-
PDF
- Split View
-
Views
-
Cite
Cite
Julia W Erath, Alexander P Benz, Stefan H Hohnloser, Mate Vamos, Clinical outcomes after implantation of quadripolar compared to bipolar left ventricular leads in patients undergoing cardiac resynchronization therapy: a systematic review and meta-analysis, EP Europace, Volume 21, Issue 10, October 2019, Pages 1543–1549, https://doi.org/10.1093/europace/euz196
Close - Share Icon Share
Abstract
Some retrospective and prospective studies in heart failure patients with indication for cardiac resynchronization therapy (CRT) suggest better clinical outcomes for quadripolar (QP) left ventricular (LV) leads over bipolar (BP) leads. Although, lead failure remains an important safety concern, when using these more complex, novel electrodes. To evaluate safety and efficacy outcomes for QP vs. BP LV leads in patients receiving CRT.
We performed a comprehensive literature search through 2018 in PubMed, Cochrane Library, and Google Scholar databases to identify studies comparing patients with QP and BP LV CRT leads. A total of 12 studies were selected for analysis comprising 31 403 patients (QP lead: 22 429 patients; BP lead: 8974 patients). Eight studies examined the effects of CRT on survival. In these studies, use of QP electrodes was associated with significantly better survival compared to patients with BP LV leads (OR 0.61, 95% CI 0.50–0.76; P < 0.01). Clinical improval measured in New York Heart Association functional class (OR 0.59, 95% CI 0.34–1.01; P = 0.05) and hospitalization rates (OR 0.67, 95% CI 0.55–0.83; P < 0.01) were also improved in patients receiving QP leads. Lead malfunctions defined as LV lead failure resulting in lead deactivation (OR 0.57, 95% CI 0.34–0.98; P = 0.04) or LV lead dislodgement requiring LV lead replacement/repositioning (OR 0.48; 95% CI 0.31–0.75; P < 0.01) were more often encountered among patients with BP leads compared to patients with QP leads.
Our meta-analysis suggests distinct benefits of QP over BP electrodes in patients undergoing CRT.
Quadripolar (QP) left ventricular (LV) leads emerged as a new technology to enable pacing from up to 12 different vectors in patients with heart failure with reduced ejection fraction and indication for cardiac resynchronization therapy (CRT).
There are known challenges associated with implantation of conventional bipolar (BP) LV leads such as lead instability, high pacing thresholds, or concomitant phrenic nerve stimulation requiring surgical repositioning of the lead.
This meta-analysis comprising over 31 000 patients revealed a significant reduction in lead failure in patients with QP LV leads compared to conventional BP LV leads.
Use of QP leads was associated with reduced hospitalization rates and more frequent improvement in New York Heart Association functional status compared to use of BP LV leads.
Finally, this meta-analysis shows a significant reduction in all-cause mortality in CRT patients implanted with QP LV leads.
Introduction
Cardiac resynchronization therapy (CRT) has revolutionized heart failure therapy for selected patients demonstrating a significant reduction in both hospitalization rates1–2 and mortality.3 Cardiac resynchronization therapy is indicated in patients with heart failure with reduced ejection fraction and a wide QRS complex.4 Despite the effectiveness of CRT, there are challenges associated with implantation of the left ventricular (LV) lead, such as inability to cannulate the target vein, lead instability, high pacing thresholds, concomitant phrenic nerve stimulation (PNS), or lead dislodgement. This may necessitate lead revision/replacement or even lead deactivation.5 The first quadripolar (QP) LV lead was approved in 2011, allowing for LV pacing from up to 10 unique pacing vectors. Several retrospective, few prospective, and two randomized controlled trials suggest less lead-related complications with implantation of QP LV leads than with bipolar (BP) LV leads in patients receiving CRT.6–17 Nonetheless, there are conflicting data concerning CRT implantation duration and fluoroscopy time6,9,12,17 as well as response to CRT6,9,13,17 in patients fitted with QP vs. BP LV leads. In fact, one study analysing the manufacturer’s registry data on 23 570 patients implanted with either BP or QP LV leads showed a significant relative reduction in mortality risk of ∼20% in CRT patients receiving QP LV leads.10
Since the majority of these studies comprised relatively few patients, encountered few endpoints, and were limited by short follow-up durations, a systematic review and meta-analysis of published data appears to be timely and may provide the best way to estimate the effectiveness, safety, and clinical implications associated with implantation of QP LV leads in heart failure patients undergoing CRT.
Methods
Study selection
We performed a comprehensive search from January 2012 to July 2018 of the English literature dealing with the effects of CRT implantation of BP vs. QP LV leads (Prospero ID: CRD42018110423, NHS). In order to identify and retrieve potentially relevant articles regarding this topic, the search was performed utilizing the terms ‘quadripolar’, ‘bipolar’, ‘left ventricular lead’, and ‘CRT’ in PubMed, Cochrane Library, and Google Scholar databases. Potentially relevant articles were evaluated by two experienced independent reviewers. Any disagreement was subsequently resolved between all authors. Additional publications were identified using the reference lists of selected manuscripts.
Randomized controlled trials, case–control studies, or cohort studies were eligible for this meta-analysis if they reported data about a direct comparison of CRT patients implanted with BP or QP LV leads. Only full-sized papers in the English language, published in peer-reviewed journals were considered. Studies analysing exclusively patients with QP LV leads were excluded. Studies were considered as retrospective when not stated otherwise in the Methods section of the respective study.
Endpoints
The primary outcome measure for this meta-analysis comparing patients implanted with CRT-D or CRT-P and QP or BP LV leads was all-cause mortality. Secondary outcomes of interest were clinical response to CRT defined as improvement of at least one New York Heart Association (NYHA) functional class and hospitalization, as well as LV lead performance as assessed by LV lead deactivation, need for surgical lead repositioning, and PNS. Fluoroscopy times were also compared between the two patient groups.
Statistical analysis
Statistical analyses were conducted utilizing Review Manager version 5 (Cochrane Central, UK) and Comprehensive Meta-Analysis 2.2 (Biostat, Inc., USA). To assess all-cause mortality, Maentel–Haentzel odds ratios (OR) were calculated along with 95% confidence intervals (CI) and the two therapy groups were compared as case–control models. Publications detailing crude and/or adjusted hazard ratios (HRs) were subjected to meta-analytic assessment. Further sensitivity analysis was performed using the ‘one-study-out method’.
Maentel–Haentzel odds ratios (OR) and respective 95% confidence intervals (CI) were calculated for each outcome (lead failure, lead deactivation, PNS, hospitalization, and CRT response) comparing event rates for QP and BP LV leads. Cardiac resynchronization therapy-response was evaluated after 3–6 months after CRT implantation and measured as improvement of the NYHA functional class. Heterogeneity between individual trial estimates was assessed using the Q statistic and I2 statistic. Since there was significant heterogeneity in the design and patient characteristics of the included studies, it was assumed that the true effect size varies from one study to the other, and hence the random-effect model was applied. Forrest plots were constructed showing the individual trials with the pooled estimates. Publication bias was assessed using the funnel plot, the trim and fill method of Duval and Tweedie, and the adjusted rank correlation test according to Begg and Mazumdar.
Results
Study characteristics
From a total of 693 initially identified studies, 19 studies matched the search criteria (Supplementary material online, Figure S1). Seven studies were excluded as they compared CRT patients implanted with QP LV leads with different LV pacing modes. This yielded a total of 12 studies6–17 (Table 1) comparing heart failure patients undergoing CRT with implantation of QP vs. BP LV leads and directly comparing patients with both lead types during follow-up. These studies followed either a retrospective (n = 6)6,10,11,15–17 or a prospective design (n = 4);7,8,12,14 two studies were randomized controlled clinical trials.9,13 Of note, two studies analysed data from a similar multicentre cohort at different time frames with different endpoints.7,8 The second publication of Behar et al.8 from the same data set was only used to extract data on hospitalization.
| Study (year of publication) . | Type of study . | No. of patients included . | Mean age (years) . | Follow-up duration (months) . | Study endpoints . | Manufacturer of QP lead . |
|---|---|---|---|---|---|---|
| Arias et al. (2012) | Retrospective, single-centre study | 42 CRT-D patients (21 QP, 21 BP LV lead) | 66 ± 10 | 9 | Successful LV lead implant, lead failure, mortality, hospitalization | St. Jude Medical/Abbott |
| Behar et al. (2015) | Prospective, multi-centre study | 721 CRT-D patients (357 QP, 364 BP LV lead) | 69 ± 10 | 29 ± 1 | Successful LV lead implant, PNS, lead failure, lead revision, mortality | Boston Scientific, Medtronic, St. Jude Medical/Abbott |
| Behar et al. (2017) | Prospective, multi-centre study | 606 CRT-D patients (319 QP, 287 BP LV lead) | 69 ± 10 | 60 | Hospital readmission (CHF, ACS, arrhythmia, device explantation, lead revision, generator replacement) | St. Jude Medical/Abbott |
| Bencardino et al. (2016) | Prospective, randomized, single-centre study | 43 CRT-D patients (23 QP, 20 BP LV lead) | 69 ± 9 | 3 | Successful LV lead implant, lead failure, PNS, CRT-response (NYHA, LVEF) | St. Jude Medical/Abbott |
| Boriani et al.(MORE-CRT), (2016) | Prospective, randomized-controlled multi-centre study | 1078 CRT-D patients (718 QP, 348 BP LV lead) | 69 ± 10 | 6 | Primary composite: intraoperative and postoperative events 6 months after implantation | St. Jude Medical/Abbott |
| Corbisiero et al. (2016) | Retrospective, single-centre study | 125 CRT-D patients (69 QP, 56 BP LV lead) | 69 ± 10 | 23 ± 7 | Hospitalization (inpatient, outpatient, emergency room) | St. Jude Medical/Abbott |
| Erath et al. (2019) | Retrospective, bicentric study | 536 CRT-D patients (123 QP, 413 BP LV lead) | 69 ± 11 | 39 ± 31 | Clinical response to CRT (NYHA, LVEF, LVEDD), mortality, implantation duration, fluoroscopy time | Biotronik, Boston Scientific, Medtronic, St. Jude Medical/Abbott |
| Forleo et al. (2015) | Prospective, multi-centre study | 418 CRT-D patients (230 QP, 188 BP LV lead) | 70 ± 9 | 39 | LV lead failure, successful LV lead implant, fluroroscopy time, lead performance, lead-related complications | St. Jude Medical/Abbott |
| Leshem et al. (2018) | Prospective, multi-centre registry | 2913 CRT-D patients (1940 QP, 973 BP LV lead) | 68 ± 11 | 72 | Primary: HF hospitalizationSecondary: all-cause mortality, HF mortality, cardiac mortality, need for additional procedure, first appropriate and inappropriate therapy | n/a |
| Rijal et al. (2017) | Retrospective, single-centre study | 1441 CRT-D/-P patients (292 QP, 1149 BP LV lead) | 72 ± 12 | 20 ± 16 |
| St. Jude Medical/Abbott, Medtronic |
| Turakhia et al. (2016) | Retrospective, nationwide registry data | 23 570 CRT-D patients (18 406 QP, 5164 BP LV lead) | 70 ± 11 | 14 |
| St. Jude Medical/Abbott |
| Yang et al. (2018) | Retrospective, single-centre study | 516 CRT-D patients (238 QP, 278 BP LV lead) | 69.8 ± 12.6 | 36 | Mortality, CRT-response (NYHA, LVEF), successful LV lead implant, PNS, LV lead dislodgement, PNS | St. Jude Medical/Abbott, Medtronic |
| Study (year of publication) . | Type of study . | No. of patients included . | Mean age (years) . | Follow-up duration (months) . | Study endpoints . | Manufacturer of QP lead . |
|---|---|---|---|---|---|---|
| Arias et al. (2012) | Retrospective, single-centre study | 42 CRT-D patients (21 QP, 21 BP LV lead) | 66 ± 10 | 9 | Successful LV lead implant, lead failure, mortality, hospitalization | St. Jude Medical/Abbott |
| Behar et al. (2015) | Prospective, multi-centre study | 721 CRT-D patients (357 QP, 364 BP LV lead) | 69 ± 10 | 29 ± 1 | Successful LV lead implant, PNS, lead failure, lead revision, mortality | Boston Scientific, Medtronic, St. Jude Medical/Abbott |
| Behar et al. (2017) | Prospective, multi-centre study | 606 CRT-D patients (319 QP, 287 BP LV lead) | 69 ± 10 | 60 | Hospital readmission (CHF, ACS, arrhythmia, device explantation, lead revision, generator replacement) | St. Jude Medical/Abbott |
| Bencardino et al. (2016) | Prospective, randomized, single-centre study | 43 CRT-D patients (23 QP, 20 BP LV lead) | 69 ± 9 | 3 | Successful LV lead implant, lead failure, PNS, CRT-response (NYHA, LVEF) | St. Jude Medical/Abbott |
| Boriani et al.(MORE-CRT), (2016) | Prospective, randomized-controlled multi-centre study | 1078 CRT-D patients (718 QP, 348 BP LV lead) | 69 ± 10 | 6 | Primary composite: intraoperative and postoperative events 6 months after implantation | St. Jude Medical/Abbott |
| Corbisiero et al. (2016) | Retrospective, single-centre study | 125 CRT-D patients (69 QP, 56 BP LV lead) | 69 ± 10 | 23 ± 7 | Hospitalization (inpatient, outpatient, emergency room) | St. Jude Medical/Abbott |
| Erath et al. (2019) | Retrospective, bicentric study | 536 CRT-D patients (123 QP, 413 BP LV lead) | 69 ± 11 | 39 ± 31 | Clinical response to CRT (NYHA, LVEF, LVEDD), mortality, implantation duration, fluoroscopy time | Biotronik, Boston Scientific, Medtronic, St. Jude Medical/Abbott |
| Forleo et al. (2015) | Prospective, multi-centre study | 418 CRT-D patients (230 QP, 188 BP LV lead) | 70 ± 9 | 39 | LV lead failure, successful LV lead implant, fluroroscopy time, lead performance, lead-related complications | St. Jude Medical/Abbott |
| Leshem et al. (2018) | Prospective, multi-centre registry | 2913 CRT-D patients (1940 QP, 973 BP LV lead) | 68 ± 11 | 72 | Primary: HF hospitalizationSecondary: all-cause mortality, HF mortality, cardiac mortality, need for additional procedure, first appropriate and inappropriate therapy | n/a |
| Rijal et al. (2017) | Retrospective, single-centre study | 1441 CRT-D/-P patients (292 QP, 1149 BP LV lead) | 72 ± 12 | 20 ± 16 |
| St. Jude Medical/Abbott, Medtronic |
| Turakhia et al. (2016) | Retrospective, nationwide registry data | 23 570 CRT-D patients (18 406 QP, 5164 BP LV lead) | 70 ± 11 | 14 |
| St. Jude Medical/Abbott |
| Yang et al. (2018) | Retrospective, single-centre study | 516 CRT-D patients (238 QP, 278 BP LV lead) | 69.8 ± 12.6 | 36 | Mortality, CRT-response (NYHA, LVEF), successful LV lead implant, PNS, LV lead dislodgement, PNS | St. Jude Medical/Abbott, Medtronic |
ACS, acute coronary syndrome; BP, bipolar; CHF, congestive heart failure; CRT, cardiac resychronization therapy; CRT-D, cardiac resychronization therapy defibrillator; CRT-P, cardiac resychronization therapy pacemaker; HF, heart failure; LV, left ventricular; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; PNS, phrenic nerve stimulation; QP, quadripolar.
| Study (year of publication) . | Type of study . | No. of patients included . | Mean age (years) . | Follow-up duration (months) . | Study endpoints . | Manufacturer of QP lead . |
|---|---|---|---|---|---|---|
| Arias et al. (2012) | Retrospective, single-centre study | 42 CRT-D patients (21 QP, 21 BP LV lead) | 66 ± 10 | 9 | Successful LV lead implant, lead failure, mortality, hospitalization | St. Jude Medical/Abbott |
| Behar et al. (2015) | Prospective, multi-centre study | 721 CRT-D patients (357 QP, 364 BP LV lead) | 69 ± 10 | 29 ± 1 | Successful LV lead implant, PNS, lead failure, lead revision, mortality | Boston Scientific, Medtronic, St. Jude Medical/Abbott |
| Behar et al. (2017) | Prospective, multi-centre study | 606 CRT-D patients (319 QP, 287 BP LV lead) | 69 ± 10 | 60 | Hospital readmission (CHF, ACS, arrhythmia, device explantation, lead revision, generator replacement) | St. Jude Medical/Abbott |
| Bencardino et al. (2016) | Prospective, randomized, single-centre study | 43 CRT-D patients (23 QP, 20 BP LV lead) | 69 ± 9 | 3 | Successful LV lead implant, lead failure, PNS, CRT-response (NYHA, LVEF) | St. Jude Medical/Abbott |
| Boriani et al.(MORE-CRT), (2016) | Prospective, randomized-controlled multi-centre study | 1078 CRT-D patients (718 QP, 348 BP LV lead) | 69 ± 10 | 6 | Primary composite: intraoperative and postoperative events 6 months after implantation | St. Jude Medical/Abbott |
| Corbisiero et al. (2016) | Retrospective, single-centre study | 125 CRT-D patients (69 QP, 56 BP LV lead) | 69 ± 10 | 23 ± 7 | Hospitalization (inpatient, outpatient, emergency room) | St. Jude Medical/Abbott |
| Erath et al. (2019) | Retrospective, bicentric study | 536 CRT-D patients (123 QP, 413 BP LV lead) | 69 ± 11 | 39 ± 31 | Clinical response to CRT (NYHA, LVEF, LVEDD), mortality, implantation duration, fluoroscopy time | Biotronik, Boston Scientific, Medtronic, St. Jude Medical/Abbott |
| Forleo et al. (2015) | Prospective, multi-centre study | 418 CRT-D patients (230 QP, 188 BP LV lead) | 70 ± 9 | 39 | LV lead failure, successful LV lead implant, fluroroscopy time, lead performance, lead-related complications | St. Jude Medical/Abbott |
| Leshem et al. (2018) | Prospective, multi-centre registry | 2913 CRT-D patients (1940 QP, 973 BP LV lead) | 68 ± 11 | 72 | Primary: HF hospitalizationSecondary: all-cause mortality, HF mortality, cardiac mortality, need for additional procedure, first appropriate and inappropriate therapy | n/a |
| Rijal et al. (2017) | Retrospective, single-centre study | 1441 CRT-D/-P patients (292 QP, 1149 BP LV lead) | 72 ± 12 | 20 ± 16 |
| St. Jude Medical/Abbott, Medtronic |
| Turakhia et al. (2016) | Retrospective, nationwide registry data | 23 570 CRT-D patients (18 406 QP, 5164 BP LV lead) | 70 ± 11 | 14 |
| St. Jude Medical/Abbott |
| Yang et al. (2018) | Retrospective, single-centre study | 516 CRT-D patients (238 QP, 278 BP LV lead) | 69.8 ± 12.6 | 36 | Mortality, CRT-response (NYHA, LVEF), successful LV lead implant, PNS, LV lead dislodgement, PNS | St. Jude Medical/Abbott, Medtronic |
| Study (year of publication) . | Type of study . | No. of patients included . | Mean age (years) . | Follow-up duration (months) . | Study endpoints . | Manufacturer of QP lead . |
|---|---|---|---|---|---|---|
| Arias et al. (2012) | Retrospective, single-centre study | 42 CRT-D patients (21 QP, 21 BP LV lead) | 66 ± 10 | 9 | Successful LV lead implant, lead failure, mortality, hospitalization | St. Jude Medical/Abbott |
| Behar et al. (2015) | Prospective, multi-centre study | 721 CRT-D patients (357 QP, 364 BP LV lead) | 69 ± 10 | 29 ± 1 | Successful LV lead implant, PNS, lead failure, lead revision, mortality | Boston Scientific, Medtronic, St. Jude Medical/Abbott |
| Behar et al. (2017) | Prospective, multi-centre study | 606 CRT-D patients (319 QP, 287 BP LV lead) | 69 ± 10 | 60 | Hospital readmission (CHF, ACS, arrhythmia, device explantation, lead revision, generator replacement) | St. Jude Medical/Abbott |
| Bencardino et al. (2016) | Prospective, randomized, single-centre study | 43 CRT-D patients (23 QP, 20 BP LV lead) | 69 ± 9 | 3 | Successful LV lead implant, lead failure, PNS, CRT-response (NYHA, LVEF) | St. Jude Medical/Abbott |
| Boriani et al.(MORE-CRT), (2016) | Prospective, randomized-controlled multi-centre study | 1078 CRT-D patients (718 QP, 348 BP LV lead) | 69 ± 10 | 6 | Primary composite: intraoperative and postoperative events 6 months after implantation | St. Jude Medical/Abbott |
| Corbisiero et al. (2016) | Retrospective, single-centre study | 125 CRT-D patients (69 QP, 56 BP LV lead) | 69 ± 10 | 23 ± 7 | Hospitalization (inpatient, outpatient, emergency room) | St. Jude Medical/Abbott |
| Erath et al. (2019) | Retrospective, bicentric study | 536 CRT-D patients (123 QP, 413 BP LV lead) | 69 ± 11 | 39 ± 31 | Clinical response to CRT (NYHA, LVEF, LVEDD), mortality, implantation duration, fluoroscopy time | Biotronik, Boston Scientific, Medtronic, St. Jude Medical/Abbott |
| Forleo et al. (2015) | Prospective, multi-centre study | 418 CRT-D patients (230 QP, 188 BP LV lead) | 70 ± 9 | 39 | LV lead failure, successful LV lead implant, fluroroscopy time, lead performance, lead-related complications | St. Jude Medical/Abbott |
| Leshem et al. (2018) | Prospective, multi-centre registry | 2913 CRT-D patients (1940 QP, 973 BP LV lead) | 68 ± 11 | 72 | Primary: HF hospitalizationSecondary: all-cause mortality, HF mortality, cardiac mortality, need for additional procedure, first appropriate and inappropriate therapy | n/a |
| Rijal et al. (2017) | Retrospective, single-centre study | 1441 CRT-D/-P patients (292 QP, 1149 BP LV lead) | 72 ± 12 | 20 ± 16 |
| St. Jude Medical/Abbott, Medtronic |
| Turakhia et al. (2016) | Retrospective, nationwide registry data | 23 570 CRT-D patients (18 406 QP, 5164 BP LV lead) | 70 ± 11 | 14 |
| St. Jude Medical/Abbott |
| Yang et al. (2018) | Retrospective, single-centre study | 516 CRT-D patients (238 QP, 278 BP LV lead) | 69.8 ± 12.6 | 36 | Mortality, CRT-response (NYHA, LVEF), successful LV lead implant, PNS, LV lead dislodgement, PNS | St. Jude Medical/Abbott, Medtronic |
ACS, acute coronary syndrome; BP, bipolar; CHF, congestive heart failure; CRT, cardiac resychronization therapy; CRT-D, cardiac resychronization therapy defibrillator; CRT-P, cardiac resychronization therapy pacemaker; HF, heart failure; LV, left ventricular; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; PNS, phrenic nerve stimulation; QP, quadripolar.
The present meta-analysis comprises 31 403 patients of whom 22 429 patients received QP and 8974 patients BP LV leads. Patients were followed between 3 and 72 months (average observation period median 24 months) in the individual studies.
Survival
Crude mortality rates were available in eight studies.6,7,9–12,16,17 In these studies, comprising 28 262 patients, use of QP leads (20 354 patients) was associated with better survival compared to patients with BP LV leads (7908 patients) (OR 0.61, 95% CI 0.50–0.76; P < 0.01; Q = 11.7; I2 = 40.0%; Figure 1A). This result was confirmed in a sensitivity analysis utilizing the one-study-out method showing that the effect size was not driven by the results of a single study (Supplementary material online, Table S1). According to the rank correlation test of Begg and Mazumdar (t = −0.04, P = 0.9) and the Duval and Tweedie’s trim and fill input method there was no sign of publication bias (Supplementary material online, Figure S2).
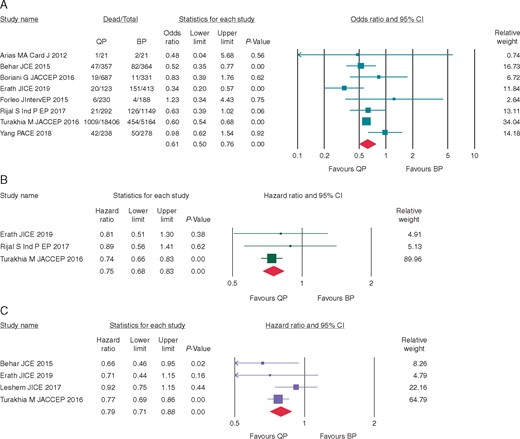
(A) Risk for all-cause mortality (MH odds ratio) in patients with QP vs. BP LV leads. (B) Risk of all-cause mortality (hazard ratio, unadjusted) in patients with QP vs. BP LV leads. (C) Risk of all-cause mortality (hazard ratio, adjusted) in patients with QP vs. BP LV leads. BP, bipolar; CI, confidence interval; LV, left ventricular; Qp, quadripolar.
Unadjusted and adjusted HRs for mortality were available in three10,11,17 and four studies,7,10,14,17 respectively. Pooled analyses of the unadjusted HRs demonstrated better survival among patients implanted with QP LV leads (HR = 0.75; 95% CI 0.68–0.83; P < 0.01; Q = 3.3; I2 = 8.6%; Begg and Mazumdar t < 0.01; P = 1.00) (Figure 1B). Pooled analyses of studies with adjusted HRs revealed similar findings (adjusted HR = 0.79; 95% CI 0.71–0.88; P < 0.01; Q = 3.2; I2 = 7.5%; Begg and Mazumdar t < 0.01; P = 1.00) (Figure 1C).
Improvement of New York Heart Association class and hospitalization
Clinical improvement by at least one NYHA functional class was defined as response to CRT in four studies.6,9,13,17 Among 1315 patients, 643 patients with QP and 672 patients with BP LV leads, more patients fitted with QP leads responded to CRT (OR = 0.59, 95% CI 0.34–1.01; P = 0.05; Q = 6.8; I2 = 55.8%) (Figure 2) without signs of publication bias (Begg and Mazumdar t = −0.50; P = 0.31) (Supplementary material online, Figure S3).
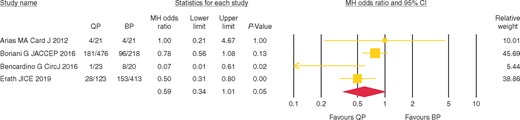
Comparison of improvement of NYHA class in patients with QP vs. BP LV leads. BP, bipolar; CI, confidence interval; LV, left ventricular; NYHA, New York Heart Association; Qp, quadripolar.
Hospitalization rates were examined in three studies9,11,15 comprising 2172 patients. The relative risk for hospitalization after CRT implantation was lower in patients implanted with QP compared to patients with BP LV leads (OR = 0.67, 95% CI 0.55–0.83; P < 0.01; Q = 2.1; I2 = 4.3%; Figure 3). There were no signs of publication bias (Begg and Mazumdar t = 0; P = 1.00) (Supplementary material online, Figure S4).
Risk of hospitalization after CRT implantation in patients with QP vs. BP LV leads. BP, bipolar; CRT, cardiac resychronization therapy; LV, left ventricular; PNS, phrenic nerve stimulation; Qp, quadripolar.
Lead performance
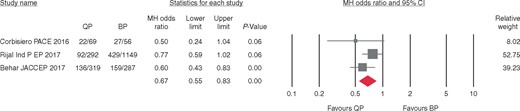
Lead malfunctions defined as LV lead failure resulting in lead deactivation were reported in four studies (13 922 patients, 9764 patients with QP and 4158 with BP LV leads).7,10,11,17 More patients with BP LV leads experienced a deactivation of the LV lead compared to patients with QP leads (OR 0.57, 95% CI 0.34–0.98; P = 0.04; Q = 3.6; I2 = 15.6%; Figure 4A) without any sign of publication bias (Begg and Mazumdar t = −0.5; P = 0.3) (Supplementary material online, Figure S5A). Dislodgement of LV leads requiring lead replacement/repositioning was reported in seven studies6,8–10,12,14,16 with 29 198 patients (21 879 patients with QP and 7319 patients with BP LV leads). The relative risk for repeated surgery to replace/reposition the LV lead was 52% lower among patients with QP leads compared to patients with BP leads (OR 0.48, 95% CI 0.31–0.75; P < 0.01; Q = 19.4; I2 = 69.0%; Figure 4B). According to the rank correlation test of Begg and Mazumdar (t = −0.1; P = 0.76), there was no sign of publication bias, however the Duval and Tweedie’s trim and fill input method indicated some residual publication bias for this endpoint (Supplementary material online, Figure S5B).
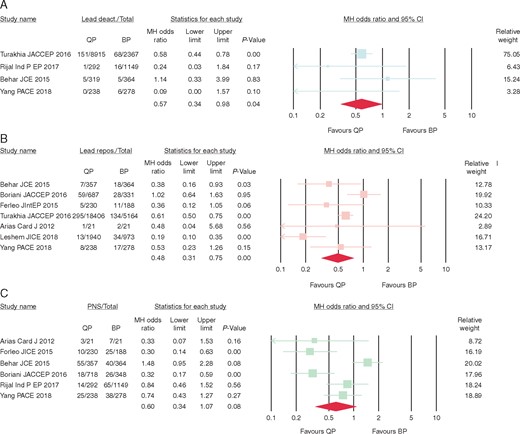
(A) Risk of lead failure resulting in lead deactivation. (B) Risk of lead dislodgement requiring surgical lead replacement/repositioning. (C) Risk of phrenic nerve stimulation requiring lead reprogramming or surgical lead repositioning. BP, bipolar; CI, confidence interval; Qp, quadripolar.
Analysing the results of six studies on the incidence of PNS requiring lead reprogramming or surgical repositioning (4204 patients),6,7,9,11,12,16 a trend for better performance of the QP leads between the two patients groups was observed (OR = 0.60; 95% CI 0.34–1.07; P = 0.08; Q = 23.6; I2 = 78.8%) (Figure 4C) without any signs of publication bias (Begg and Mazumdar t = −0.40; P = 0.26) (Supplementary material online, Figure S5C).
Fluoroscopy times
A total of four studies reported fluoroscopy times in 2062 patients (QP LV leads: 1092 patients; BP LV leads: 970 patients).6,9,12,17 Fluoroscopy duration was on average 4.3 min less (95% CI −8.02 to −0.51; P = 0.03) in patients fitted with QP LV leads compared to those with BP LV leads (Supplementary material online, Figure S6).
Discussion
Main findings
This meta-analysis on the clinical performance of QP LV leads compared to BP leads comprises over 31 000 patients and is, to the best of our knowledge, the largest one at present. Analysing 12 studies, distinct benefits of QP LV leads in CRT patients including improved post-procedural LV lead performance, shorter fluoroscopy times, less PNS, and higher CRT response rates compared to BP LV leads. Of particular note, implantation of QP LV leads was associated with significantly better pooled survival rates.
Clinical efficacy of quadripolar left ventricular leads
This meta-analysis confirms findings of a nationwide American registry10 comprising more than 18 000 patients receiving QP LV leads. The authors found a lower mortality rate among patients with QP leads compared to subjects with BP leads (5.04 deaths vs. 6.45 deaths per 100 patient-years; P < 0.01). After adjustment for confounding baseline variables, the QP lead remained significantly associated with reduced risk of death (HR 0.77, 95% CI 0.69–0.86; P < 0.01). In contrast, the MORE-CRT Trial, randomizing 1018 patients in a 2:1 fashion either to QP or BP CRT systems, showed no difference in all-cause mortality (P = 0.59).9 One explanation for this discrepancy might be the short follow-up duration of only 6 months in the latter study.9 In the study by Turakhia et al., the unadjusted Kaplan–Meier survival curves separate between 90 and 120 days after CRT implantation.10 This hypothesis is also supported by the long follow-up duration of 5 years of a UK prospective multi-centre trial analysing 721 CRT-D patients (357 implanted with QP and 364 implanted with BP LV leads).7 Behar et al. found a relative mortality risk reduction of 36% in patients implanted with QP LV leads. Another factor positively impacting on survival might be response to CRT. Most of the studies analysed in this meta-analysis report data on clinical improvement measured in NYHA functional class revealing a strong trend towards a higher NYHA response rate after CRT implantation using QP LV leads. Consequently, patients with QP LV leads had a significantly lower pooled relative risk ratio for hospitalization by 33% in the present analysis.
Safety of quadripolar left ventricular leads
Avoiding lead malfunctions necessitating repeated surgery is of paramount importance in CRT recipients.18,19 In a large registry, Poole et al.19 prospectively analysed data of patients undergoing replacement of a pacemaker or defibrillator generator with or without additional implant of leads over a 6-months follow-up period. Complications were highest in patients undergoing upgrade or revision of a CRT system (18.7%, 95% CI 15.1–22.6).19 The present meta-analysis indicates superiority of QP over BP LV leads regarding LV dislodgement requiring surgical lead replacement or repositioning. Similarly, there was less LV lead deactivation associated with subjects with QP leads.
Phrenic nerve stimulation is a known common adverse device effect in CRT patients.20 In the above-mentioned MORE-CRT trial, the proportion of patients with rejected lead positions due to PNS was significantly lower in the QP LV lead group than in the BP LV lead group (2.5% vs. 8.8%, P < 0.0001). Furthermore, the overall average safety margin was significantly higher in the QP LV lead group than in the BP LV lead group (4.5 ± 3.3 V vs. 1.9 ± 3.2 V, P = 0.03).9 The present meta-analysis found a trend towards less PNS among patients with QP LV leads (P = 0.08). These factors might explain the significantly shorter fluoroscopy times in patients implanted with QP LV leads of about 4 min.
Limitations
This meta-analysis is subject to all potential limitations of this kind of analysis. We did not have access to individual patient data from all studies reviewed and had to rely on published information. Secondly, not all the identified studies used statistical adjustments to correct for potential confounding, hence residual confounding cannot be excluded. However, the large number of data sets obtained in more than 31 000 patients and the internal consistency of findings emphasize the validity of this meta-analysis. Moreover, data on clinical response and hospitalizations should be considered with caution as they are based on a small number of heterogeneous studies. Operator skill and experience has improved the results of cardiac resynchronization therapy concurrently with the uptick of QP leads, which might also lead to the better performance of these leads. Finally, from the total of 31 403 patients one retrospective registry10 contributed 23 570 patients, thus potentially dominating the results of the meta-analysis. However, the results for crude survival (i.e. one-study-out method), improvement of NYHA class, hospitalization, and PNS demonstrated significant benefits for QP leads over BP leads even without the inclusion of the study by Turakhia et al.10
Conclusions
This meta-analysis suggests distinct benefits of QP over BP leads in patients undergoing CRT.
Conflict of interest: J.W.E. reports receiving consulting fees, travel support and lecture fees from Zoll Medical, travel grants from St. Jude Medical/Abbott and lecture fees from Servier and was a fellow of the Boston Scientific heart rhythm fellowship program, outside the submitted work. A.P.B. reports receiving travel support to attend a scientific meeting from SJM. S.H.H. reports consulting fees Bayer, BI, Boston Scientific, BMS, Gilead, J&J, Medtronic, Pfizer, SJM, Sanofi-Aventis, Zoll Medical and Cardiome, outside the submitted work. M.V. reports lecture/consulting fees from Bayer, BMS, Daiichi-Sankyo, Pfizer and Spectranetics and support attending scientific meetings from Bayer, Daiichi-Sankyo, Egis, Pfizer, and SJM, outside the submitted work.
References
Author notes
Stefan H. Hohnloser and Mate Vamos authors contributed equally as last authors.



