-D over CRT-P. A large proportion of non-cardiovascular outcomes after implant of an implantable cardioverter-defibrillator or CRT-D device was found also in the study by Boriani et al.4 in terms of non-cardiovascular hospitalizations and can be interpreted as competing risk. These findings suggest the need for a further assessment of the role of CRT-D vs. CRT-P in selected patients, especially in those with non-ischaemic cardiomyopathy.
A meta-analysis of 44 studies and 18 874 patients found that the occurrence of sudden cardiac death in patients implanted with CRT-P was significantly higher in certain subgroups (males, ischaemic cardiomyopathy, NYHA class III), where CRT-D may exert a specific benefit.8 Therefore, when targeting CRT-D vs. CRT-P devices, specific considerations about risk of arrhythmic death vs. the competing risk of non-arrhythmic death need to be taken into account such as age, underlying aetiology, and comorbidities. In this perspective, CRT-P can be an appropriate choice in the very elderly, when the indication to CRT is dictated by the need to reduce heart failure hospitalizations and improve quality of life.
The implications of the study of Leyva et al.3 suggest the importance of large datasets to improve our knowledge on the outcome of patients treated with implanted devices, in order to improve patient targeting, as well as organization of care and providing the basis for economic analysis as a guide to decision-making, in line with the multidimensional approach of Health Technology Assessment.11 Even though randomized controlled trials play a central role in defining the efficacy of device treatments in specific settings of patients, which are by definition rather selected, further registry studies are needed deriving data from ‘real-world’ practice in order to obtain crucial hints to improve patient targeting, and improve patient care in a holistic approach, taking into account the important implications of comorbidities.
Conflict of interest: G.B. received speaker’s fees of small amount form Boehringer Ingelheim, Boston, Biotronik and Medtronic. V.K. received research grants from Boston Scientific, and Zoll, and consultation fees from Zoll and Biotronik.
Acknowledgement
The opinions expressed in this article are not necessarily those of the Editors of Europace or of the European Society of Cardiology.



