-
PDF
- Split View
-
Views
-
Cite
Cite
Antonio Hernández-Madrid, Mélèze Hocini, Jian Chen, Tatjana Potpara, Laurent Pison, Carina Blomström-Lundqvist, conducted by the Scientific Initiative Committee, European Heart Rhythm Association, How are arrhythmias managed in the paediatric population in Europe? Results of the European Heart Rhythm survey, EP Europace, Volume 16, Issue 12, December 2014, Pages 1852–1856, https://doi.org/10.1093/europace/euu313
Close - Share Icon Share
Abstract
The aim of this survey was to provide insight into current practice regarding the management of paediatric arrhythmias in Europe. The survey was based on a questionnaire sent via the Internet to the European Heart Rhythm Association (EHRA) electrophysiology research network centres. The following topics were explored: patient and treatment selection, techniques and equipment, treatment outcomes and complications. The vast majority of paediatric arrhythmias concerns children older than 1 year and patients with grown-up congenital heart disease. In 65% of the hospitals there is a specialized paediatric centre, and the most commonly observed arrhythmias include Wolff-Parkinson-White syndrome and atrioventricular nodal re-entry tachycardias (90.24%). The medical staff performing paediatric catheter ablations in Europe are mainly adult electrophysiology teams (82.05% of the centres). Radiofrequency is the preferred energy source used for paediatric arrhythmia ablation. Catheter ablation is only chosen if two or more antiarrhythmic drugs have failed (94.59% of the centres). The majority of the centres use flecainide (37.8%) or atenolol (32.4%) as their first choice drug for prevention of recurrent supraventricular arrhythmias. While none of the centres performed catheter ablation in asymptomatic infants with pre-excitation, 29.7% recommend ablation in asymptomatic children and adolescents. The preferred choice for pacemaker leads in infants less than 1 year old is implantation of epicardial leads in 97.3% of the centres, which continues to be the routine even in patients between 1 and 5 years of age as reported by 75.68% of the hospitals. Almost all centres (94.59%) report equally small number of complications of catheter ablation in children (aged 1–14 years) as observed in adults.
Introduction
Management of paediatric arrhythmias is always challenging. In children without structural heart disease, most arrhythmia mechanisms are typically the same as in adults. However, some arrhythmias are specific to younger age or associated with a particular congenital heart disease. The different characteristics of cardiac arrhythmias in children, the lower body weight, and a more frequent presence of congenital heart disease make the management of arrhythmias in this population different from that in adults.1,2
Radiofrequency catheter ablation is increasingly being performed in children. Even at the younger age, catheter ablation can be performed with high success rates, provided that it is performed by an experienced, usually multidisciplinary team.1
This European Heart Rhythm Association (EHRA) survey intended to explore the treatment approaches adopted for paediatric arrhythmias, including the selection of children and equipment used, the use of antiarrhythmic drugs that require different precautions compared with adults, and the implantation preferences regarding pacemakers, and complications of the procedures.
Methods and results
Participating centres
This survey is based on a questionnaire sent via the Internet to the EHRA electrophysiology (EP) research network centres. Responses were received from 42 centres spanning a wide geographical area. The majority of the responding centres performed a high volume of invasive procedures. In the last calendar year, 66.7% of the centres performed 200 or more catheter ablation procedures, and 19.05% performed 100–199 procedures. The number of implantations including new implants and replacements was more than 400 in 46.3% of the centres. Two-thirds of the centres (66.7%) carried out more than 100 implantable cardioverter defibrillators (ICDs) procedures per year, and 82.42% annually implanted more than 200 pacemakers. The majority of the centres (80.95%) were university hospitals, 11.9% were private hospitals, and the rest were other types of hospitals.
Patient selection
Almost all the responding centres (93%) regularly perform paediatric interventions, including device implants and catheter ablations, and there is a specialized paediatric centre in 65% of the hospitals. Catheter ablation was very rarely performed in children under 1 year of age, representing only a small proportion (<5%) of the ablation procedures in almost all the centres (96.88%). Most interventions were performed in children older than 1 year and in patients with adult congenital heart disease (independent of patient age).
More than 90% of the centres perform catheter ablation for Wolf-Parkinson-White (WPW) syndrome and atrioventricular (AV) nodal re-entry tachycardias, and almost two-thirds perform ablation of the arrhythmias associated with congenital heart disease, atrial fibrillation or ventricular arrhythmias.
Only 2.44% of the centres routinely use genetic testing in all paediatric cardiac arrhythmias, and 58.54% always use it for channelopathies or suspected genetic disease. One-third of the centres (34.15%) use genetic testing sometimes and 4.88% do not use because it is not available.
Techniques and equipment
Catheter ablation of paediatric arrhythmias was exclusively performed by paediatric electrophysiologists in only 2.56% of the centres, while EP teams were multidisciplinary in 15.36% of hospitals or the same teams performed ablations both in children and adult patients (82.05%). Catheter ablation in children is always challenging because of the need for deep sedation or general anaesthesia during the procedure in order to avoid pain and discomfort for the patient. Most of the centres (71.79%) always use general anaesthesia in children under 14 years of age.
The number of catheters used for ablation directly correlates with the weight of the patient. Most hospitals use two catheters for ablation procedures (even if the patient's body weight is less than 10 kg) and almost half the centres use three catheters for children weighing more than 20 kg. The use of small 5 French catheters for ablation is not widely adopted, thus being used by only 56.4% of the centres. The preferred technique for the left accessory pathway ablation is retrograde transaortic approach in two-thirds of the hospitals (64.10%), while the remaining centres use the ransseptal technique for ablation.
Radiofrequency energy is most commonly used for catheter ablation of paediatric arrhythmias. Regarding other energy sources, one-third of the centres (35.9%) use cryoablation only for the ablation of AV nodal/perinodal substrate, 23.1% never use cryoablation and in 17.95% of the centers it is not available at all. Cryoenergy is used after failed radiofrequency catheter ablation in only 5.13% of the centers. A total of 23.08% of the centres use electroanatomical mapping to guide ablation in the majority of cases, while one-third (30.77%) use mapping only for complex substrates.
Treatment selection and outcome
Acute management
If vagal manoeuvres fail to stop a neonatal supraventricular tachycardia, intravenous (i.v.) propranolol is used in almost half the hospitals, while others use amiodarone (21.6%) or flecainide (18.9%) as the first choice drug. If the combination of several drugs does not eliminate neonatal tachycardia, but tachycardia causes cardiomyopathy, the treatment of choice is catheter ablation in 59.46%, followed by drug therapy at incremental doses in 24.32% of the centres.
For the acute management of supraventricular tachycardia in schoolchildren, when vagal manoeuvres fail, the first-line drug preferred by the majority of the centres is i.v. adenosine (64.86%), followed by i.v. propranolol (16.22%) or verapamil (8.11%), while i.v. flecainide, propafenone, or amiodarone is the last resort.
The first-line treatment option for acute management of wide QRS tachycardias in infants and children is electrical cardioversion in almost half the centres, followed by i.v. amiodarone in 27% of the centres.
Prophylactic therapy
Most of the centres use flecainide (37.8%) or atenolol (32.4%) as the drug of choice for prevention of recurrent supraventricular arrhythmias if ablation is not preferred or advised. None of the centres reported using digoxin for this purpose.
For patients under 5 years of age, the most common clinical approach is non-invasive, selecting antiarrhythmic drugs as the first choice in recurrent arrhythmias despite the failure of one antiarrhythmic drug (63.89%). Catheter ablation is only used for recurrent arrhythmias if two or more antiarrhythmic drugs fail as reported by (94.59% of the centres. All the centres perform catheter ablation when tachycardiomyopathy is present or suspected (Figure 1).
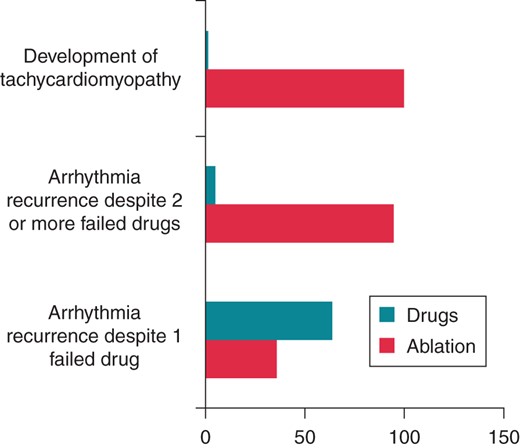
Selection of treatment with catheter ablation or antiarrhythmic drugs for the management of supraventricular tachycardia in children under 5 years.
Regarding the management of asymptomatic pre-excitation in different age groups, none of the centres performs catheter ablation in infants, but 29.7% of the centres perform ablation in children and adolescents. Almost all the respondents perform catheter ablation if the patient wishes to participate in competitive sport or is at increased risk of sudden death (Figure 2).
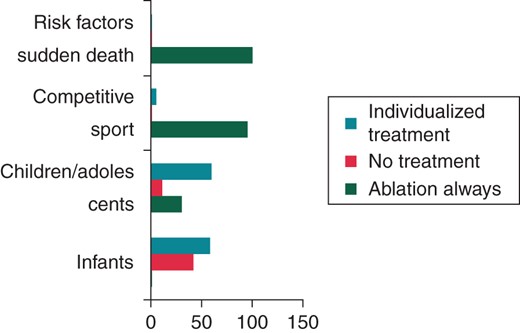
Clinical approaches to the management of asymptomatic pre-excitation in different groups.
The preferred treatment for infants with episodes of orthodromic reentrant tachycardia and WPW syndrome is antiarrhythmic drug therapy, such as β-blockers (32.4%) or flecainide (37.8%), while catheter ablation is selected as first choice by only in 13.51% of the hospitals. Most centres (91.89%) prefer antiarrhythmic drugs, or no treatment if possible, for a narrow QRS tachycardia in children under 5 years. Some (21.62%) centres use the same approach for very infrequent or the first episode of narrow QRS tachycardia.
Exploring the choice of leads for cardiac pacing in infants under 1 year, 97.3% of the centres implant epicardial leads. The majority of the hospitals (75.68%) implant epicardial leads in patients between 1 and 5 years of age. Even in patients with congenital heart disease and no venous access to the right ventricle, the preferred site is epicardial in 86.1% of the hospitals. Most centres (80.56%) are now implanting left ventricular leads in children not only for cardiac resynchronization therapy for heart failure (72.2%), but also for congenital heart disease without access to the right ventricle and the need for pacing. In patients with congenital AV block, 27% of the centres implant a left ventricular lead for pacing. Although 40.5% of the centres implant subcutaneous cardiac defibrillators in adults, only 5.56% have used it in children.
In the last decades, radiofrequency catheter ablation is progressively used as curative therapy for tachyarrhythmias in children, with as excellent results as in adults. Almost all centres (94.59%) report the same rate of complications of catheter ablation in children as in adults.
Discussion
Patient selection
To achieve high quality of care in the management of paediatric arrhythmias in all age groups, a specific paediatric centre with skilled and trained physicians and personnel is necessary.3 Surgical procedures for correction of congenital heart disease with the formation of myocardial scar tissue can create almost any kind of macro-reentrant circuits. Further understanding of complex anatomy and variations in surgical and interventional procedures, resulting in a variety of complex arrhythmias, is particularly challenging for the electrophysiologists, and puts emphasis on the role of specific paediatric centres and collaborations with paediatric cardiologists and arrhythmologists. Even though some genetic diseases are associated with high mortality in the early years,4–6 the proportion of centres that would use genetic screening for channelopathies or suspected genetic disease was relatively low at 59%.
Techniques and equipment
Catheter ablation in small children may require specific modifications to reduce risk of complications. The adult electrophysiology team are the medical staff performing catheter ablation for paediatric arrhythmias in Europe, and most of the centres always use general anaesthesia in children. In infants and young children, modifications may include downsizing to 5F ablation catheters and limiting the number to a single diagnostic catheter for both atria and ventricular pacing and recording. The numbers of catheters used for ablation correlates directly with the weight of the patient.7
Radiofrequency is the most frequently used energy for ablation of paediatric arrhythmias. Cryoablation is emerging in the paediatric population as an alternative technique for arrhythmias near the AV node,8 but is less suitable in infants because of the relatively large size and stiffness of the catheter.9 The use of the non-fluoroscopic navigation systems allows for significant reduction of fluoroscopy for complex substrates.10
Treatment selection and results
Acute management
In infants and children, a clear diagnosis with electrocardiographic documentation of the arrhythmia is required before the prescription of any antiarrhythmic drug. A 12 lead electrocardiogram must thus be obtained prior to therapy. The recommendation for acute termination of narrow complex tachycardias in a stable patient is vagal manoeuvres, which are effective in a considerable proportion of patients, prior to the administration of antiarrhythmic drugs. In case of failure, intravenous adenosine is the drug of choice. It was therefore surprising that only 65% of the respondents used i.v. adenosine and as many as one-quarter used i.v. propranolol or verapamil. Verapamil may be given in older children but is contra-indicated in infants, as it has been described that this may lead to cardiovascular collapse.11 It was also surprising that i.v. amiodarone was used in almost one-third of children with wide QRS tachycardias.
Prophylactic therapy
The sole complaint of palpitations or other symptoms is not a sufficient reason to give antiarrhythmic drugs. Long-term treatment has to take into account that the majority of young patients may have only a few episodes of tachycardia, and invasive therapy is thus limited to patients with drug-refractory or life-threatening arrhythmias.
In patients with supraventricular tachycardia that continues to recur after 1 year of age or those with the first manifestation after infancy, the management strategy has to be individualized for the patients according to the severity of symptoms and frequency of episodes. No treatment is probably warranted in case of rare and short events that are well tolerated, the absence of pre-excitation, and a structurally normal heart. In children older than 5 years, with a long-lasting history of episodes, invasive curative treatment may be preferred over long-term prophylactic antiarrhythmic medication, given the safety and efficacy of ablation in the current era.
The optimal management of patients with asymptomatic WPW syndrome is still controversial, which was evident in this European survey, with some physicians aiming at the conservative approach and others advocating the early ablation approach, thus demonstrating diverse management routines for this patient population.12 Recent studies, however, have reported that no differences in atrial vulnerability and parameters associated with risk of sudden cardiac death (including the shortest pre-excited RR interval) between asymptomatic and symptomatic patients, and that prognosis of WPW syndrome essentially depends on the intrinsic electrophysiological properties of an accessory pathway rather than on symptoms, and ablation is of benefit in improving the long-term outcome.13,14
The generator size has diminished and pacing leads have become progressively thinner. These developments have made using cardiac pacing in children easier although no dedicated paediatric pacing systems exist. The majority of the hospitals usually implant epicardial leads in patients between 1 and 5 years of age. The longevity of modern steroid eluting epicardial leads is good and can be considered almost equivalent to that of endocardial pacing leads. This is in accordance with the present guidelines that advised epicardial implants for infants <10 kg, and endocardial systems only in specific situations (failed epicardial implant, centre preference) and in children >20 kg.15–17
In young patients, cardiac resynchronization device implantation may be technically challenging because of inaccessibility of the ventricular free wall through a transvenous route due to either small vessel size or abnormal cardiac anatomy. Despite a much more heterogeneous structural and functional substrate, limited evidence has so far shown similar effects of resynchronization therapy in children as in adults.18 Many centres have reported implanting left ventricular leads for congenital heart disease without access to right ventricle and in patients with congenital AV block.19
A ‘leadless’ ICD is now available that has the generator placed subcutaneously in the left anterior chest together with a parasternal subcutaneous lead that allows both defibrillation and back up post-shock pacing. The current system is suitable for adults and children over 40 kg only.20 This fact explains why although a significant proportion of the centres have used the subcutaneous defibrillator in adults, only 5.56% have used it in children.
Small patient size has been reported to be associated with a higher rate of major complications after radiofrequency ablation compared with older children. This is in contrast to the studies revealing no differences concerning success and major complications between infants (<18 months), non-infants, and adults.21–23 Data from the Paediatric Radiofrequency Ablation Registry and the study for Prospective Assessment after Paediatric Cardiac Ablation reported a complication rate ranging from 3% to 4.2%.22 Prolonged radiation exposure is of particular concern in children. In this survey, almost all the centres reported no excess in complications of catheter ablation in children compared with adults. As this is not a survey recording the prospective individual patient data, one cannot exclude underreporting of complications.
Conclusions
In 65% of the hospitals there is a specific paediatric centre. The adult electrophysiology team are the medical staff performing catheter ablation for paediatric arrhythmias in Europe. Radiofrequency is preferred energy for ablation of paediatric arrhythmias. The complication rates of ablation in children are not increased compared with the results in the adult patients.
Acknowledgements
The production of this EP wire document is under the responsibility of the Scientific Initiative Committee of the European Heart Rhythm Association: Carina Blomström-Lundqvist (chairman), Maria Grazia Bongiorni (co-chair), Jian Chen, Nikolaos Dagres, Heidi Estner, Antonio Hernandez-Madrid, Melece Hocini, Torben Bjerregaard Larsen, Laurent Pison, Tatjana Potpara, Alessandro Proclemer, Elena Sciraffia, Derick Todd Document reviewer on behalf EP-Europace: Irene Savelieva (St George's University of London, London, UK). The authors acknowledge the EHRA Research Network centres participating in this EP-Wire. A list of the Research Network can be found on the EHRA website.
Conflict of interest: None declared.



