-
PDF
- Split View
-
Views
-
Cite
Cite
Thomas Schroeter, Axel Linke, Martin Haensig, Denis R. Merk, Michael A. Borger, Friedrich W. Mohr, Gerhard Schuler, Predictors of permanent pacemaker implantation after Medtronic CoreValve bioprosthesis implantation, EP Europace, Volume 14, Issue 12, December 2012, Pages 1759–1763, https://doi.org/10.1093/europace/eus191
Close - Share Icon Share
Abstract
High-grade conduction disturbances requiring permanent pacemaker (PPM) implantation occur in up to 40% of patients following transcatheter aortic valve implantation (TAVI). The aim of this study was to identify pre-operative risk factors for PPM implantation after TAVI with the Medtronic CoreValve prosthesis (CVP).
We retrospectively analysed 109 patients following transfemoral CVP implantation performed between 2008 and 2009 at the Leipzig Heart Center. Patients who had indwelling PPM at the time of TAVI (n = 21) were excluded, leaving 88 patients for analysis. Mean age was 80.3 ± 6.6 years and logistic EuroScore predicted risk of mortality was 23.3 ± 12.1%. A total of 32 patients (36%) underwent PPM implantation post-TAVI during the same hospital admission. A total of 27/88 (31%) had evidence of pre-operative abnormal conduction, including first degree AV block and left bundle brunch block. Statistically significant risk factors for the need for post-operative PPM were patient age >75 years [P = 0.02, odds ratio (OR) 4.6], pre-operative heart rate <65 beats per minute (b.p.m.; P = 0.04, OR 2.9), CVP oversizing >4 mm (P = 0.03, OR 2.8), CVP prosthesis >26 mm (OR 2.2), atrial fibrillation (P = 0.001, OR 5.2), and ventricular rate <65 b.p.m. at the first post-operative day (P = 0.137, OR 6.0).
PPM implantation occurs frequently after transfemoral TAVI with the CVP. Older age, chronic atrial fibrillation, pre-operative bradycardia, and larger or significantly oversized prostheses were independent risk factors for PPM implantation following TAVI with the CVP.
Introduction
Transcatheter aortic valve implantation (TAVI) for aortic stenosis (AS) has become an accepted treatment for older patients with severe co-morbidities.1–4 Benefits of this procedure include a minimally invasive approach, and the avoidance of cardiopulmonary bypass and cardioplegic arrest. Furthermore, transfemoral TAVI can be performed without general anaesthesia, intubation, and ventilation. Despite these benefits, a growing clinical experience with TAVI has revealed several intra- and post-procedure complications that can occur. One of these complications is the occurrence of post-operative conduction problems with the requirement for subsequent permanent pacemaker (PPM) implantation. Observed PPM implantation rates post-TAVI range from 4 to 40%,5,6 with generally higher rates observed post-implantation of the CoreValve prosthesis (CVP) (Medtronic, Inc., Minneapolis, MN, USA).
The objective of this study was to determine the predictors of post-operative PPM implantation in a consecutive series of patients undergoing transfemoral CVP implantation.
Methods
Patients
We retrospectively analysed 109 patients who underwent transfemoral implantation of a CVP performed between 2008 and 2009 at the Heart Center Leipzig. Surgical risk of those patients was assessed by the logistic EuroSCORE system (expected mortality >20%) and clinical presentation. Twenty-one of 109 patients had a pre-operative PPM and were therefore excluded, leaving 88 patients for subsequent analysis. Pre-operative measurement of the size of the aortic annulus by transoesophageal echocardiography (TEE) was used to determine the correct size of the valvuloplasty balloon and the necessary prosthesis size. The prosthesis was implanted via the femoral artery in all patients. A balloon valvuloplasty of the stenotic aortic valve was performed under rapid ventricular pacing using a 24 or 26 mm balloon catheter (Osypka AG, Rheinfelden, Germany). The crimped prosthesis was placed under fluoroscopy control in the aortic annulus. Immediately before and after step-wise release of the prosthesis, we performed an angiography to assess the correct position. For closure of the femoral artery access, we used the ProStar device (Abbott Vascular, IL, USA). A temporary transvenous pacemaker was placed through the contralateral femoral vein. After the implantation procedure, the patients were transferred to the intensive care unit. Continuous telemetry was continued for 5 days post-procedure.
We collected echocardiographic and electrocardiographic data pre- and post-operatively on all patients. Annulus diameter measurements were collected from the pre-operative TEE data. Oversizing was considered the difference between the actual implanted valve size and the annular diameter as measured by TEE. Transvalvulars gradients were measured by pre- and post-operative echocardiography, and an invasive pressure gradient was determined in all patients intra-operatively.
Continuous variables are presented as means ± SD; categorical variables are presented as proportions. The Mann–Whitney U test was used to compare continuous variables. A level of P < 0.05 was considered significant. The multivariate analysis was performed according to Cochran–Mantel–Haenszel7,8 test for repeated test of independence. Statistical analysis was performed with SPSS Statistical Software 16.0 (SPSS Inc., Chicago, IL, USA).
Results
Transfemoral CVP implantation was successfully performed in all 109 patients. The peak gradient across the aortic valve decreased from 70.4 ± 23.2 to 17.2 ± 7.1 mmHg and the mean gradient from 46.4 ± 15.3 to 9.7 ± 4.4 mmHg (both P < 0.001).
A total of 32 patients (36.4%) without pre-operative PPM developed high-grade AV block, AVB (26 patients) or bradyarrhythmia (6 patients) necessitating post-CVP PPM implantation. The mean time between TAVI procedure and PPM implantation was 5.2 ± 4.6 days. A total of 55 patients (62.5%) were treated with β-blockers pre-operatively. The proportion of patients receiving pre-operative β-blocker therapy was similar in patients who did and did not require post-operative PPM implantation.
The baseline characteristics of the 88 analysed patients and potential influencing factors for post-operative requirement of PPM are summarized in Table 1. There were no statistically significant differences in age, EuroScore, left ventricular function, or transvalvular pressure gradients between patients who did or did not require a post-operative PPM. Aortic valve area, annulus dimension, interventricular septal dimension, valve size, oversizing of the prosthesis, and re-dilatation rates were also comparable between groups. In addition, the pre-operative electrocardiography (ECG) showed no significant differences in PR duration, QRS duration, frequency of AVB, left, or right bundle brunch block (RBBB) between patients who did or did not require post-operative PPM. The only observed significantly different pre-operative variable was pre-operative ventricular rate [77.4 ± 14.4 vs. 70.8 ± 14.5 beats per minute (b.p.m.); P = 0.034] and sinus rhythm vs. atrial fibrillation (P = 0.006).
Clinical characteristics of 88 patients without a previously implanted pacemaker undergoing transfemoral aortic valve implantation (continuous variables expressed as mean ± standard deviation)
| Variables . | No new PM . | New PM . | P value* . |
|---|---|---|---|
| Number, n (%) | 56 (63.6%) | 32 (36.4%) | |
| Age, year | 79.4 ± 8.0 | 80.7 ± 4.6 | 0.621 |
| Biplane LVEF (%) | 53.5 ± 14.5 | 57.8 ± 12.1 | 0.262 |
| β-Blockers (pre-operative) | 35 (62.5%) | 20 (62.5%) | 0.996 |
| Aortic valve area (cm2) | 0.56 ± 0.15 | 0.59 ± 0.17 | 0.652 |
| Aortic annulus dimension TTE (mm) | 23.2 ± 2.4 | 23.1 ± 2.0 | 0.810 |
| Interventricular septum (mm) | 14.2 ± 2.8 | 14.1 ± 2.4 | 0.769 |
| Peak pressure gradient (mmHg) | 73.6 ± 22.9 | 74.2 ± 24.7 | 0.953 |
| Mean pressure gradient, mmHg | 47.3 ± 14.9 | 49.1 ± 16.4 | 0.861 |
| Coronary heart disease, n (%) | 37 (67.3%) | 17 (53.1%) | 0.252 |
| Intra-operative | |||
| Peak pressure gradient CVP, mmHg | 16.7 ± 8.2 | 18.4 ± 6.1 | 0.148 |
| Mean pressure gradient CVP (mmHg) | 9.5 ± 5.2 | 9.9 ± 3.6 | 0.295 |
| Oversizing (mm) | 3.56 ± 2.02 | 4.19 ± 1.89 | 0.099 |
| Valve size (mm) | 26.6 ± 2.4 | 27.3 ± 2.1 | 0.187 |
| Re-dilation, n (%) | 12 (21.4%) | 7 (21.9%) | 1.000 |
| Valve-in-valve, n (%) | 2 (3.6%) | 1 (3.1%) | 1.000 |
| ECG characteristics | |||
| Ventricular rate | 77.4 ± 14.3 | 70.8 ± 14.5 | 0.034 |
| Sinus rhythm | 44 (78.6%) | 16 (50.0%) | 0.006 |
| Pre-operative atrial fibrillation | 12 (21.4%) | 16 (50.0%) | 0.006 |
| PQ duration (ms) | 182.1 ± 42.7 | 184.7 ± 25.0 | 0.400 |
| QRS duration (ms) | 94.1 ± 24.1 | 94.4 ± 19.7 | 0.714 |
| AV-block, n (%) | 11 (19.7%) | 4 (13.3%) | 0.550 |
| LBBB, n (%) | 5 (8.9%) | 2 (6.5%) | 1.000 |
| RBBB, n (%) | 3 (5.4%) | 3 (9.4%) | 0.664 |
| Variables . | No new PM . | New PM . | P value* . |
|---|---|---|---|
| Number, n (%) | 56 (63.6%) | 32 (36.4%) | |
| Age, year | 79.4 ± 8.0 | 80.7 ± 4.6 | 0.621 |
| Biplane LVEF (%) | 53.5 ± 14.5 | 57.8 ± 12.1 | 0.262 |
| β-Blockers (pre-operative) | 35 (62.5%) | 20 (62.5%) | 0.996 |
| Aortic valve area (cm2) | 0.56 ± 0.15 | 0.59 ± 0.17 | 0.652 |
| Aortic annulus dimension TTE (mm) | 23.2 ± 2.4 | 23.1 ± 2.0 | 0.810 |
| Interventricular septum (mm) | 14.2 ± 2.8 | 14.1 ± 2.4 | 0.769 |
| Peak pressure gradient (mmHg) | 73.6 ± 22.9 | 74.2 ± 24.7 | 0.953 |
| Mean pressure gradient, mmHg | 47.3 ± 14.9 | 49.1 ± 16.4 | 0.861 |
| Coronary heart disease, n (%) | 37 (67.3%) | 17 (53.1%) | 0.252 |
| Intra-operative | |||
| Peak pressure gradient CVP, mmHg | 16.7 ± 8.2 | 18.4 ± 6.1 | 0.148 |
| Mean pressure gradient CVP (mmHg) | 9.5 ± 5.2 | 9.9 ± 3.6 | 0.295 |
| Oversizing (mm) | 3.56 ± 2.02 | 4.19 ± 1.89 | 0.099 |
| Valve size (mm) | 26.6 ± 2.4 | 27.3 ± 2.1 | 0.187 |
| Re-dilation, n (%) | 12 (21.4%) | 7 (21.9%) | 1.000 |
| Valve-in-valve, n (%) | 2 (3.6%) | 1 (3.1%) | 1.000 |
| ECG characteristics | |||
| Ventricular rate | 77.4 ± 14.3 | 70.8 ± 14.5 | 0.034 |
| Sinus rhythm | 44 (78.6%) | 16 (50.0%) | 0.006 |
| Pre-operative atrial fibrillation | 12 (21.4%) | 16 (50.0%) | 0.006 |
| PQ duration (ms) | 182.1 ± 42.7 | 184.7 ± 25.0 | 0.400 |
| QRS duration (ms) | 94.1 ± 24.1 | 94.4 ± 19.7 | 0.714 |
| AV-block, n (%) | 11 (19.7%) | 4 (13.3%) | 0.550 |
| LBBB, n (%) | 5 (8.9%) | 2 (6.5%) | 1.000 |
| RBBB, n (%) | 3 (5.4%) | 3 (9.4%) | 0.664 |
*Mann–Whitney U or Fisher's exact test; LVEF, left ventricular ejection fraction; TTE, transthoracal echocardiography; LBBB, left bundle branch block; RBBB, right bundle branch block.
Clinical characteristics of 88 patients without a previously implanted pacemaker undergoing transfemoral aortic valve implantation (continuous variables expressed as mean ± standard deviation)
| Variables . | No new PM . | New PM . | P value* . |
|---|---|---|---|
| Number, n (%) | 56 (63.6%) | 32 (36.4%) | |
| Age, year | 79.4 ± 8.0 | 80.7 ± 4.6 | 0.621 |
| Biplane LVEF (%) | 53.5 ± 14.5 | 57.8 ± 12.1 | 0.262 |
| β-Blockers (pre-operative) | 35 (62.5%) | 20 (62.5%) | 0.996 |
| Aortic valve area (cm2) | 0.56 ± 0.15 | 0.59 ± 0.17 | 0.652 |
| Aortic annulus dimension TTE (mm) | 23.2 ± 2.4 | 23.1 ± 2.0 | 0.810 |
| Interventricular septum (mm) | 14.2 ± 2.8 | 14.1 ± 2.4 | 0.769 |
| Peak pressure gradient (mmHg) | 73.6 ± 22.9 | 74.2 ± 24.7 | 0.953 |
| Mean pressure gradient, mmHg | 47.3 ± 14.9 | 49.1 ± 16.4 | 0.861 |
| Coronary heart disease, n (%) | 37 (67.3%) | 17 (53.1%) | 0.252 |
| Intra-operative | |||
| Peak pressure gradient CVP, mmHg | 16.7 ± 8.2 | 18.4 ± 6.1 | 0.148 |
| Mean pressure gradient CVP (mmHg) | 9.5 ± 5.2 | 9.9 ± 3.6 | 0.295 |
| Oversizing (mm) | 3.56 ± 2.02 | 4.19 ± 1.89 | 0.099 |
| Valve size (mm) | 26.6 ± 2.4 | 27.3 ± 2.1 | 0.187 |
| Re-dilation, n (%) | 12 (21.4%) | 7 (21.9%) | 1.000 |
| Valve-in-valve, n (%) | 2 (3.6%) | 1 (3.1%) | 1.000 |
| ECG characteristics | |||
| Ventricular rate | 77.4 ± 14.3 | 70.8 ± 14.5 | 0.034 |
| Sinus rhythm | 44 (78.6%) | 16 (50.0%) | 0.006 |
| Pre-operative atrial fibrillation | 12 (21.4%) | 16 (50.0%) | 0.006 |
| PQ duration (ms) | 182.1 ± 42.7 | 184.7 ± 25.0 | 0.400 |
| QRS duration (ms) | 94.1 ± 24.1 | 94.4 ± 19.7 | 0.714 |
| AV-block, n (%) | 11 (19.7%) | 4 (13.3%) | 0.550 |
| LBBB, n (%) | 5 (8.9%) | 2 (6.5%) | 1.000 |
| RBBB, n (%) | 3 (5.4%) | 3 (9.4%) | 0.664 |
| Variables . | No new PM . | New PM . | P value* . |
|---|---|---|---|
| Number, n (%) | 56 (63.6%) | 32 (36.4%) | |
| Age, year | 79.4 ± 8.0 | 80.7 ± 4.6 | 0.621 |
| Biplane LVEF (%) | 53.5 ± 14.5 | 57.8 ± 12.1 | 0.262 |
| β-Blockers (pre-operative) | 35 (62.5%) | 20 (62.5%) | 0.996 |
| Aortic valve area (cm2) | 0.56 ± 0.15 | 0.59 ± 0.17 | 0.652 |
| Aortic annulus dimension TTE (mm) | 23.2 ± 2.4 | 23.1 ± 2.0 | 0.810 |
| Interventricular septum (mm) | 14.2 ± 2.8 | 14.1 ± 2.4 | 0.769 |
| Peak pressure gradient (mmHg) | 73.6 ± 22.9 | 74.2 ± 24.7 | 0.953 |
| Mean pressure gradient, mmHg | 47.3 ± 14.9 | 49.1 ± 16.4 | 0.861 |
| Coronary heart disease, n (%) | 37 (67.3%) | 17 (53.1%) | 0.252 |
| Intra-operative | |||
| Peak pressure gradient CVP, mmHg | 16.7 ± 8.2 | 18.4 ± 6.1 | 0.148 |
| Mean pressure gradient CVP (mmHg) | 9.5 ± 5.2 | 9.9 ± 3.6 | 0.295 |
| Oversizing (mm) | 3.56 ± 2.02 | 4.19 ± 1.89 | 0.099 |
| Valve size (mm) | 26.6 ± 2.4 | 27.3 ± 2.1 | 0.187 |
| Re-dilation, n (%) | 12 (21.4%) | 7 (21.9%) | 1.000 |
| Valve-in-valve, n (%) | 2 (3.6%) | 1 (3.1%) | 1.000 |
| ECG characteristics | |||
| Ventricular rate | 77.4 ± 14.3 | 70.8 ± 14.5 | 0.034 |
| Sinus rhythm | 44 (78.6%) | 16 (50.0%) | 0.006 |
| Pre-operative atrial fibrillation | 12 (21.4%) | 16 (50.0%) | 0.006 |
| PQ duration (ms) | 182.1 ± 42.7 | 184.7 ± 25.0 | 0.400 |
| QRS duration (ms) | 94.1 ± 24.1 | 94.4 ± 19.7 | 0.714 |
| AV-block, n (%) | 11 (19.7%) | 4 (13.3%) | 0.550 |
| LBBB, n (%) | 5 (8.9%) | 2 (6.5%) | 1.000 |
| RBBB, n (%) | 3 (5.4%) | 3 (9.4%) | 0.664 |
*Mann–Whitney U or Fisher's exact test; LVEF, left ventricular ejection fraction; TTE, transthoracal echocardiography; LBBB, left bundle branch block; RBBB, right bundle branch block.
A total of 60 patients had pre-operative sinus rhythm and atrial fibrillation was present in the remaining 28.
Multivariate logistic regression predictors of post-operative PPM implantation are presented in Table 2 and graphically represented in Figure 1. Independent predictors were age [odds ratio (OR) 4.58, P = 0.023], valve oversizing more than 4 mm (OR 2.78, P = 0.032), valve size >26 mm (OR 2.17, P = 0.214), pre-operative atrial fibrillation (OR 5.21, P = 0.001), and pre-operative ventricular rate <65 b.p.m. (OR 2.91, P = 0.036). Multivariate analysis of predictors for PPM implantation during the first post-operative day showed an increased OR for ventricular rate <65 b.p.m. (OR 6.08, P = 0.137) and periprocedural AVB (OR 4.00, P = 0.046).
Multivariate logistic regression analysis for predictors of post-operative pacemaker implantation
| Variable . | P . | Odds ratio . | 95% confidence interval for odds ratio . |
|---|---|---|---|
| Age >75 years | 0.023 | 4.58 | 1.23–17.04 |
| Annulus dimension <23 mm | 0.313 | 0.63 | 0.26–1.55 |
| IVSH >17 mm | 0.842 | 0.86 | 0.20–3.71 |
| Oversizing, mm | 0.032 | 2.78 | 1.09–7.08 |
| Valve size | 0.214 | 2.17 | 0.64–7.33 |
| Re-operation | 0.493 | 0.70 | 0.25–1.94 |
| Re-dilation | 0.961 | 1.03 | 0.36–2.94 |
| Valve-in-valve | 0.912 | 0.87 | 0.08–10.00 |
| Pre-operative ECG characteristics | |||
| Sinus rhythm | 0.006 | 0.22 | 0.08–0.56 |
| Pre-operative atrial fibrillation | 0.006 | 5.21 | 1.97–13.82 |
| Heart frequency <65 b.p.m. | 0.036 | 2.91 | 1.07–7.86 |
| PQ >200 ms | 0.561 | 1.50 | 0.39–5.81 |
| QRS >100 ms | 0.397 | 0.63 | 0.22–1.83 |
| AV-block | 0.465 | 0.63 | 0.18–2.18 |
| LBBB | 0.685 | 0.70 | 0.13–3.86 |
| RBBB | 0.477 | 1.83 | 0.35–9.64 |
| Post-operative day 1 | |||
| Sinus rhythm | 0.005 | 0.24 | 0.09–0.65 |
| Atrial fibrillationa | 0.469 | 1.50 | 0.50–4.44 |
| High-grade AV-Block | 0.046 | 4.00 | 1.03–15.60 |
| Ventricular rate <65 b.p.m. | 0.137 | 6.08 | 1.71–21.56 |
| Variable . | P . | Odds ratio . | 95% confidence interval for odds ratio . |
|---|---|---|---|
| Age >75 years | 0.023 | 4.58 | 1.23–17.04 |
| Annulus dimension <23 mm | 0.313 | 0.63 | 0.26–1.55 |
| IVSH >17 mm | 0.842 | 0.86 | 0.20–3.71 |
| Oversizing, mm | 0.032 | 2.78 | 1.09–7.08 |
| Valve size | 0.214 | 2.17 | 0.64–7.33 |
| Re-operation | 0.493 | 0.70 | 0.25–1.94 |
| Re-dilation | 0.961 | 1.03 | 0.36–2.94 |
| Valve-in-valve | 0.912 | 0.87 | 0.08–10.00 |
| Pre-operative ECG characteristics | |||
| Sinus rhythm | 0.006 | 0.22 | 0.08–0.56 |
| Pre-operative atrial fibrillation | 0.006 | 5.21 | 1.97–13.82 |
| Heart frequency <65 b.p.m. | 0.036 | 2.91 | 1.07–7.86 |
| PQ >200 ms | 0.561 | 1.50 | 0.39–5.81 |
| QRS >100 ms | 0.397 | 0.63 | 0.22–1.83 |
| AV-block | 0.465 | 0.63 | 0.18–2.18 |
| LBBB | 0.685 | 0.70 | 0.13–3.86 |
| RBBB | 0.477 | 1.83 | 0.35–9.64 |
| Post-operative day 1 | |||
| Sinus rhythm | 0.005 | 0.24 | 0.09–0.65 |
| Atrial fibrillationa | 0.469 | 1.50 | 0.50–4.44 |
| High-grade AV-Block | 0.046 | 4.00 | 1.03–15.60 |
| Ventricular rate <65 b.p.m. | 0.137 | 6.08 | 1.71–21.56 |
A P value < 0.05 was considered significant. Odds ratio according to Cochran–Mantel–Haenszel test for the various predictors assessed.
IVSH, interventricular septal hypertrophy; LBBB, left bundle branch block; RBBB = right bundle branch block; AV, atrio-ventricular.
aAtrial fibrillation on ECG on the first post-operative day.
Multivariate logistic regression analysis for predictors of post-operative pacemaker implantation
| Variable . | P . | Odds ratio . | 95% confidence interval for odds ratio . |
|---|---|---|---|
| Age >75 years | 0.023 | 4.58 | 1.23–17.04 |
| Annulus dimension <23 mm | 0.313 | 0.63 | 0.26–1.55 |
| IVSH >17 mm | 0.842 | 0.86 | 0.20–3.71 |
| Oversizing, mm | 0.032 | 2.78 | 1.09–7.08 |
| Valve size | 0.214 | 2.17 | 0.64–7.33 |
| Re-operation | 0.493 | 0.70 | 0.25–1.94 |
| Re-dilation | 0.961 | 1.03 | 0.36–2.94 |
| Valve-in-valve | 0.912 | 0.87 | 0.08–10.00 |
| Pre-operative ECG characteristics | |||
| Sinus rhythm | 0.006 | 0.22 | 0.08–0.56 |
| Pre-operative atrial fibrillation | 0.006 | 5.21 | 1.97–13.82 |
| Heart frequency <65 b.p.m. | 0.036 | 2.91 | 1.07–7.86 |
| PQ >200 ms | 0.561 | 1.50 | 0.39–5.81 |
| QRS >100 ms | 0.397 | 0.63 | 0.22–1.83 |
| AV-block | 0.465 | 0.63 | 0.18–2.18 |
| LBBB | 0.685 | 0.70 | 0.13–3.86 |
| RBBB | 0.477 | 1.83 | 0.35–9.64 |
| Post-operative day 1 | |||
| Sinus rhythm | 0.005 | 0.24 | 0.09–0.65 |
| Atrial fibrillationa | 0.469 | 1.50 | 0.50–4.44 |
| High-grade AV-Block | 0.046 | 4.00 | 1.03–15.60 |
| Ventricular rate <65 b.p.m. | 0.137 | 6.08 | 1.71–21.56 |
| Variable . | P . | Odds ratio . | 95% confidence interval for odds ratio . |
|---|---|---|---|
| Age >75 years | 0.023 | 4.58 | 1.23–17.04 |
| Annulus dimension <23 mm | 0.313 | 0.63 | 0.26–1.55 |
| IVSH >17 mm | 0.842 | 0.86 | 0.20–3.71 |
| Oversizing, mm | 0.032 | 2.78 | 1.09–7.08 |
| Valve size | 0.214 | 2.17 | 0.64–7.33 |
| Re-operation | 0.493 | 0.70 | 0.25–1.94 |
| Re-dilation | 0.961 | 1.03 | 0.36–2.94 |
| Valve-in-valve | 0.912 | 0.87 | 0.08–10.00 |
| Pre-operative ECG characteristics | |||
| Sinus rhythm | 0.006 | 0.22 | 0.08–0.56 |
| Pre-operative atrial fibrillation | 0.006 | 5.21 | 1.97–13.82 |
| Heart frequency <65 b.p.m. | 0.036 | 2.91 | 1.07–7.86 |
| PQ >200 ms | 0.561 | 1.50 | 0.39–5.81 |
| QRS >100 ms | 0.397 | 0.63 | 0.22–1.83 |
| AV-block | 0.465 | 0.63 | 0.18–2.18 |
| LBBB | 0.685 | 0.70 | 0.13–3.86 |
| RBBB | 0.477 | 1.83 | 0.35–9.64 |
| Post-operative day 1 | |||
| Sinus rhythm | 0.005 | 0.24 | 0.09–0.65 |
| Atrial fibrillationa | 0.469 | 1.50 | 0.50–4.44 |
| High-grade AV-Block | 0.046 | 4.00 | 1.03–15.60 |
| Ventricular rate <65 b.p.m. | 0.137 | 6.08 | 1.71–21.56 |
A P value < 0.05 was considered significant. Odds ratio according to Cochran–Mantel–Haenszel test for the various predictors assessed.
IVSH, interventricular septal hypertrophy; LBBB, left bundle branch block; RBBB = right bundle branch block; AV, atrio-ventricular.
aAtrial fibrillation on ECG on the first post-operative day.
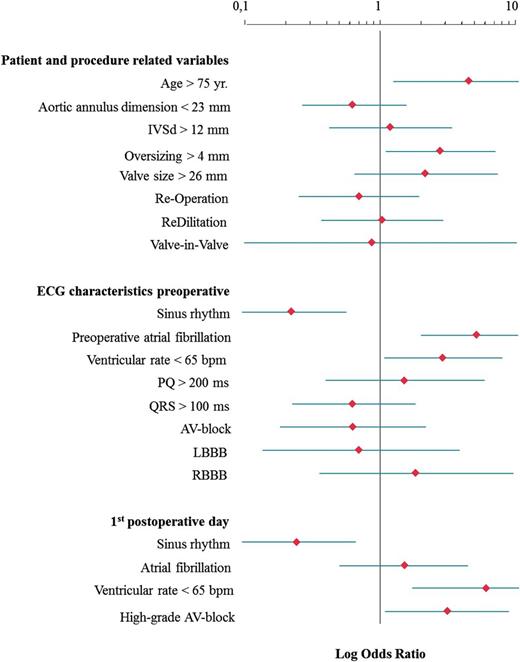
Multivariate logistic regression analysis of predictors for permanent pacemaker implantation post-transfemoral CoreValve implantation; IVSd, interventricular septal thickness at diastole; LBBB, left bundle branch block; RBBB, right bundle branch block; AV, atrio-ventricular.
Discussion
TAVI for severe AS in patients with multiple co-morbidities has now become a common procedure in patients who are at high risk for conventional aortic valve replacement (AVR). Although TAVI has many advantages, increasing experience with this treatment has also revealed a number of risks and complications. A group from the Netherlands recently analysed the occurrence of in-hospital complications after TAVI with the CVP according to the Valve Academic Research Consortium criteria and observed one or more complications in 51% of patients. In addition, such patients were observed to have a prolonged length of stay in hospital.9
Along with annular rupture, inadvertent coronary artery occlusion and aortic dissection, the development of high-grade AVB with bradycardia is also a serious and sometimes life-threatening complication. We performed the current study in order to more clearly define risk factors for post-operative PPM implantation in patients undergoing transfemoral CVP implantation.
The incidence for PPM after conventional surgical AVR has been reported to be as high as 6%.10–12 Known risk factors for PPM after surgical AVR include pre-operative conduction system disease,12,13 pre-operative aortic valve regurgitation and history of myocardial infarction.10,14 In contrast, pacemaker implantation rates post-TAVI are higher than post-conventional AVR. Depending on the implanted prosthesis, the reported need for PPM after TAVI ranges between 4 and 12% for the Edwards Sapien prosthesis (Edwards LifeSciences, Irvine, CA, USA)15,16 and 5.7–50% for the CVP.6,17–19 The higher pacemaker rate associated with the CVP device is probably due to its length, with contact between the self-expanding nitinol stent and the sub-aortic conduction pathway being unavoidable during valve deployment. Guetta et al. observed a high grade AVB necessitating PPM implantation in 40% of patients undergoing TAVI with CVP. Independent risk factors for PPM were pre-operative RBBB and low valve implantation, defined as >6 mm from the lower edge of the non-coronary cusp to the ventricular end of the prosthesis.20
Our retrospective analysis revealed an incidence of PPM implantation of 36.4%, well within the reported range for transfemoral CVP implantations. There were no significant differences in pre-operative variables between patients requiring post-procedure PPM and those who did not, with the exception of a lower baseline ventricular rate in PPM patients. With regard to intra-procedure variables, we observed a significant difference regarding prosthesis diameter and oversizing of the valve with PPM patients receiving larger CVP prostheses and more oversizing. These findings were similar to the observations of Bleiziffer et al.21 In contrast to Jilaihawi et al.,18 we found no difference in septal hypertrophy between the two groups both by univariate and multivariate analysis.
Our multivariate analysis revealed age older than 75 years (OR 4.58), pre-operative atrial fibrillation (OR 5.2), and pre-operative ventricular rate <65 b.p.m. (OR 2.9) as significant pre-operative predictors of post-procedure PPM requirement. Additionally, oversizing of the prosthesis >4 mm (OR 2.78) and implantation of a prosthesis larger than 26 mm (OR 2.17) were intra-operative independent risk factors.
Surprisingly, re-dilation after CVP implantation had no effect on the requirement for PPM. The reason for this observation might be the relatively short time period where the aortic annulus was exposed to high pressure from repeat valvuloplasty. In juxtaposition to this short period of high pressure, the long nitinol frame of the CVP applies a long-standing, increased pressure to the annulus, the fibrous skeleton, the interventricular septum, and the structures of the conduction system.22 This continuous frame expansion pressure, in combination with large calcium formations that can be found in the non-coronary cusp and in the intra-ventricular septum, may be the reason for the higher PPM rate observed after CVP implantation when compared to other prostheses. The frame of the Edwards Sapien valve, for example, is a stainless steel, balloon expandable stent which is ∼50 mm shorter than the stent of the CV prosthesis. Additionally the CV prosthesis is intended to be implanted deeper in the left ventricular outflow tract, which has been shown to be an independent risk factor for PPM.5 The shorter frame and the higher device landing zone of the Edwards Sapien prosthesis should be an advantage regarding the development of injury of the conduction system.
CVP oversizing may also lead to subsequent damage to the conduction system for the same reasons discussed above. Our multivariate analysis showed an increased risk of PPM implantation for oversizing >4 mm. Bleiziffer et al.21 also described this problem, but concluded that, in cases of borderline annulus dimensions, a larger prosthesis should be implanted in order to avoid the development of paravalvular leaks. Since aortic valve regurgitation has also been indentified as an independent risk factor for AVB and given the negative influence of acute aortic regurgitation on patient haemodynamics, we also recommend the implantation of the larger prosthesis in this clinical situation.10,12,23 However, such an approach should also lead to a heightened awareness for possible PPM requirement post-procedure.
Different authors described the influence of RBBB on the need for PPM.12,13,15 Our study revealed no statistically significant effect of pre-operative RBBB on univariate analysis, but a slight increased risk for PPM on multivariate analysis (OR 1.83) was demonstrable.
With regard to minimizing the risk of post-procedure PPM implantation, pre-operative CT might be helpful to assess the presence of extensive calcium in the non-coronary cusp and the interventricular septum. Such patients may benefit from the implantation of another transcutaneous device, rather than a CVP. With the ability to more accurately quantify the calcification of the aortic valve and surrounding structures, a prediction of secondary manoeuvres after device implantation, such as re-dilation, may be possible.24–26 Additionally, if patients develop AVB within 24 h after CVP implantation, the risk for PPM increases four-fold in our study population and six-fold in the case of a ventricular rate <65 b.p.m. In our opinion, continuous ECG should be performed for 5 days post-procedure, because the mean time from implantation to problem was in our study population was 2.8 ± 4.1 days. The additional costs of continuous post-procedure telemetry need to be weighed against the risk of possible delayed presentation of serious conduction disturbances.
Conclusion
PPM implantation following transfemoral CVP implantation is a frequent complication. Advanced patient age, pre-operative atrial fibrillation, pre-operative ventricular rate <65 b.p.m., prosthesis oversizing >4 mm and the use of a prosthesis larger than 26 mm are independent risk factors for this complication. The development of a periprocedural high-grade AVB increases the risk for PPM four-fold, and a post-procedure ventricular rate <65 b.p.m. ∼six-fold.
Limitations
There are several limitations to our study. The presented data are a single centre experience with a relatively small sample size, but the number of adverse events (i.e. PPM implantation) was large enough to perform meaningful analyses. In addition, our data are comparable with other publications on this topic. Another weakness of our study is that the indications for early PPM implantation after occurrence of conduction system disease are not universally accepted. In this population of patients with severe co-morbidities, however, we opted for a relatively aggressive PPM implantation approach in order to avoid possible catastrophic haemodynamic instability.
Conflict of interest: none declared.



